13
Anomalies of tooth formation and eruption
P.J.M. Crawford and M.J. Aldred
Chapter contents
13.4 Abnormality of tooth size
13.5 Abnormality of tooth form
13.5.1 Abnormality of crown form
13.7 Abnormality of tooth structure
13.9 Disturbances of exfoliation
13.1 Introduction
Both the primary and permanent dentitions may be affected by variations in the number, size, and form of the teeth, as well as the structure of the dental hard tissues. These variations may be exclusively genetically determined, brought about by either local or systemically acting environmental factors, or possibly a combination of both genetic and environmental factors acting together. The same interplay of influences may affect the eruption and exfoliation of primary teeth, as well as the eruption of permanent teeth. This chapter considers a range of conditions involving abnormalities of the number, size, form, and structure of teeth and their eruption.
It is important to be aware of the psychosocial aspect when meeting children and families affected by these conditions. We have too often heard stories of social isolation of even very young children as a result of their missing or discoloured teeth. In the case of discoloured teeth, parents have told us that they have been taken to task by other adults for not looking after their child’s teeth when the discolouration was intrinsic and unavoidable. Society’s preoccupation with ‘the perfect smile’ seems to increase and, in a world where employment opportunities are at a premium, children denied access to dental aesthetic adjustment may be genuinely disadvantaged.
While investigating inherited conditions, it is important to enquire of both sides of the family tree equally. Not only does this ensure that the investigation is complete, but also it may help to alleviate any sense of ‘guilt’ felt by an affected parent.
Wherever possible, we try to avoid the use of the word ‘normal’ in our clinical care, although the word will be used in this text. The vast majority of children with these conditions want to become ‘one of the crowd’. Thus we would speak, when offering restorative treatment for example, of making a smile ‘ordinary’ or ‘boring’. We have found this approach successful in our practices; our readers may choose this or one of many other approaches in order to further the care of these children.
We have been questioned repeatedly about the possibility of genetic treatment for some of these inherited conditions. We are not aware of any progress in this direction at present.
13.2 Missing teeth
Hypodontia is the term most often applied to a situation where a patient has missing teeth as a result of their failure of development. Anodontia describes the total lack of teeth of one or both dentitions. Oligodontia is a term used to describe a situation where multiple (usually more than six) teeth are missing.
13.2.1 Prevalence
In the primary dentition, missing teeth occur more commonly in the maxilla and typically the maxillary lateral incisor is the tooth involved. Various studies have shown the prevalence of missing primary teeth to be between 0.1% and 0.9% of Caucasian populations, with males and females affected equally. Developmentally missing permanent teeth are seen in both the maxilla and mandible (Fig. 13.1). In Caucasian populations the third molars are the most common missing teeth, followed by the mandibular second premolar, the maxillary lateral incisor, and then the maxillary second premolar. A female-to-male ratio of 4:1 has been reported. Missing third molars occur in 9–30% of individuals. If the third molars are excluded, the prevalence in the permanent dentition varies between 3.5% and 6.5% according to the study quoted. (See Key Points 13.1.)
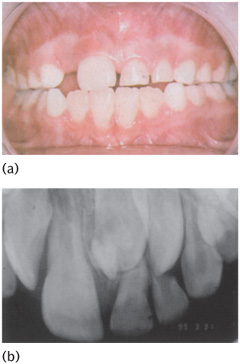
Figure 13.1 Hypodontia, absent 41, retained 81.
13.2.2 Aetiology
The cause of an isolated developmentally missing tooth is often unclear; this is most likely to be genetic in origin. Rarely, it may be a consequence of some environmental insult during development. Missing teeth have been reported in association with multiple births, low birth weight, and increased maternal age. Rubella and thalidomide embryopathies may also be associated with missing teeth.
Single-gene disorders have been associated with missing teeth. Multiple missing teeth, as well as teeth with small crowns, may be seen in a number of syndromes including X-linked hypohidrotic ectodermal dysplasia (Fig. 13.2), autosomal dominant and autosomal recessive cases of ectodermal dysplasia, and autosomal recessive chondroectodermal dysplasia (Ellis–van Creveld syndrome). Down syndrome (trisomy 21) is also associated with hypodontia.
