13
Radiographic Considerations during the Endodontic Treatment
Introduction
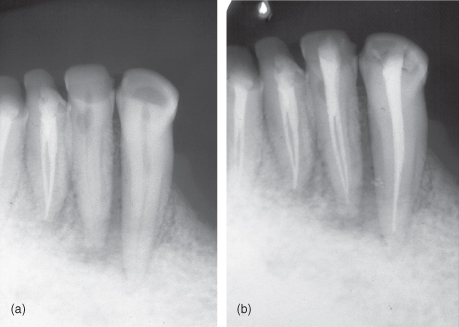
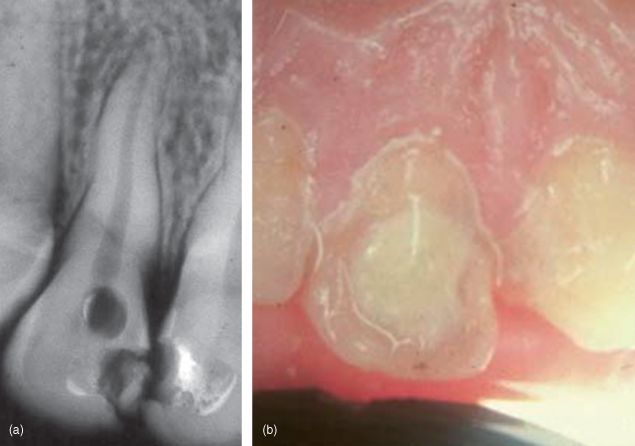
Radiology is an indispensable tool in the clinical practice of endodontics because most structures harboring disease are not visible to the naked eye. As a result, radiographs are needed during several aspects of the treatment, and their proper interpretation and analysis is crucial to the establishment of a favorable outcome (Torabinejad and Walton, 2009) (Figure 13.1A,B).
Figure 13.1 (a and b) The radiographs contain more information than can readily be seen by the naked eye. Noticeable in this retreatment case is the complex anatomy of the lateral incisor
(Courtesy of Dr G. Yared).
Standard two-dimensional radiographs used for the management of endodontic problems yield limited information because the images produced often are accompanied by geometric distortion and anatomical noise. Goldman et al. (1972), in his classic paper, mentioned that radiographs are not so much read as interpreted and that this process can be ambiguous and inconsistent. Dentists are always asking: is there an area of radiolucency? How large is the area? Where is the apex of the tooth? (Figure 13.2).
Figure 13.2 This radiograph shows an apical and lateral rarefaction. Accurate interpretation of these areas is essential for correct diagnosis.

In endodontics, radiographs are essential in diagnosis, treatment planning, treatment procedures, prognosis, follow-up, legal documentation, and education. In this chapter, the art of interpreting everyday radiographs will be explained in detail. (Note that through this chapter, the term “radiographs” will suggest conventional receptors as well as digital sensors.)
Diagnosis
Radiographs are important, if not the most important, tools available to the clinician; and they help identify the problem–the tooth–and help develop the treatment plan. At least one current preoperative radiograph taken using the paralleling technique is mandatory in identifying the presence and nature of pathosis.
Some common rules are important to follow when radiographs are used to assess diagnosis: If the tooth in question is fully mature and vital and your diagnostic testing reveals an irreversible pulpitis, no significant changes may be apparent on the radiograph. Teeth with necrotic pulps do not routinely have rarefactions associated with their roots, and apical rarefactions of pulpal origin will routinely demonstrate the loss of the apical lamina dura in association with the rarefaction (Figure 13.3) (Gutmann et al., 1992).
Figure 13.3 Radiograph showing the lost of the lamina dura at the apex, indicating pulp pathosis.

From the clinical point of view, it is important to remember that necrosis can sometimes be seen by the naked eye. In other words, when a crown that we “see” is discolored, it may be an indication of pulpal necrosis; or when we “see” a sinus track on the gingiva, it may indicate the presence of infection originating from a necrotic pulp. By the same standard, an apical rarefaction that we “see” radiographically may indicate necrosis. While patients demonstrating the clinical signs of irreversible pulpitis may not show demonstrable radiographic changes, the radiograph does have the potential to show etiological contributing factors, such as caries or a deep restoration. Establishing a diagnosis in cases such as this can at times be more challenging.
During the diagnostic procedures, it is crucial to assess tooth restorability. Radiographs are also helpful in assessing and in explaining to the patient the risks and benefits of the proposed treatment.
