CHAPTER 10
Subnasal Elevation and Bone Augmentation
The anterior maxilla commonly lacks sufficient bone height for implant placement. To augment both the quantity and quality of bone in the anterior maxillary residual crest, a subnasal elevation followed by bone grafting may be performed. This useful technique can predictably elevate the nasal mucosa 3 to 5 mm prior to grafting and is indicated when the residual crest is less than 10 mm in height. Prior to implant insertion, the recipient bone bed in the anterior maxilla should ideally be at least 6 mm wide and 13 mm high.1 This allows for the placement of longer implants (10 to 13 mm), which increase the success of implant restoration in this area. 2, 3, 4 The technique also deters penetration of the implant into the nasal cavity, which has been shown to occur frequently when the transverse alveolar dimension of the anterior maxilla has significantly diminished.5
For the subnasal elevation, the periosteum of the labial aspect of the anterior maxilla is reflected to expose the inferior and/or lateral piriform rim (Figs 10-1 and 10-2). A nasal undercut region is typically present in the area of the lateral-inferior piriform rim, and in this region, the nasal mucosa can be elevated (Fig 10-3). Particulated graft material is typically used to augment this area. In patients with unilateral or bilateral edentulism, antral-nasal inlay composite grafts can also be used.6 For the edentulous patient with a compromised anterior maxillary region, a complete-arch onlay graft can be used to reduce the interarch space and to create an arch with a more ideal size and shape.7, 8 In totally edentulous patients, however, a complete-arch onlay graft may not be possible because of an inadequate arch space or a short upper lip.
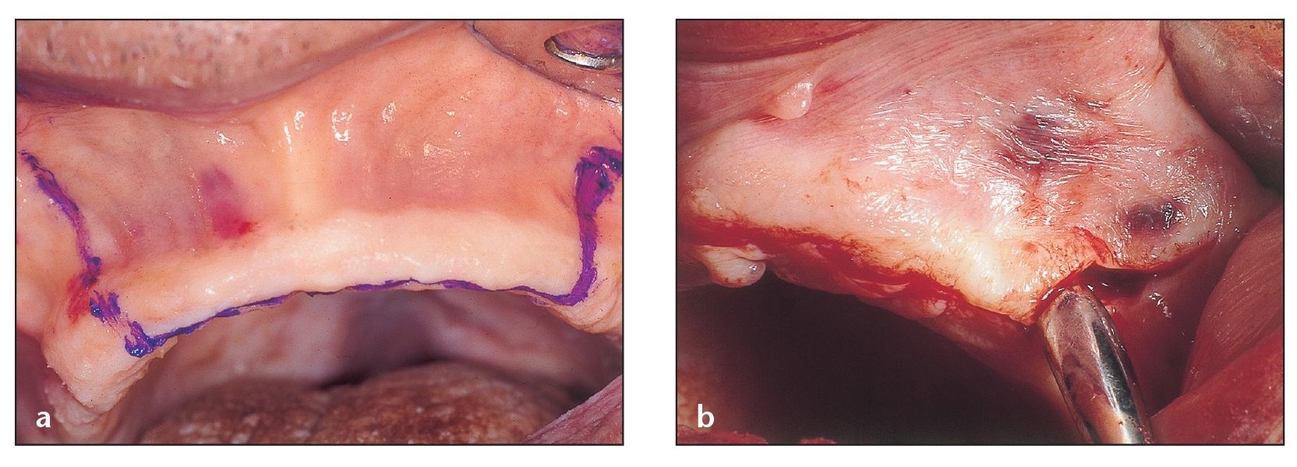
A midcrestal incision and two high vertical divergent incisions will provide a flap that can be reflected adequately to provide access and visibility for the nasal spine and piriform rims. Here the initial incision is performed on a cadaver specimen (a) and on an actual patient (b).
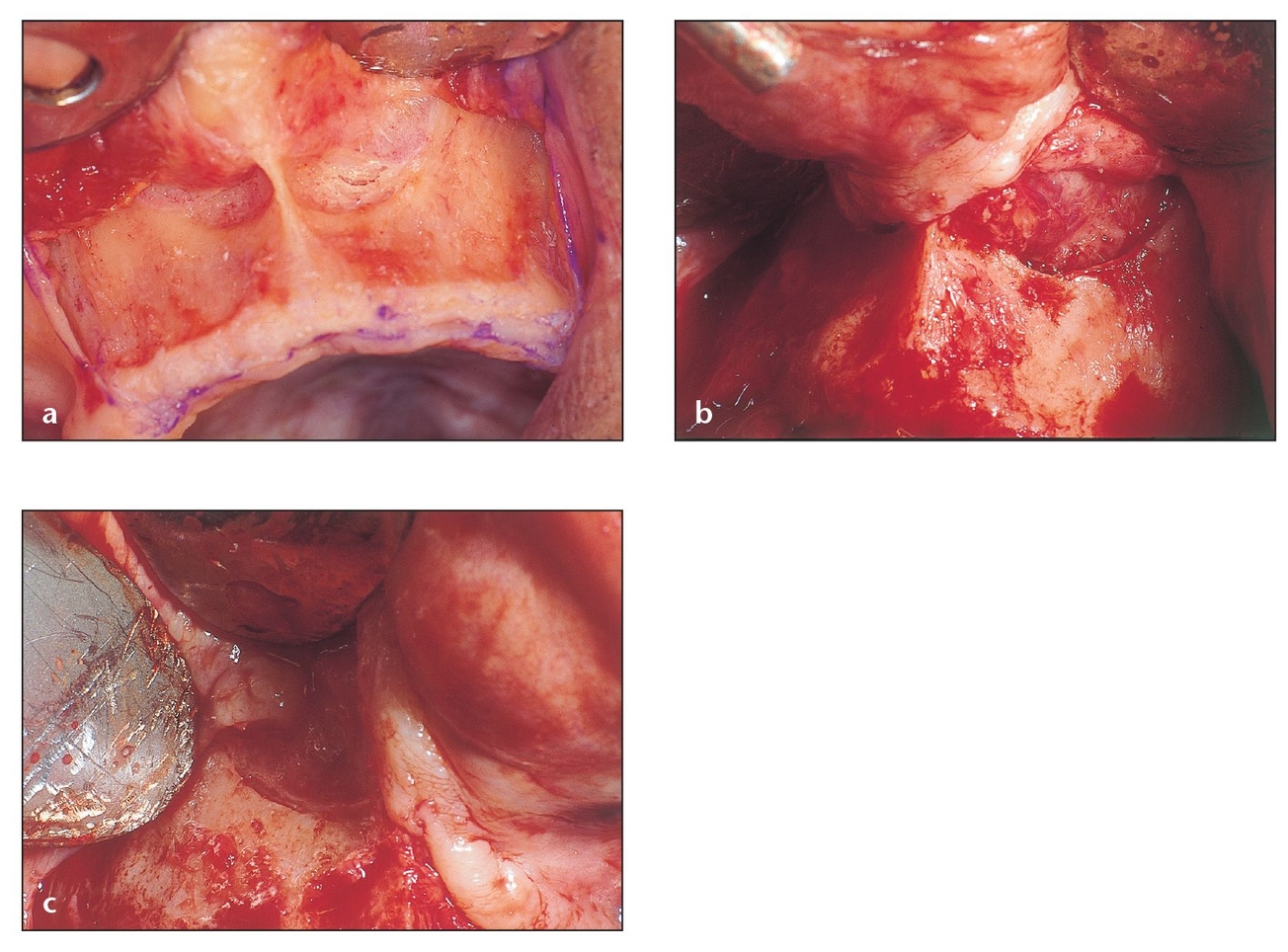
The flap reflection, shown here in a cadaver (a) and an actual patient (b and c), should be done with a sharp periosteal elevator to prevent tearing the periosteum or mucosa and should also permit a careful separation of the mucosa from the nasal lining.
A significantly resorbed maxilla, which often presents with reverse architecture in the anterior maxilla where retained or su-pererupted mandibular incisors have accelerated resorption into the basal bone, may leave only a few millimeters or complete dehiscence of the anterior nasal floor. In these situations, a 5- to 7-mm block graft is placed following nasal mucosal elevation, and an inferior septoplasty is performed. When performed in conjunction with alveolar augmentation, this procedure provides additional stability and vertical dimension for the implants.
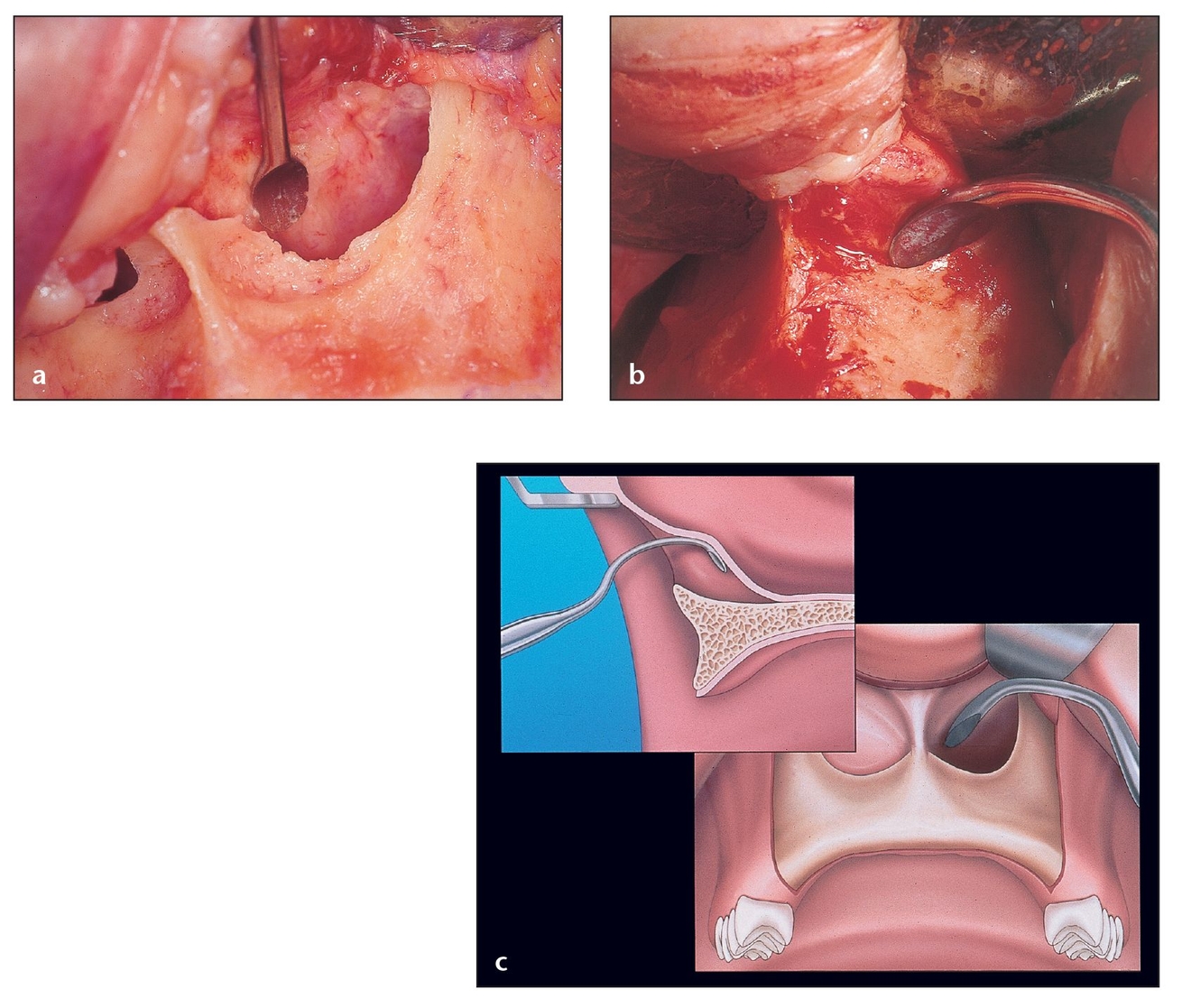
(a) The nasal mucosa should be carefully dissected to detach it from the bone starting at the piriform rim and continuing into the nasal floor. Note the separation of mucosa from bone in this cadaver demonstration.
(b) Excessive pressure could give way to a perforation. This mucosa is thicker and more resistant than the sinus membrane, but a tear here calls for a water-tight closure with resorbable sutures or aborting of the procedure because bacterial contamination could enter the grafted site from the nasal cavity.
(c) Lateral and frontal view of the correct way to hold the curette, with the concavity of the curette oriented toward the bone.
Despite these augmentation measures, inlay or onlay grafting procedures do not always adequately restore enough vertical bone to accommodate a fixed prosthesis. In that case, a continuous bar overdenture is a prudent prosthetic choice.6
In some respects, the nasal lift is similar to the maxillary sinus lift; both are performed using a soft tissue curette to elevate the mucosa. Because the nasal mucosa is generally much thicker and more tear resistant than the maxillary sinus membrane, there is less chance of perforation during elevation, and it is easier to elevate. An underlying elastic fiber makes it adhere more firmly to the underlying bone; therefore, significant pressure must be applied to elevate the nasal mucosa. The clinician should bear in mind that if a perforation occurs in the mucosa, it is imperative to suture it closed and obtain a water-tight closure to minimize the chance of bacterial flora from the nose migrating into the graft and causing contamination and infection.
This chapter outlines a step-by-step technique for performing a nasal sinus lift and subsequent grafting and also provides an overview of the nasal anatomy and vasculature, of which the surgeon must have a good working understanding before undertaking this procedure.
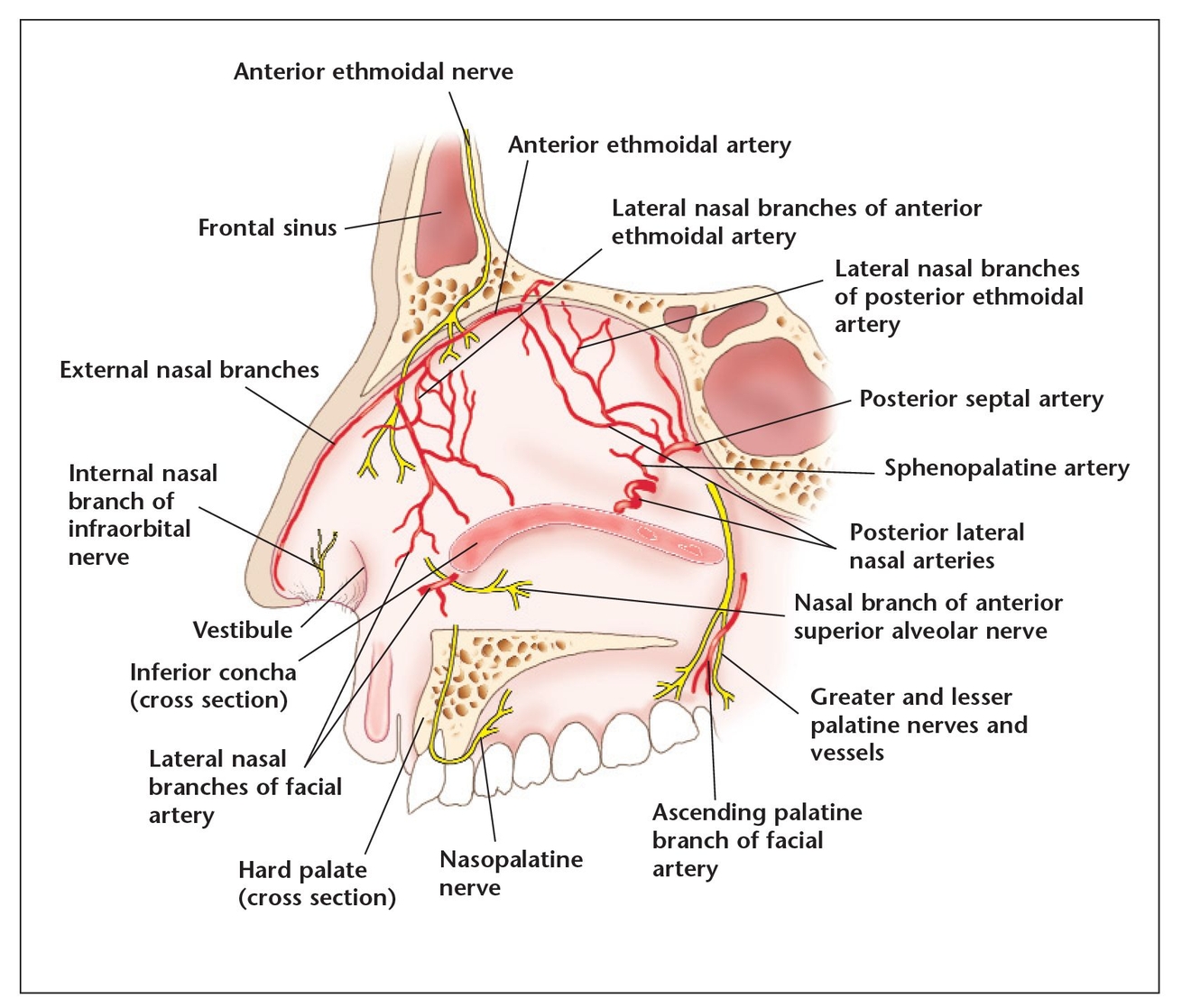
The septum—and the nasal cavity in general—is highly vascularized. This may be to warm the air before it reaches the bronchi and lungs. The arterial blood supply to the nose is derived from the terminal branch of the maxillary artery, which supplies the sphenopalatine artery, which in turn supplies the lateral and medial walls of the nasal chamber. The anterior and posterior ethmoidal arteries supply the vestibule and the anterior portion of the septum. A few blood vessels from the greater palatine artery pass through the incisive canal of the palate to reach the anterior part of the nose. Sensory innervation to the nose is also important in that it provides reflexes (such as the sneeze reflex) to keep foreign particles out of the respiratory system. For this surgery, it is critical for the surgeon to be familiar with the orientation of the anterior ethmoidal and nasopalatine nerves.
Nasal Anatomy and Vasculature
To successfully perform a subnasal elevation, the surgeon must consider the nasal structure, vasculature, innervation, and soft tissues in the operative area.
The arterial blood supply to the nose is derived from the external and internal carotid arteries. The terminal branch of the maxillary artery (a branch of the external carotid artery) supplies the sphenopalatine artery, which in turn supplies the lateral and medial walls of the nasal chamber. The anterior and posterior ethmoidal arteries (branches of the ophthalmic artery, which itself is a branch of the internal carotid artery) supply the vestibule and the anterior portion of the septum. A few blood vessels from the greater palatine artery pass through the incisive canal of the palate to reach the anterior part of the nose (
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