Hypodontia and microdontia involving the maxillary lateral incisor occur in clefts involving the lip and palate. X-linked hypohidrotic ectodermal dysplasia is characterized in males by thin sparse hair, dry skin, absence of sweating (and therefore heat intolerance), and multiple missing teeth. These children are at risk because of their inability to cool themselves and may die of hyperthermia in infancy if undiagnosed. This condition, while rare, is of particular importance as the dental professional may be the first to come to a diagnosis, and thus introduce families to support mechanisms. In heterozygous females the changes are milder and may be restricted to the teeth, although a distinctive facial profile (slight retrusion of the maxilla) may be recognized. Most commonly, one or both maxillary lateral incisors and/or the second premolars are missing. In some patients one or both of the maxillary lateral incisors may be of peg form. The responsible gene is the ED1 gene on the X chromosome which encodes the protein ectodysplasin-A.
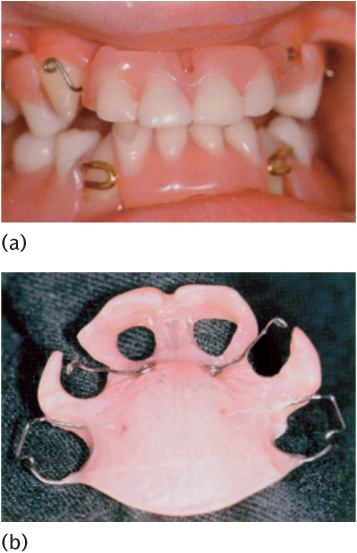
Figure 13.2 Hypohidrotic ectodermal dysplasia: erupted permanent teeth.
Figure 13.3 Median maxillary central incisor syndrome.
Figure 13.4 a) Hypohidrotic ectodermal dysplasia: (b) erupted permanent teeth masked by a ‘porthole’ denture with canine retractors during eruption.
Autosomal dominant inheritance of missing teeth is seen in families with mutations in the MSX1 gene on chromosome 4. Missing third molars and second premolars are the most common finding. These families may also have clefting segregating with the missing teeth. Mutations in the MSX1 gene are also seen in the tooth-nail (Witkop) syndrome.
A pattern of autosomally dominant inheritance of missing teeth, particularly molars, is seen as a result of mutations in the PAX9 gene on chromosome 14.
Some patients with a solitary median maxillary central incisor in combination with other developmental defects have been found to have mutations in the sonic hedgehog (SHH) gene on chromosome 7 (Fig. 13.3).
13.2.3 Treatment
The care of children with multiple missing teeth can be complex and ideally requires multidisciplinary input from paediatric dentists, orthodontists, and prosthodontists, as well as genetic counselling. Active repeated preventive input and support is essential, and the general practitioner has a large part to play in the underpinning care of these children. Missing teeth and small teeth often present together, and so masking conical or similarly distinctive teeth with composite is strongly advised. This is possible from a very early age and can be made easier by using laboratory-made composite ‘onlay crowns’ cemented with flowable composite. In cases of anodontia, full dentures are required. These can be provided, albeit with likely limited success, from about 3 years of age, with the possibility of implant support for prostheses provided in adulthood (Fig. 13.4). Multiple missing teeth can be treated using partial dentures, with implants as part of the treatment protocol at a later age. Implant placement is best left until skeletal maturity. Dentures will need to be replaced as the jaws grow; ‘holes’ may have to be provided within the denture base for teeth to erupt through, thereby masking their form until an appropriate time for crown modification. Progressive provision of dentures with annual replacements during the school holidays (the long vacation), mimicking the developing dentition at the child’s age, can do much to minimize the stigma of these conditions. Although, ultimately, dentures can be retained by implants, the lack of development of the alveolar bone may prove to be a limiting factor.
13.3 Extra teeth
Extra teeth (supernumerary teeth) have been reported to occur in 0.2–0.8% of Caucasians in the primary dentition and 1.5–3.5% in the permanent dentition in the same populations. There is a male-to-female ratio of approximately 2:1. Patients with supernumerary primary teeth have a 30–50% chance of these being followed by supernumerary permanent teeth. Teeth that resemble those of the normal series are referred to as supplemental teeth (Fig. 13.5) while those of less typical, often reduced, form—sometimes further described as tuberculate or conical—may be termed accessory supernumerary teeth.
Supernumerary teeth are most often located in the anterior maxilla in or immediately adjacent to the midline, and are then referred to as a mesiodens. Supernumerary teeth in the molar regions adjacent or distal to the normal sequence of teeth are referred to as paramolars or distomolars, respectively. In some cases the supernumerary teeth may be an odontome.
Supernumerary teeth are more common in the maxilla than in the mandible, with a ratio of about 5:1. Apart from those in the midline, they may be present bilaterally and symmetrically; hence the presence of a supernumerary in one part of the jaw should lead to consideration of further supernumeraries elsewhere. Supernumerary teeth may fail to erupt and may delay eruption of a permanent tooth which is developing deeper within the jaw. This commonly occurs in the case of a mesiodens (Fig. 13.6).
There is a significant association between supernumerary teeth and invaginated teeth (see Section 13.5.3). There is also an association with palatal clefts, with approximately 40% of patients with a cleft of the anterior palate having supernumerary teeth.
Multiple supernumerary teeth are seen in cleidocranial dysplasia as well as in other syndromes such as oral–facial–digital syndrome type 1 and Gardner syndrome. The management of supernumerary teeth is discussed in Chapter 14. (See Key Points 13.2.)
13.4 Abnormality of tooth size
13.4.1 Crown size
There is a degree of subjectivity regarding what constitutes normal (‘ordinary’) tooth size (and shape). Teeth which are obviously larger than normal are referred to as megadont or macrodont, whereas teeth which are smaller than normal are termed microdont. Crown size is often related to root size, so teeth with large crowns often have large (broad) roots, while teeth with small crowns tend to have small (slender) roots. Microdontia can be associated with hypodontia, as in the example of X-linked hypohidrotic ectodermal dysplasia where a heterozygous female might have one missing lateral incisor and a peg-shaped crown of the contralateral maxillary lateral incisor (Fig. 13.7).
Figure 13.5 Supplemental tooth 12.
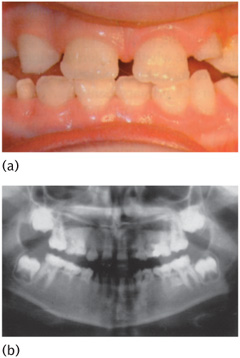
Figure 13.6 (a) Clinical and (b) radiographic views of a supernumerary tooth delaying the exfoliation of teeth 61 and 62, and the eruption of tooth 21.
Megadont teeth
Megadont maxillary incisors can occur as a result of fusion of adjacent tooth-germs or as a result of an attempt at separation of a single tooth-germ to form two separate teeth (gemination). To determine which of these possibilities has occurred, it is necessary to count the number of teeth—in fusion there will be a reduced number of teeth, and in gemination there will be a normal number with one larger tooth or an increased number if the division of the one tooth-germ into two is complete. The permanent maxillary central incisors are most often affected (Fig. 13.8) followed by the mandibular second premolars. Isolated megadontia in the permanent dentition has been estimated to occur in approximately 1% of patients. The condition may be symmetrical. Generalized megadontia has been reported in association with pituitary gigantism, unilateral facial hyperplasia, and hereditary gingival fibromatosis.
Figure 13.7 Hypodontia concurrent with microdontia.
Figure 13.8 Megadont tooth 11, absent tooth 12.
Figure 13.9 Isolated microdontia affecting 22 in a female. The gingival architecture is suggestive of occult cleft.
Microdontia
Microdont primary teeth are uncommon, with a reported prevalence of 0.2–0.5%. In the permanent dentition the prevalence is approximately 2.5% for individual teeth, with generalized microdontia occurring in approximately 0.2% of individuals. Females are more often affected than males, with the maxillary lateral incisor being most commonly affected, having a peg-shaped or conical crown (Fig. 13.9). As noted in Section 13.2, there is an association between microdontia and hypodontia.
13.4.2 Root size
Root length appears to be subject to some racial variation, with shorter roots being seen in people of Oriental background and larger roots in patients of African origin.
Large root size
Larger than normal roots are most typically seen affecting the permanent maxillary central incisors, with a population prevalence in one Swedish study of 2.3%. Males were four times more likely to be affected than females.
Small root size
Short-rooted teeth in the primary dentition may be associated with other dental abnormalities. Short roots may also be seen in a number of conditions affecting the dentine and/or pulp. These will be considered in a later section.
Short roots may be seen affecting the permanent maxillary central incisors. The shortening affects approximately 2.5% of children and some 15% of these may have shortened roots on other teeth, most often premolars and/or canines. The cause is often unknown, although it can occur as a result of orthodontic treatment.
In regional odontodysplasia (Section 13.7.1) there is typically abnormal root formation as well as abnormalities of the crowns of the teeth.
Irradiation of the jaws or chemotherapy during the period of root formation may lead to truncation of roots which were developing at the time of treatment (Fig. 13.10).
13.4.3 Treatment
As with hypodontia, the active cooperation of paediatric dentist, orthodontist, and restorative dentist should be encouraged to optimize treatment planning for young people affected by these conditions from an early age.
A megadont maxillary central incisor can be cosmetically unaesthetic and treatment decisions may need to be considered soon after (or, in some cases, before) eruption of the tooth. The options include acceptance, remodelling of the tooth, extraction of the tooth with orthodontic treatment if necessary, and subsequent masking of the space with a bridge, denture, or implant (Fig. 13.11).
Figure 13.10 (a) Clinical and (b) radiographic views showing disturbed dental development following chemotherapy for leukaemia.
A microdont tooth, particularly if this affects the maxillary lateral incisors, can be modified by the addition of acid-etch composite material to the tooth to reproduce the typical contours of the crown (Fig. 13.12). In adult life, porcelain veneers may also be used or the tooth can be crowned. However, the continued use of composite has the benefit of minimal tooth preparation and delay of the start of the ‘restorative cycle’ with its ultimate end in the loss of the tooth.
Figure 13.11 Megadont tooth 11. Minimal adjustment of tooth form 11, 13, from its original state in Fig. 13.8.
Figure 13.12 Isolated microdontia affecting 22 in a female. Restored with composite.
13.5 Abnormality of tooth form
13.5.1 Abnormality of crown form
Fusion and gemination
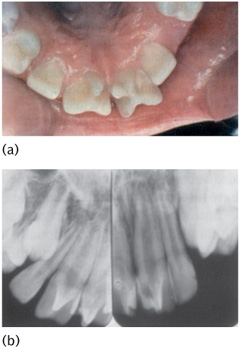
Some cases of megadont crowns are due to fusion of adjacent tooth-germs (fusion) or attempts at developmental separation of a single tooth-germ to produce two separate teeth (gemination), and a variety of terms have been used for such situations. The term ‘double teeth’ has been applied to cover both situations. It is necessary to count the number of teeth present clinically and with the aid of radiographs determine whether fusion or gemination has occurred. The prevalence of such abnormalities in the primary dentition ranges from 0.5% to 1.6% of Caucasian populations studied. The permanent dentition is less commonly affected (prevalence 0.1–0.2%). Males and females are affected equally. A genetic basis has been suggested, but not confirmed.
The clinical manifestation may vary from a minor notch on the incisal edge of an abnormally wide incisor crown to two separate crowns with a single root. The crowns and root may be in continuity along their entire length or may be almost separate; some pulp intercommunication is often present. The most typical areas affected are the anterior segments of the arches in the primary dentition, with the mandible more commonly affected than the maxilla (Fig. 13.13). There may be an association with hypodontia, so that a larger than normal tooth of the primary series together with a missing tooth in that series may represent an intermediate stage between the presence or absence of a tooth.
Physiological root resorption of primary fused or geminated teeth may be delayed and this may lead to delayed eruption of the permanent successors.
Treatment
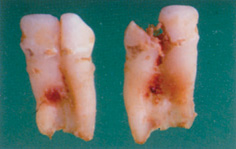
When this condition affects the primary dentition no treatment per se is required. However, it is important to consider the possibility of abnormalities of the number and/or form of the permanent dentition in the area. One problem which can occur is that caries can develop at the interface between the two crown segments (Fig. 13.14). This can be prevented by an etch-retained sealant before any decay has occurred, or a similar restoration to fill in the defect, which will also improve the cosmetic appearance. In the permanent dentition, the final decision on whether to retain, extract, surgically divide, or otherwise treat such teeth will depend on many factors including space available within the arch, the morphology of the pulp chambers and/or root canals, and the degree of attachment between the two parts of the tooth or teeth. (See Key Points 13.3.)
Figure 13.13 (a) Clinical and (b) radiographic appearance of geminated lower primary lateral incisor/canine.
Figure 13.14 Caries in extracted geminated teeth.
13.5.2 Accessory cusps
Extra cusps are not uncommon in the human dentition and may occur in both the primary and permanent dentition, most commonly affecting molar teeth. In the primary dentition the most common accessory cusps are seen on either the mesiobuccal aspect of the maxillary first molar or the mesiopalatal aspect of the maxillary second molar, the latter being similar to the cusp of Carabelli seen on the first permanent molar. The latter is a relatively frequent finding on the mesiopalatal aspect of the crown of the maxillary first molars, is typically bilateral, and may be seen in 10–60% of various populations. Permanent incisor teeth may have an additional cusp arising from the cingulum, often referred to as a ‘talon cusp’. This most commonly affects the maxillary central incisor. Talon cusps may interfere with the occlusion and may be aesthetically unpleasing (Fig. 13.15). As with double teeth, caries may occur in the groove between the cusp and the palatal surface of the incisor. Other incisor evaginations have been reported (Fig. 13.16). Permanent canines may also have a prominent lingual/palatal cusp, perhaps indicating a tendency towards a premolar tooth form. Additional cusps may uncommonly be seen on premolars.
Treatment
The talon cusp may require action for both aesthetic and occlusal reasons. Selective grinding, repeated over a period of time, will reduce the height of the cusp and allow deposition of reactionary dentine on the pulpal surface of the dentine. Single-visit sectioning of the cusp from the tooth followed by elective pulpotomy can also be considered.
13.5.3 Invaginated teeth
This term refers to the presence of an invagination in the crown of the tooth, forming an infolding lined by enamel within the crown of the tooth and sometimes extending into the root. An invagination of enamel epithelium into the dental papilla during development leads to the formation of the abnormality. The terms invaginated tooth or dens invaginatus can be used; other terms commonly applied (but not necessarily correctly) are dens in dente, gestant composite odontome, and dilated composite odontome.
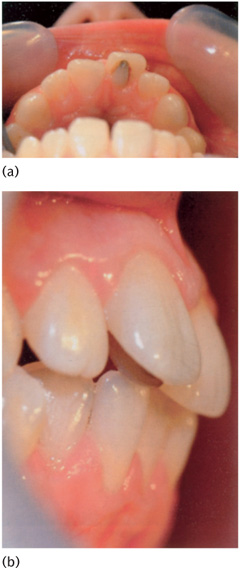
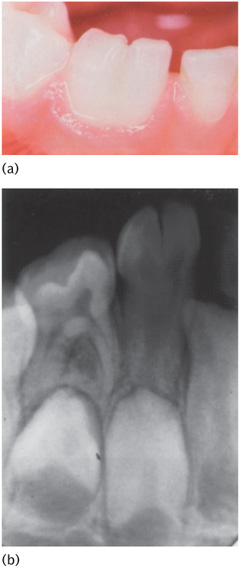
The maxillary lateral incisor is the most commonly affected tooth (Fig. 13.17). The maxillary central incisors are less commonly affected, and occasionally the canines are affected. In its mildest form an invaginated tooth is typically a maxillary lateral incisor with a deep cingulum pit on the palatal aspect of the crown. In its more extreme form the invagination is associated with grossly abnormal crown and root forms (Fig. 13.18). In these gross examples the crown is tuberculate with the invagination appearing on the cusp (which is the modified incisal edge) of the abnormal tooth. Radiographs show the extent of the invagination chamber. Enamel, which may be extremely thin or even absent, can be seen lining this chamber. The pulp may be displaced and surround the invagination cavity, appearing radiographically as narrow slits around the dentine forming the wall of the invagination. Sometimes the root is significantly expanded.
Figure 13.15 Accessory cusps—talon cusp with plaque accumulation interfering with the occlusion.
Invagination of primary teeth is uncommon, but in the permanent dentition has been estimated to affect between 1% and 5% of different groups. Males are more commonly affected than females, with a ratio of 2:1. Invaginations may also differ in different racial groups, with people of Chinese ethnicity being reportedly more commonly affected.
Figure 13.16 (a) Clinical and (b) radiographic appearance of accessory cusps—triform and cruciform teeth, 11, 21.
Invaginated teeth may cause problems because of the development of caries and pulpal pathology. This can occur soon after tooth eruption, with the child presenting with an acute abscess or facial cellulitis. In such cases the radiograph will invariably demonstrate incomplete root formation as well as periapical rarefaction (Fig. 13.17). The presence of one invaginated t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Key Points 13.1
Key Points 13.1


 Key Points 13.2
Key Points 13.2





 Key Points 13.3
Key Points 13.3