The Dental Patient
Learning Objectives
1 Pronounce, define, and spell the Key Terms.
2 Describe the role the assistant has in providing quality patient care.
3 Describe the forms of a patient record.
5 Define vital signs and describe the four vital signs commonly taken in the dental office.
6 Describe the procedure for taking a patient’s temperature, pulse, respiration, and blood pressure.
Key Terms
Blood Pressure
Brachial
Carotid
Demographics
Diastolic
Health Insurance Portability and Accountability Act (HIPAA)
Medically Compromised
Patient Record
Respiration
Sphygmomanometer
Stethoscope
Systolic
Temperature
Thermometer
Vital Signs
Patients are the only reason a dental practice exists. And your primary responsibility to these patients is to be a component of the dental team that provides quality patient care. This includes making patients feel welcome and comfortable in the practice. It also includes maintaining the patient’s safety and well-being during treatment. See Box 11-1: The Assistant’s Responsibilities to the Patient.
The Patient Record
Before any treatment can begin, the dentist will request personal and clinical information from the patient. The patient record is an important legal document that maintains this information about a patient. Each patient has a separate record. This information is obtained by asking the new patient to complete the printed forms at the first visit.
There are circumstances when a patient may be unable to complete the forms, such as a language barrier, not being able to read, or being visually impaired. When this is apparent, assist the patient by helping him or her to complete the form’s and by answering any questions necessary to help the patient provide the required data.
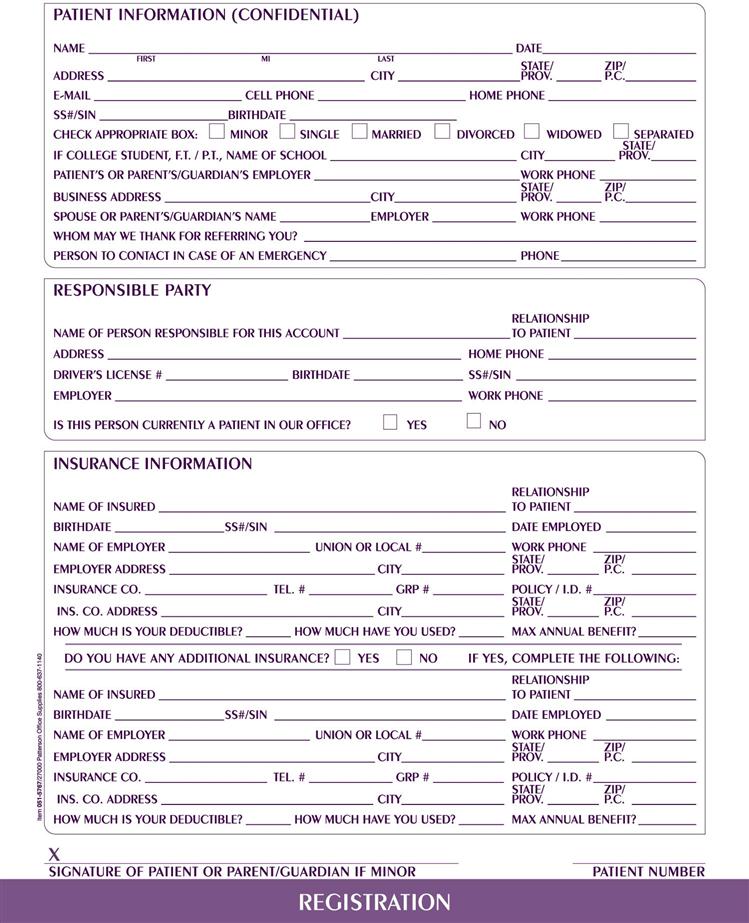
Patient Registration
The patient registration form is completed and used primarily for the business office in management of the account. Information gathered here must be complete and accurate (Figure 11-1) and includes the following:
Clinical Information
The patient record also consists of a medical and dental history completed by the patient and a record of all examination findings and treatment descriptions as dictated by the dentist. The patient’s radiographs, laboratory prescriptions, and any correspondence will also be stored within the patient record. The patient must give consent by signing a release of information form before a consultation between the dentist and the physician can take place.