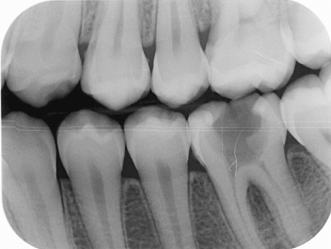
The preoperative (or diagnositc) radiograph should also be used to assess the root canal anatomy, and the difficulty of the case should be evaluated. A supplemental bite-wing (Figure 13.4) radiograph is useful to detect caries, to determine the depth of a calcified pulp chamber, or to reveal a pulp chamber obscured by a large radiopaque restoration. A second periapical radiograph taken at a different horizontal projection is also helpful in determining the number and shape of the roots when multirooted teeth are involved.
Figure 13.4 Bite-wing radiograph can be taken as a complimentary diagnosis aid.
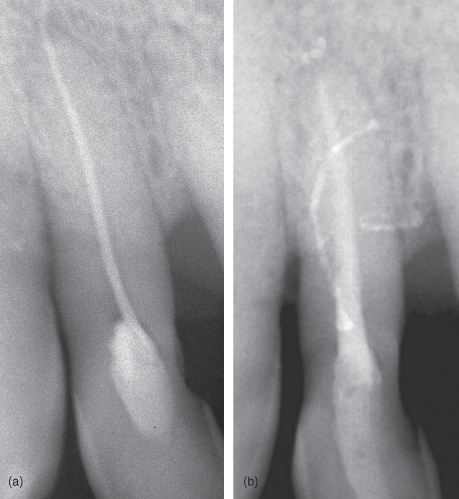
When a sinus track or fistula is present (Figure 13.5A,B), it can sometimes be traced back to an area of pathosis. This is accomplished by threading a new gutta-percha cone (size 30 or 40) through the track and exposing a periapical radiograph. Generally, it is not necessary to anesthetize during this step. If the sinus track cannot be penetrated with a gutta-percha point, it may be necessary to reopen it with an explorer tip or periodontal probe and then introduce a new cone.
Figure 13.5 (a and b) Sinus track traced with a gutta percha cone.
The clinician must realize that periradicular pathosis and/or bone destruction may be present, but not radiographically visible. Radiographic bone loss is not evident until there is significant erosion of the cortical plate (Bender and Seltzer, 2003) (Figure 13.6A,B).
Figure 13.6 (a and b) Radiograph showing maxillary lateral incisor with an acute abscess with minimal bone destruction.
There are some limitations of conventional radiography for endodontic diagnosis (Patel et al., 2009). The most important one is the loss of three-dimensional anatomy: Conventional images compress three-dimensional anatomy into a two-dimensional image or shadowgraph, greatly limiting diagnostic performance (Webber and Messura, 1999). Important features of the tooth and its surrounding tissues are visualized in the mesiodistal (proximal) direction only. Similar features presenting in the buccolingual plane (i.e., the third dimension) may not be fully appreciated.
On occasions, deliberate and controlled alteration of the radiation geometry can be beneficial and provide additional information not always visible on images taken with standard angulations. For example,
Figure 13.7 (a) Anatomical superimposition. Superimposition of the nasopalatine foramen. Tooth roots change position more than foramen with changes in direction of central ray
(Courtesy of Dr. C. Torneck).
(b) Anatomical superimposition with mental foramen. Being buccal to the tooth roots, the mental foramen will move more in the direction of the change in the direction of the central ray than the teeth
(Courtesy of Dr. C. Torneck).
Preoperative Radiograph and Anatomy
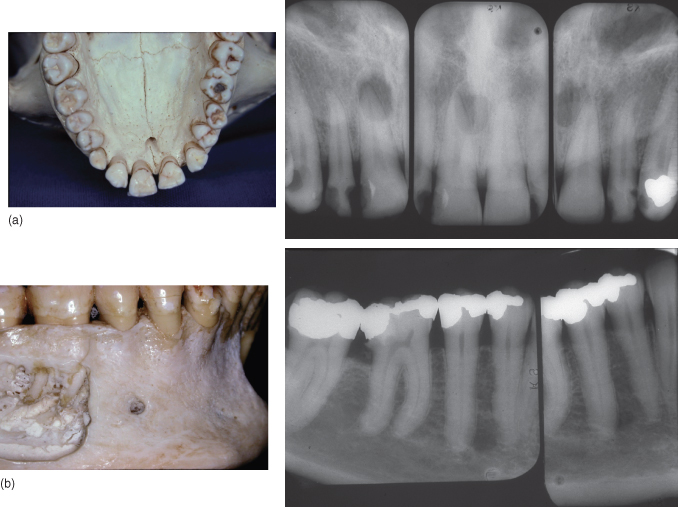
During the preoperative steps, it is important to analyze and categorize the tooth with the different degree of difficulty (average, moderate, or high risk) (form adapted from the risks and difficulty form used by the University of Toronto) (Table 13.1). A special consideration and analysis should be given to the radiographic consideration of the canal(s). The following points need to be examined:
- Angle of curvature: There are many techniques to evaluate the canal curvature. The first and most common method was reported by Schneider in 1971. The degree of canal curvature was defined as the acute angle between the long axis of the canal and a line from the point of initial curvature to the apical foramen. In 1982, Weine proposed another method that defined the angle of curvature differently. The acute angle between lines passing through the apical and coronal portions was measured. Pruett et al. (1997) pointed out that the shape of any root canal curvature could be more accurately described by using two parameters, angle of curvature and radius of curvature (Gu et al., 2010).
- Radius of curvature: The radius is defined as the length of a line segment between the center and circumference of a circle or sphere and represents the abruptness of curvature. The shorter the radius, the more abrupt the curvature (Figure 13.8A,B).
- Distance: From the start of the curvature to the apex: The smaller the distance, the more abrupt the curvature.
- Number of canals:
- When a radiograph reveals a root canal space that is not at the center of the root, an extra canal should be suspected. If there is only one canal, it will appear in the center of the root regardless of the angulations (Figure 13.9).
- In a single rooted tooth, a sharp or rapid change in the visible density of the root canal space usually indicates that one large canal that has split into two canals (Figure 13.10) (Gutmann et al., 1992).
- If a rapid change in density occurs in the apical third of the root, it is possible that the canal exists on the buccal or lingual surface of the root (Figure 13.11A–D) (Gutmann et al., 1992).
Table 13.1 Analysis of endodontic case difficulty and risk
(Adapted from the risks and difficulty form used by the University of Toronto).
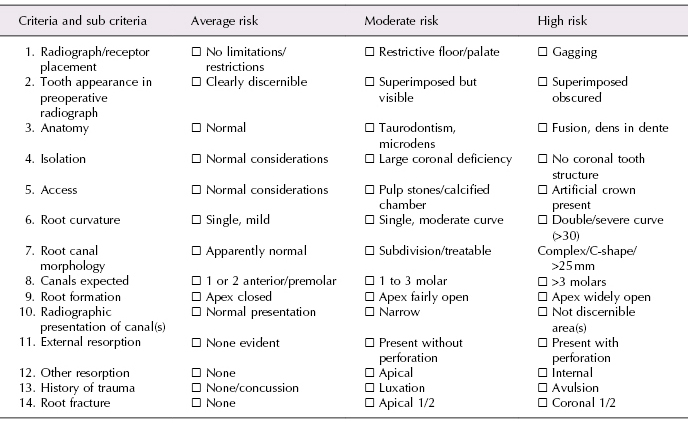
Figure 13.8 (a and b) Image showing different radius of curvatures. The shorter the radius, the more abrupt the curvature is.
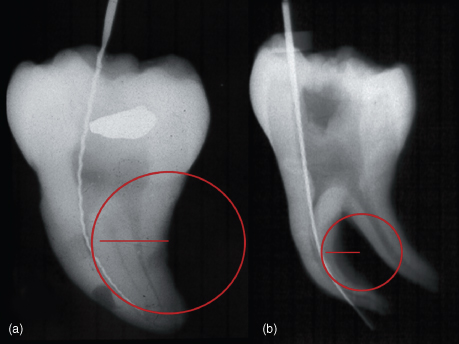
Figure 13.9 (a and b) Radiograph reveals a root canal space that is not at the center of the root. Therefore, an extra canal should be suspected
(Courtesy of Dr. Hilu).
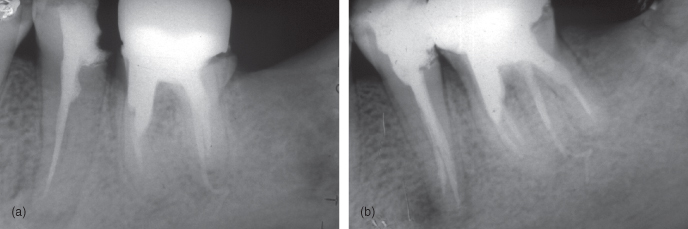
Figure 13.10 Changes in the radiolucency of the canals indicates that the canals may split in two.
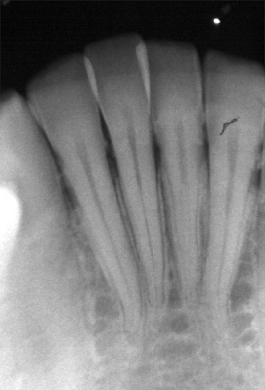
Figure 13.11 (a–d) Rapid change in density occurs in the apical third of the root; it is possible that the canal exists on the buccal.

Radiographs and Different Teeth Groups (Hargreaves and Cohen, 2011)
Maxillary Central Incisor
The root canal system outline of this tooth reflects the external surface outline. It is the only tooth where the mesial-distal dimension and the buccal-lingual dimension are similar.
Maxillary Lateral Incisor
This tooth is wider mesiodistally than buccolingually. The probability of a sharp apical curvature is high. Buccal or lingual root curvature is not visible on the standard (direct) view. Changing the horizontal angulation will allow this common occurrence to be identified, although such images are often poorly defined. Buccal curves move in the opposite direction to the angulation of the beam; a mesial angulation will produce a movement of the root apex toward the distal aspect. Lingual curves will move toward the direction of angulation. When identification of root curvature is critical, such as when surgery is planned, or when the precise location of canal irregularities or fractured instruments is required, the use of the triangular scanning technique (Bramante et al., 1980) can be beneficial (explained in detail in Chapter 2), as visualization of the opposite maxillary lateral incisor can also give some information on the anatomy, given that teeth are usually symmetric (Torabinejad and Walton, 2009).
Maxillary Canine
The root canal system is similar to that of the maxillary incisor. It is wider labiolingually than mesiodistally. The average length is 26.5 mm. This is the longest tooth in the mouth. It can be problematic to visualize the apex in the radiograph. By increasing the vertical angulation of the X-ray tube, it may help foreshorten the root and give a more accurate idea of the periodontal ligament space, lamina dura, and the end of the root.
First Maxillary Premolars
The majority of the first premolars have two canals located in the buccal and lingual surfaces. Changing 20 degrees on the horizontal projection has great value to separate the two canals.
Maxillary Molars
Maxillary first molar is one of the most complex in root canal anatomy, making it very difficult and challenging to treat. A major reason is associated with radiography. The frequent superimposition of portions of the other roots on each other, superimposition of bony structure (such as sinus floor or zygomatic process) on root structures, and shape and depth of the palate can obstruct the visualization of the roots. This problem can be solved by proper changes in the angulation of the root. On many occasions, and particularly when using the bisecting angle technique, superimposition of the zygomatic process of the maxilla over the root apices of molar teeth occurs, resulting in the characteristic arch-like radiopacity which hinders radiographic interpretation. To lessen this imaging difficulty, modification by decreasing the vertical angulation can be considered. In addition, when using the bisecting angle technique, the vertical orientation of the receptor is dictated by the local anatomy. So in situations where the receptor forms an angle with the long axis of the teeth, most commonly occurring in the palatal arch of the maxilla, placement of a cotton roll will help the positioning of the receptor. Alternatively, a film holder that positions the receptor in a parallel orientation to the teeth and guides the X-ray beam (e.g., Rinn holder) can be used to minimize this anatomical obstruction. (Special radiographic techniques are explained in detail in Chapter 2.)
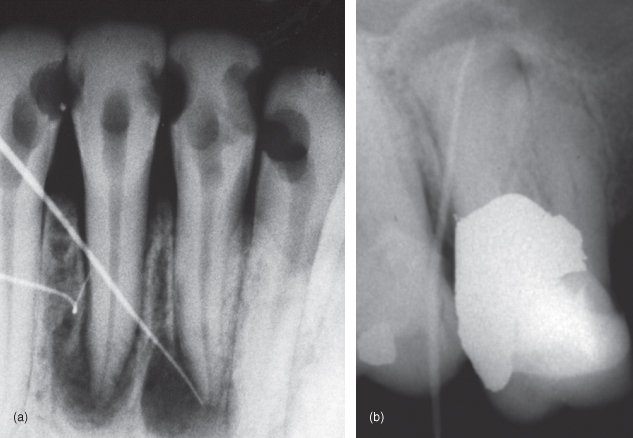
Lower Central and Lateral Incisors
The mandibular incisors, because of their small size and internal anatomy, may be the most difficult to access and prepare. The possibility of second canals is high (around 40%). The canal found first after access will always be the buccal canal, therefore the access needs to be extended toward the lingual to find the second canal. Changing the horizontal angulation separates the canals and allows their identification (Figure 13.12A,B).
Mandibular Canines
The root canal system is very similar to that of the maxillary canine, except that the dimensions are smaller. The root canal outlines are narrower in the mesial-distal dimensions but usually very broad buccolingually. Occasionally, they may have two roots, located in buccal and lingual surfaces.
/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses