Chapter 11
Preparation of the Mouth for Prostheses
- Preservation of alveolar bone
- Surgical preparation for tissue-borne prostheses
- Surgical preparation for endosteal implant-borne prostheses
The surgical preparation of the mouth for prostheses begins at the time the first permanent tooth is extracted. At this and at all subsequent operations the oral surgeon must try to leave the soft and hard tissues in satisfactory condition to support a tissue, tooth or implant borne prosthesis. For more complex cases it is helpful for surgeon and prosthodontist to plan the case together. Even for simpler cases, it is always important that the practitioner considers the future prosthodontic requirements when selecting any surgical procedure. Joint planning of surgery for prostheses should give the surgeon a clear treatment plan and a transparent rationale to work to. Joint planning should also ensure the retention of potentially restorable teeth either to assist denture retention or bridge construction, or to retain overdentures, which will help maintain alveolar bone height.
As a general rule those who require tissue-borne prostheses, for example complete dentures, should not be subjected to surgery to improve the stability, comfort or aesthetic appearance of their dentures without the opinion of a specialist prosthodontist or restorative dentist. This is largely due to the advancement in prosthodontic techniques that may mean surgery can be avoided altogether, or that less extensive surgery can be carried out.
This chapter will outline some general principles on the preservation of alveolar bone and discuss some of the preparatory surgery for tissue-borne prostheses. However, it will largely concentrate on the implant-borne prosthesis. This is due the increasing importance of implants in prosthodontics. The surgical techniques discussed throughout the chapter such as torus removal, bone grafting, etc., are equally applicable to tissue-borne, tooth-borne and implant-borne prosthesis.
Preservation of Alveolar Bone
Atraumatic Extraction
This is a contradiction in terms; however, the principle it tries to communicate is sound and appropriate for all oral surgeons. It should always be borne in mind that alveolar bone is precious and once lost cannot easily be replaced. This is even more important since the advent of dental implants. Alveolar bone, possibly more than any other tissue, suffers from instrument mismanagement, and a conservative approach with a careful surgical technique will help to reduce prosthetic difficulties later.
During extractions the alveolar bone may be damaged or fractured by the use of excessive force or worse, by the inclusion of the socket wall within the forcep blades. The commonest site of alveolar fracture is the buccal plate of the upper molars. The surgeon should always strive to avoid the fracture and loss of the maxillary tuberosity as this may interfere with retention of the upper denture by making the peripheral seal at this point inadequate. Alveolar bone, if still attached to periostium, may be preserved and pressed back into place, but if detached from its blood supply it should be removed to avoid sequestration and delayed healing.
Consideration should be given to the initial use of periotomes to cut the periodontal ligament, followed by luxators to begin the widening of the tooth socket, prior to application of elevators and forceps (see Chapter 8). Sectioning multirooted teeth before extraction and the use of piezoelectric instruments, harnessing ultrasonic forces to sever the periodontal attachment and remove bone, may facilitate minimally traumatic extractions. Alveolar bone may also be conserved by the immediate placement of implants directly into healthy extraction sites.
Difficult extractions may be best completed through a planned transalveolar approach to avoid accidental alveolar fractures that may lead to more widespread loss of bone. Sharp burs and copious irrigation should be used to help prevent overheating of the bone and subsequent necrosis.
Access to deeply buried roots or teeth can often be made through the lateral aspect of the alveolus, leaving the ridge intact. Indeed, this principle holds true for access to cystic or granulomatous tissue at apices. This approach attempts to maintain ridge height for any prosthesis planned. In all such operations bone cutting should be limited to one side, leaving the lingual or palatal plate and its mucoperiostium untouched. Osteoplastic flaps, as described in Chapter 9, are an alternative to lateral access to deeply buried roots or teeth. Piezoelectric saws now allow minimal trauma to both hard and soft tissues when creating such flaps. Sometimes it is more appropriate to leave a buried root to be removed at the time of preparing the bone for a dental implant.
Edentulous jaws can prove a difficulty, as the bone in such jaws is often dense and brittle. Compounding this is the resorption of the alveolar ridge, which makes the bone less strong. Under such conditions the extraction of buried teeth and roots can be difficult. Those teeth and roots that are symptomless need not be extracted if they are covered by bone and are unlikely to come to the surface during the life of the denture or to affect any planned implant placement. Those lying superficially, close to implant sites, or that are associated with secondary disease such as cysts or granulomas, should be removed. Roots and teeth must be accurately localised and tooth division carried out to reduce the amount of bone removed. This is confined as far as possible to the buccal aspect, and osteoplastic flaps are used to preserve the ridge where teeth are lying in it.
Socket Preservation
This involves minimising the trauma of the extraction by the methods described in previous paragraphs followed by the placement of autogenous (from the same individual), allogenous (from another individual of the same species, e.g. cadaveric bone) or xenogenous (from another species, e.g. cow) bone, or alloplastic substances (synthetic or naturally derived material, e.g. calcium triphosphate or hydroxyapatite) into the empty socket. Either a mucosal graft or a biological membrane is then used to cover the inserted material.
The principles behind this technique are dependent on the material placed within the socket but the aim is to reduce to the absolute minimum the amount of local alveolar resorption. Potentially it can provide:
- osteogenesis – only autogenous bone has this potential
- an osseoinductive stimulus – autogenous and allogenous bone
- an osseoconductive scaffold to facilitate bone formation – alloplasts, allogenous and xenogenous bone.
Practitioners should be wary of placing any type of material into recently infected sites as some new bone should be formed irrespective of whether or not a material is placed into the socket following extraction.
Bone Recontouring
It is advisable to do the minimum recontouring of the bone at the time of extraction and wait for at least 3 months to reconsider the situation once healing and remodelling has taken place, as some natural resorption always takes place and it is impossible to tell how extensive this will be. A conservative approach is particularly important where periodontal disease has already caused appreciable bone loss. Indications for minor surgery at the time of the extractions include the following.
- Jagged or irregular alveolar margins and septal bone, which are treated by dividing the buccal interdental papillae from the lingual along the ridge and exposing the bony edges of the sockets just enough to smooth the bone with a bur or file, after which the mucosa is closed over the ridge.
- Minor local deformities, such as fibrous bands, bulbous tuberosities and undercuts, which may be removed.
Surgical Preparation for Tissue-Borne Prostheses
Surgery for Complete Immediate Dentures
Where a complete denture is to be provided, consideration can be given to removing all the posterior teeth first. Sufficient teeth can be left in the premolar region to maintain the vertical dimension of the occlusion while the molar sockets are healing. Three months later the rest of the teeth are removed and the denture(s) inserted.
When an anterior flange cannot be worn either because it would cause the lip to be over supported in an unsightly way, or there would be an undercut preventing flange insertion, an open-faced denture with the anterior teeth socketed into the alveolus is provided as a temporary measure until natural resorption has taken place. In certain cases, however, it is obvious that some alveolectomy is necessary at the time the teeth are extracted.
Where the patient must be admitted to hospital for a general anaesthetic, the less satisfactory procedure of fitting an immediate complete denture can be performed.
Hard Tissue Irregularities
Torus
A large palatal torus can be prosthodontically acceptable if smooth, but when nodular or irregular in shape it may need to be removed. Tori, often bilateral, are sometimes found on the lingual aspect of the mandible in the premolar region and can cause pain from denture contact or interfere with the path of insertion.
The torus palatinus is excised through a Y-shaped midline sagittal incision and the bony prominence removed with burs, chisels or a piezoelectric saw. A full denture or cover-plate lined with a periodontal dressing is immediately fitted to hold the flap in place and prevent formation of a haematoma (Figure 11.1).
Figure 11.1 Tori. (a) Mandibular tori would cause problems when denture is worn. (b) Palatal torus.
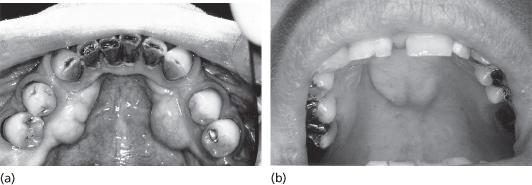
Mandibular lingual tori are removed where they cause a hindrance to the design of tissue- or tooth-borne prostheses or when they are continually traumatised by a denture. A lingual mucoperiosteal flap is raised and an instrument (e.g. a Howarth periosteal elevator) is passed below the torus to isolate it. Burs or a piezoelectric saw can be used to section the majority of the distance through the torus and final fracture is achieved with an elevator. The torus is removed and the operation site, smoothed, debrided and toileted.
Tori in either arch can provide an excellent source of bone for grafting and should be one of the considerations when bone is required elsewhere in the arch.
Alveolectomy
This is the operation used to smooth irregular ridges and remove undercuts. Radiographs must be studied to determine the extent of the antrum and the position of the mental nerve. Plaster casts of the ridges may be used to assist planning so that the procedure is completed with minimum unnecessary destruction of alveolar bone.
A horizontal incision is made on the buccal aspect of the alveolus through fixed mucoperiosteum just short of non-keratinised mucosa so that this is not disturbed by the operation. Two vertical incisions are taken over the crest of the alveolus and on to the lingual or palatal mucosa. The flap is reflected to expose the alveolar crest. The bone may be trimmed with a large rosehead bur or rongeurs and smoothed with a bone file. The operator then replaces the flap and runs their finger over the ridge to check it is smooth. The wound is thoroughly irrigated with saline and if much reduction has taken place the flap is trimmed conservatively. The mucoperiosteal flap is closed without tension.
Feather Edge Ridge
This condition typically occurs in the lower anterior region. The patient complains of inability to wear the denture for more than 1 or 2 hours owing to soreness. The ridge is usually very narrow and covered with thin atrophic mucosa, which is inflamed and tender to palpation. Radiographs show an uneven resorbed ridge with a feathered appearance due to spicules of bone standing vertically.
Surgery should be considered only when all prosthetic techniques to reduce the load (selective compression impressions, narrow teeth and resilient linings) have failed.
Genial Tubercles
These sometimes become prominent in the floor of the mouth owing to alveolar resorption. They are best left, as genioglossus is attached to them. Occasionally, the upper part of a prominent genial tubercule may require excision to facilitate denture wearing.
Mylohyoid Ridge Removal
Where the mandibular alveolus has undergone gross resorption, the mylohyoid ridge may be at the level of the resorbed alveolus and, if sharp, be a source of pain under the lower denture. Its removal, by cutting off the attachment of the mylohyoid muscle, does deepen the lingual sulcus of the mandible and may assist denture retention.
An incision is made along the alveolar crest and reflected lingually to expose the mylohyoid muscle, which is detached from the bone. The prominent bony mylohyoid ridge is then separated from the mandible with burs. Bleeding is meticulously arrested and the incision closed. This procedure may be carried out in combination with sulcus deepening in the anterior mandible (see later in this chapter).
Soft Tissue Irregularities
Mobile Ridges
Ideally, denture-supporting alveolar mucosa should be firm and closely adherent to the ridge, but especially after the extraction of teeth for periodontal disease, hyperplastic tissue may remain to form a mobile ridge. Often such ridges are found in the anterior region of the maxilla when a full upper denture is opposed only by the natural lower anterior teeth. The occlusal forces from the natural lower dentition against the complete upper denture is thought to cause localised resorption of the maxillary bone, leaving a thick mobile fibrous ridge of soft tissue. The thick mobile ridge offers unstable support for the denture. However, as this may be better than the alternative of a completely flat surface left by surgery, the prosthodontist often prefers to manage this problem with special impression techniques and denture design. An alternative approach is to augment the underlying bone with alloplastic substances to try and provide support for the soft tissue.
Reduction of Tuberosities
With careful denture design and construction techniques, large maxillary tuberosities with deep sulci can assist retention, but if too large they may encroach on the interocclusal space available for dentures. Many also have appreciable bony undercuts on their buccal aspects, which, if unilateral, can be used to improve denture stability, but when present bilaterally, interfere with the path of insertion. Radiographs before surgery are necessary to identify unerupted upper third molars, to establish the relationship between soft tissue and underlying alveolar bone, and to determine the extent of the maxillary antrum.
Treatment
A fibrous tuberosity may be reduced by making palatal and buccal incisions down to bone to excise a wedge of mucous membrane, fibrous tissue and periosteum from the crest of the ridge. To facilitate closure the incisions are carried forward to meet in the first molar region. The raw edges are then undermined and the underlying fibrous tissue removed to produce a reduction in the height of the ridge and to allow satisfactory closure (Figure 11.2). The space available for denture(s) between upper and lower ridges at the approximate occlusal vertical dimension is checked before the wound is sutured.
Figure 11.2 Reduction of the tuberosity. (a) Above: Elliptical incision over tuberosity. Below: Cross-section of excision showing deep portion secondarily excised (shaded) to allow flaps to be apposed on bone without tension. (b) Closure.
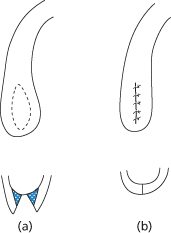
Where only the bone is to be reduced in height or a buccal undercut removed, the approach is made through a buccal mucoperiosteal flap. Care is required not to perforate the antral lining when cutting bone in this region. Usually both bone and soft tissue are to be reduced and the elliptical incision is used to expose the ridge by reflecting the edges of the wound. Buccal undercuts in this area are often found high above the crest, making a vertical incision at the anterior buccal edge of the ellipse necessary.
Fraenectomy
A fraenum is a musculofibrous band attached to the alveolus and inserted into the muscles of the face or tongue. The most important of these are the labial fraena in the midline of the upper and lower jaw, the buccal fraena in the premolar region and the lingual fraenum of the mandible. During movements of the facial muscles or tongue, fraena can lift the dentures and so reduce their stability. The denture can usually be relieved around the fraenum in question, but where the ridges have resorbed and the fraenum approaches the crest of the ridge, this may greatly reduce the possible depth of the flange and even weaken the denture, making treatment by excision necessary.
Treatment
The maxillary labial fraenum is excised as follows. First the extent of its attachment to the maxilla is found by drawing the upper lip forward to put the fraenum on tension. This causes the base to blanch and it is frequently seen to extend palatally into the incisive papilla. The whole length of the fraenum and the mucosa over it is removed but the periostium is left intact. A diamond-shaped incision is made round the margins of the band sufficiently deep to allow it to be dissected out and for the portion in the lip to the superficially excised (Figure 11.3). The mucosa is undermined before suturing. The effect of suturing the lateral edges of the diamond-shaped incision together is to lengthen the wound and this allows a greater depth of sulcus to be achieved.
Figure 11.3 Fraena. (a) Incision for excision of labial fraenum. (b) Lingual fraenum lengthened by making a horizontal incison A–B and suturing it vertically.

Fraena may be lengthened by making a horizontal incision across the middle of the band which passes through the whole depth of the fibrous tissue it contains. The mucosal edges are undermined and the incision is sutured vertically (Figures 11.4 and 11.5).
Figure 11.4 Fraenectomy. (a) Tight labial fraenum. (b) Following fraenectomy. (c) Tight lingual fraenum.

Figure 11.5 Denture hyperplasia.

Denture Irritation Hyperplasia
This is a fibroepithelial overgrowth in response to chronic trauma. The cause is an overextended denture flange, which transmits the masticatory forces to the soft tissues. This situation often occurs with continued use of a denture following resorption of the ridges (Figure 11.5).
The denture hyperplasia may present as one fold or a series of folds like the leaves of a book, which lie in the buccal sulcus either between the alveolus and the denture or along the periphery of the flange.
Treatment
First the irritation is removed by leaving out the denture or easing back the flange. The patient is reviewed after one month and if satisfactory recession has not taken place, the hyperplasia should be excised.
A single hyperplastic fold can be removed by excision at its base with either a blade or laser. The edges of the resultant wound are then undermined and sutured without altering the depth of the buccal sulcus. Large multi-leaved hyperplasias require excision. If a multi-leaved hyperplasia is excised with a laser then the resultant open wound will present less pain while healing and can be left to heal by secondary intention. If a blade is used to excise a multi-leaved hyperplasia consideration should be given to covering the resultant raw area with a split thickness skin graft or a mucosal graft from the cheek or palate to help reduce contracture and pain. Removal of a multi-leaved hyperplasia may be combined with sulcus deepening if necessary.
Cryosurgery has also been used to remove multi-leaved hyperplasia and does leave a satisfactory />
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