Medical History
The medical history asks questions regarding the patient’s past medical history, present physical condition, chronic conditions, allergies, and medications. Each new patient must complete a medical history form before treatment can begin (Figure 11-2).
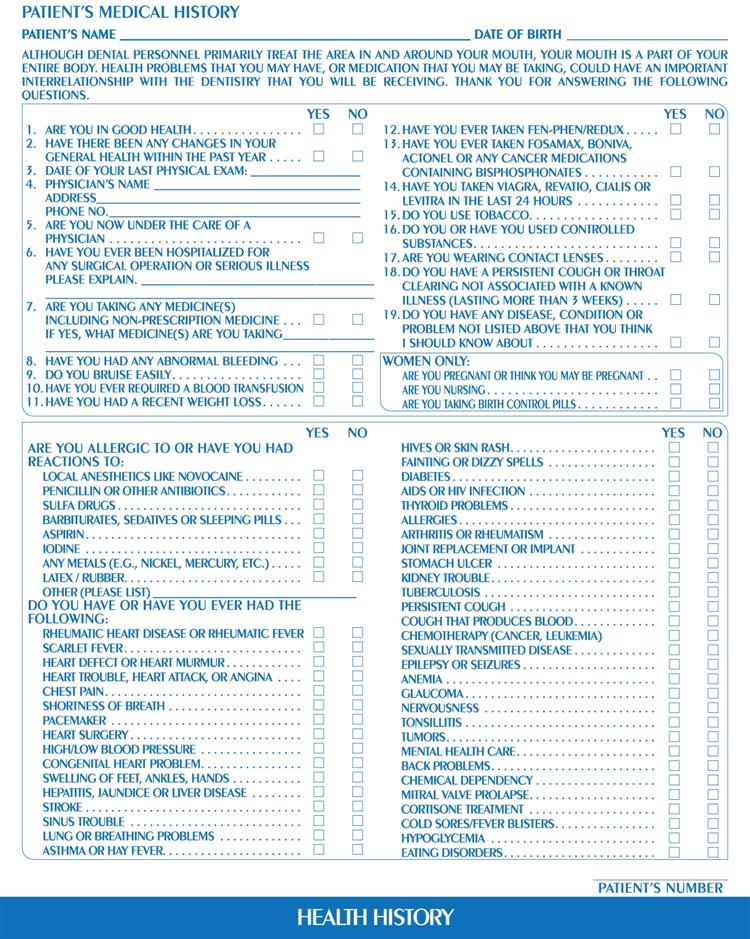
The patient’s signature on the form indicates that he or she has provided the information and takes responsibility for its accuracy.
A complete and up-to-date medical history is important because it
• Alerts the dentist to medical conditions and medications that may complicate treatment
• Aids the dentist in identifying any special treatment needs
• Alerts the dentist to any allergies that could pose a potential medical emergency
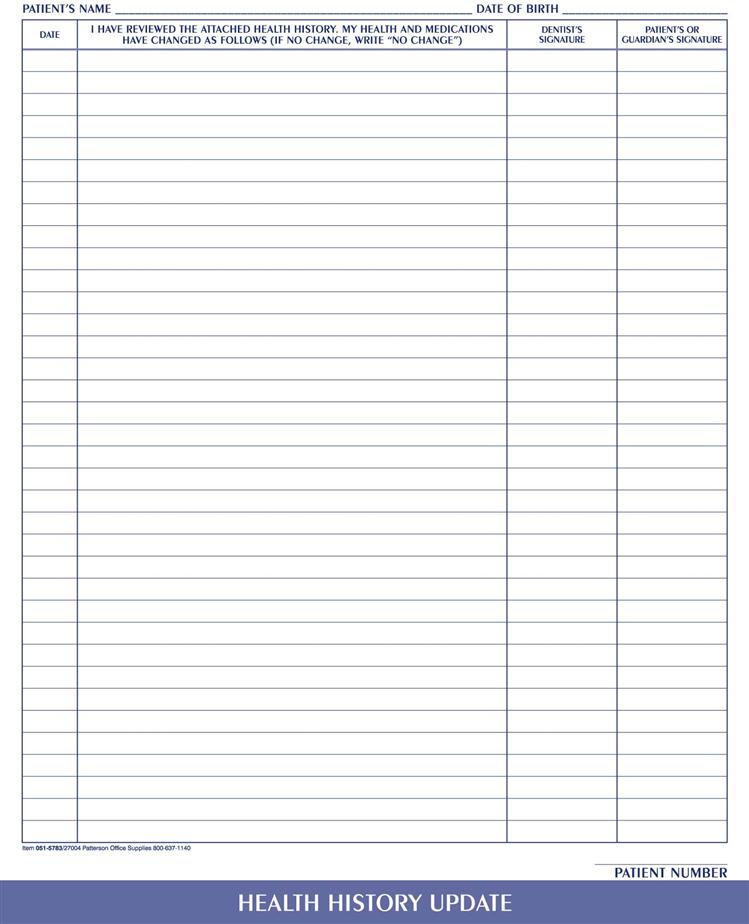
Returning patients are asked to update their medical history at each visit. The patient should sign the form to indicate that the information is accurate and up-to-date (Figure 11-3).
The dentist may also wish to consult the patient’s physician regarding health problems, particularly if the patient is medically compromised. (Medically compromised is defined as a patient with an illness or physical condition that may influence the way dental treatment is provided.)
Medication History
A medication history, which is an essential part of the medical history, is a record of all the medications a patient is currently taking. These include prescription drugs, over-the-counter drugs, vitamins, and any other drugs. This history is particularly important in older patients, many of whom have chronic conditions and are taking several prescribed and over-the-counter medications.
The dentist needs to be aware of these medications because either the medicine or the condition for which it was prescribed may modify the selection of anesthetic, premedication, and procedures when providing dental treatment.
Allergies
If the patient has any known allergies, it is extremely important that the dental team be aware of these. A reaction could increase with severity each time the individual comes into contact with the substance. For this reason, it is important to ask about both known and suspected allergies.
Of particular concern in the dental setting are allergies to latex, antibiotics, pain medication, and local anesthetic solutions (Box 11-2).
Medical Alert
If the patient has a predisposing medical condition that could impact decisions regarding dental treatment, this information must be indicated on the inside cover of the patient record. A brightly colored “ALERT” sticker is placed for the attention of the dental team. The alert sticker should never be placed on the outside of a patient record because this would violate dentist-patient confidentiality and the privacy of the patient.
Dental History
The patient’s dental history offers important clues in reference to previous dental care. Questions can include how recently the patient received dental treatment, the frequency of dental visits, and the patient’s attitude concerning the importance of the appearance of his or her own teeth and dental care.
See Procedure 11-2: Obtaining a Medical-Dental Health History.
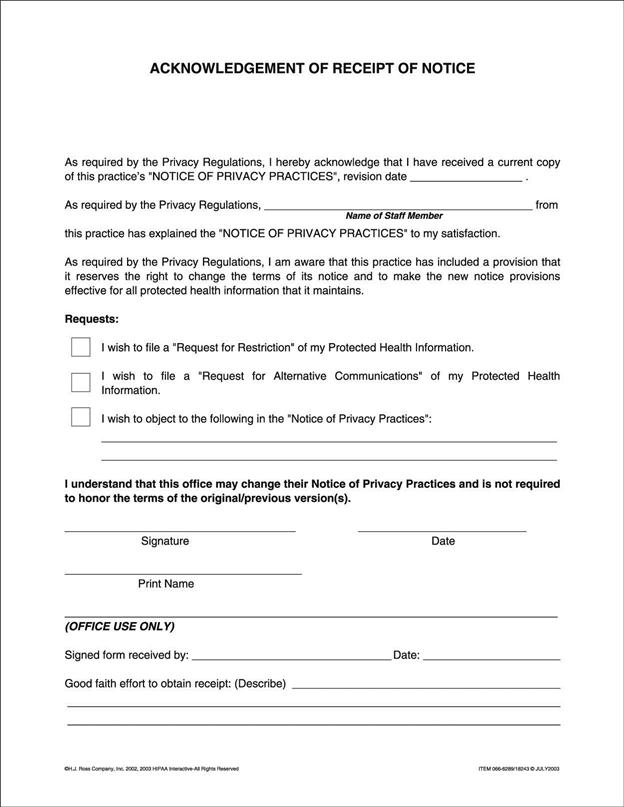
Privacy Policy of the Health Insurance Portability and Accountability Act
The Health Insurance Portability and Accountability Act (HIPAA) requires that all dental practices have a written privacy policy. This policy must inform the patient that the office will not use or disclose protected health information (PHI) for any purpose other than treatment, diagnosis, and billing. The privacy policy must be available for patients to review, and all patients (new and existing) must sign an acknowledgment of receipt of privacy practices. The signed acknowledgment must be kept in the patient’s record for a minimum of 6 years (Figure 11-4).
HIPAA states that additional authorization and consent from the patient would be required if the disclosure of documents were to be used for healthcare operations, research, or public need.
It is necessary to be in a private or semiprivate area when reviewing a health history or any specific content of a patient record.
Additional information about HIPAA can be found at: http://www.ada.org/prof/resources/topics/hipaa/index.asp.
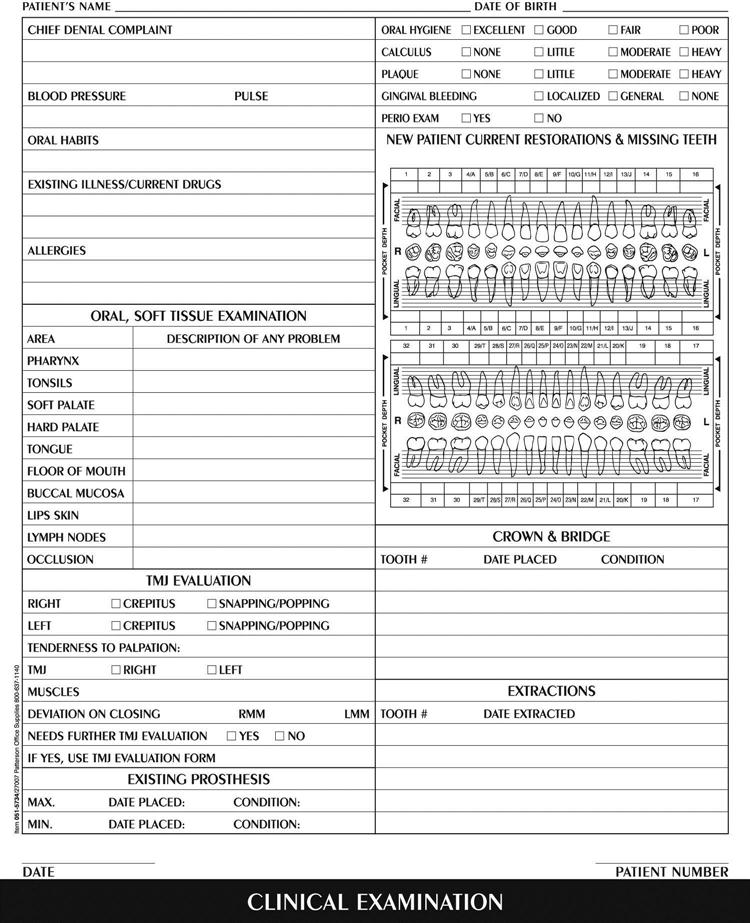
Clinical Examination
The clinical examination form is the most detailed document in the patient record. This form provides the dental team all examination data from the past, present, and future. Each time a patient comes in for an appointment, this form will be updated (Figure 11-5).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses