CHAPTER 9
Augmentation and Grafting for the Maxillary Anterior Alveolar Ridges
The anterior maxilla is the most challenging region of the dentition to restore (Fig 9-1).1, 2, 3, 4 Bone grafting to support esthetics is key in this prominent area because the underlying ridge must support both the implant restoration and the soft tissue to achieve a long-lasting, esthetic result. These factors are particularly important in cases involving two or more teeth. Osseointegration of dental implants, particularly in the anterior maxilla, depends on adequate trabecular bone density, ridge height and width,5 and systemic bone health. The clinician must evaluate all of these factors to ensure that implants can maintain osseointegration during function. 6, 7, 8, 9, 10, 11 Furthermore, the clinician must take advantage of all available clinical, laboratory, and communication technologies to meet the patient’s functional and esthetic needs.12
Bone augmentation is required when anterior tooth loss leads to the loss of bone volume needed for proper implant positioning. 13, 14 The diameter of the implant, compared with that of natural teeth, can create challenges associated with the cervical esthetics of the crown. Other unique problems that may limit ideal placement of implants in the anterior maxilla include (1) a resorbed (from periodontal disease) or fractured (from extraction) facial cortical plate over the maxillary roots of the teeth; (2) close proximity of the nasal and maxillary sinus cavities; (3) lateral extension of the incisive canal; (4) facial concavities; and (5) reduced turnover and health of bone caused by aging or metabolic disease (which may not be revealed until after implant placement) (Fig 9-2). Attention must also be paid to developing a healthy and esthetic soft tissue result and a natural emergence profile,15, 16, 17, 18, 19, 20, 21, 22 with soft tissue grafting undertaken as needed.23, 24, 25, 26, 27, 28 Thus, the clinician must develop a comprehensive treatment plan that allows the surgeon, the laboratory technician, and the restorative clinician to visualize the anticipated result before treatment begins.
From simple restorations to complex reconstruction, the prominence and visibility of the anterior maxilla always presents challenges.
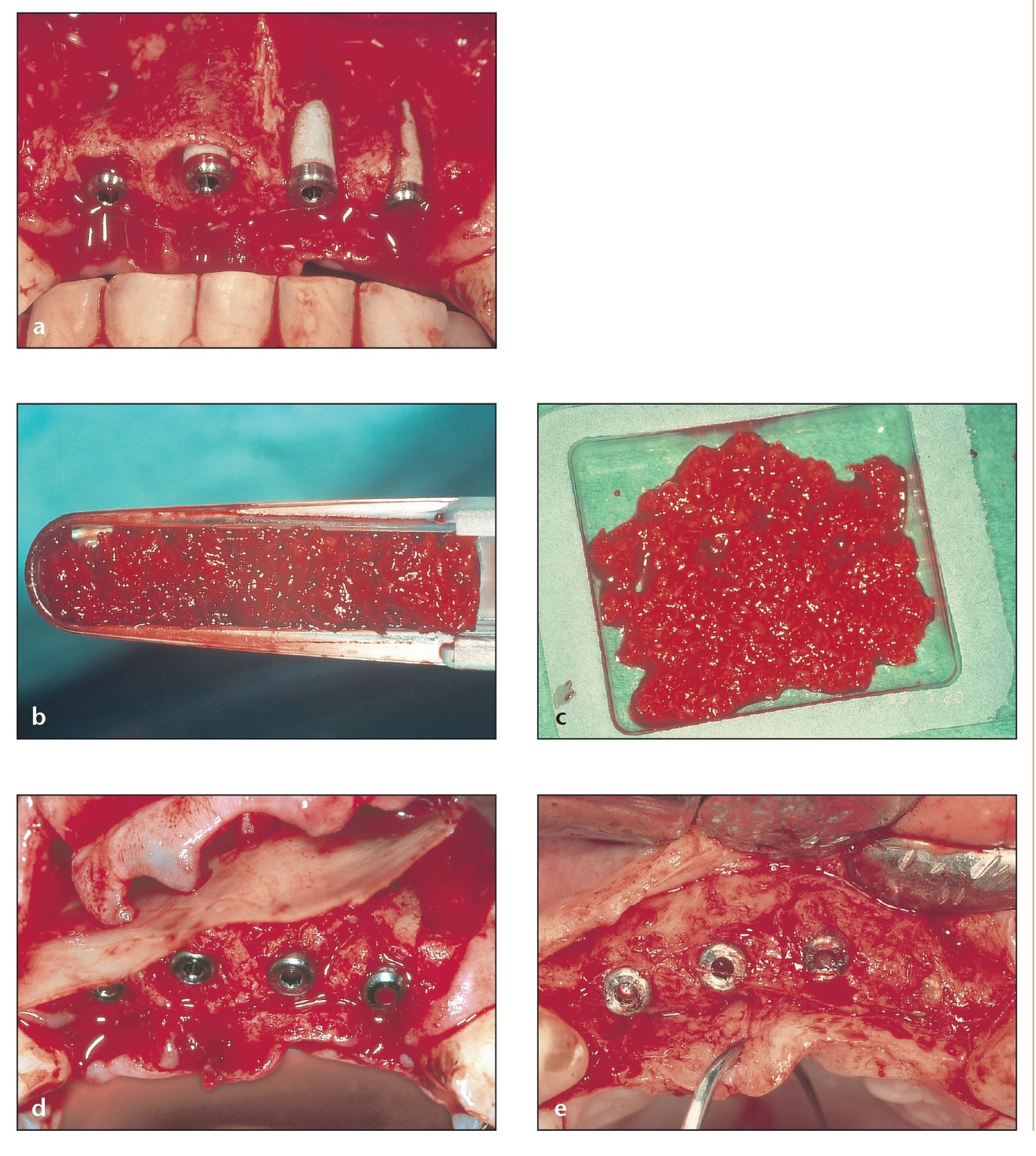
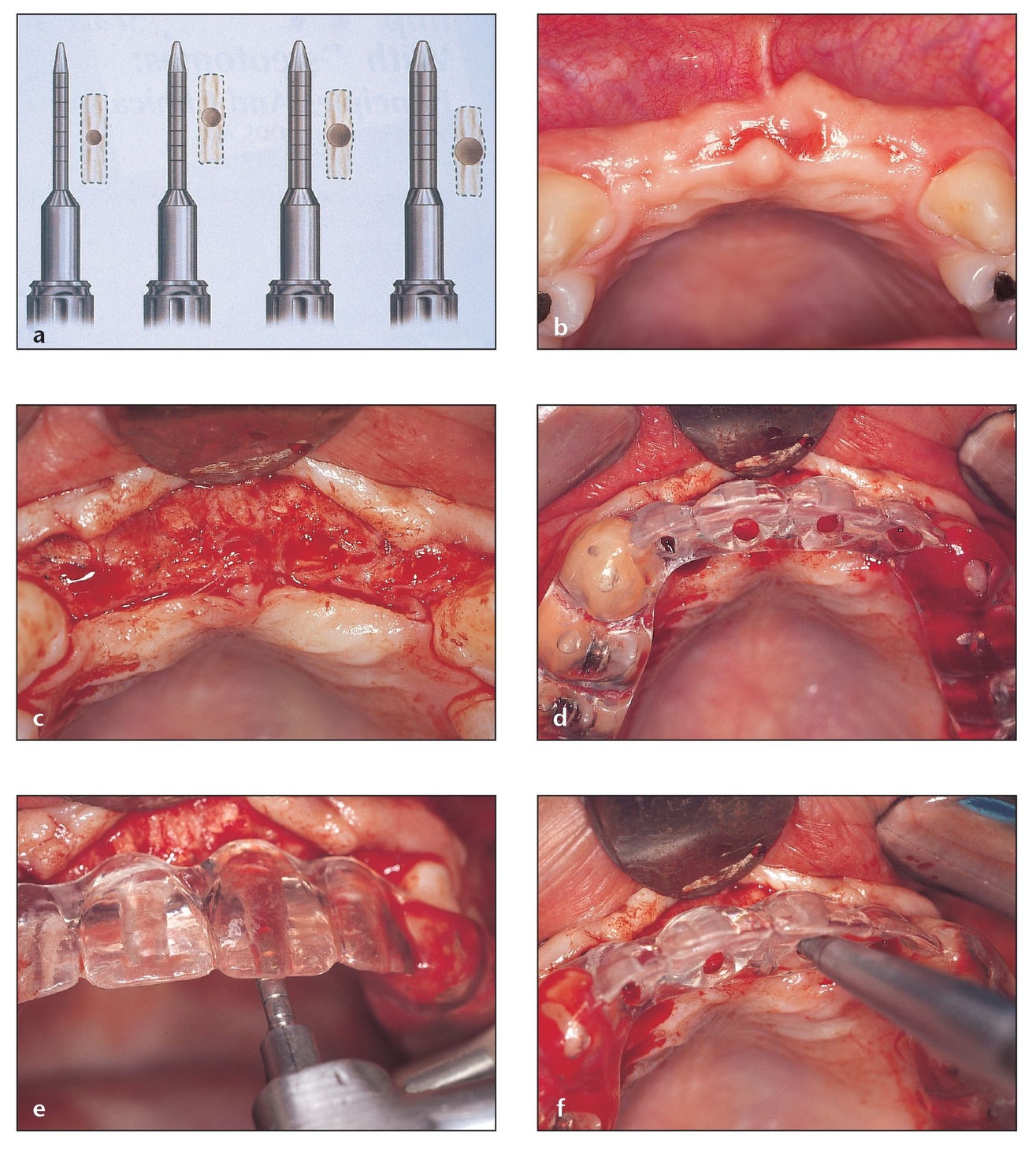
Fig 9-2 Bone volume must be adequate not only for proper face contour and lip support but also for exact positioning and angulation and correct intermaxillary relationship of subsequent implants.
(a) This partially resorbed maxilla required grafting and implants.
(b) A bone shaver can provide particulate bone, even from the implant area, while the ridge is simultaneously smoothed.
(c) As little as 2 mL of particulate bone can adequately cover the buccal surface of two exposed implants.
(d) A thin piece of lamellar allogeneic bone can be placed over the implants to help keep the particulate bone in place and keep soft tissue cells from invading the area where bone growth alone is desired.
(e) After 6 months, the implants show perfect coverage; extra bone can be removed from the head of the fourth implant at this stage 2 procedure.
Evaluating Tissues to Determine Grafting Needs
During treatment planning for implant placement in the anterior maxilla, the clinician must analyze the topography of the edentulous ridge, particularly from the in-cisogingival and faciolingual positions. Adequate bone must be available to accommodate the number and length of implants needed to support the planned restoration and the soft tissue architecture. 29 The examination is done clinically and radiographically. If even more information is needed, a computerized tomography (CT) or spiral tomography scan30 may be used to obtain a three-dimensional view. This implant placement technology is complemented by the three-dimensional placement of abutments via computer-aided design/computer-assisted manufacture (CAD/CAM) technology to help provide functional and esthetic satisfaction for the patient.31 Additionally, a waxup of the ridge as well as the missing tooth or teeth can be requested from the laboratory.
The approach to implant restoration will depend on whether a single tooth or multiple teeth are being restored32, 33, 34, 35, 36, 37, 38, 39, 40, 41 and whether implant placement is immediate or delayed.42, 43, 44, 45, 46 If more than two teeth are missing, reducing the number of implants can improve the esthetic outcome by enhancing the peri-implant soft tissue architecture at the pontic area.47 The clinician can then take steps to develop the inter-implant papillae. If there are the same number of implants as there are missing teeth, creating the illusion of papillae can be difficult.48, 49, 50
Anterior Ridge Augmentation Methods
To determine whether and how to augment the anterior alveolar ridge of the maxilla, the clinician must consider the crown-to-implant ratio and the incisal edge position in relation to the implant body. The morphology of the defect must also be considered because it will determine which techniques or graft materials will be used. Ridge augmentation techniques (separately or in combination) to accommodate implant placement in the anterior maxilla include nasal floor elevation with grafting (see chapter 10), ridge spreading using osteotomes, corticocancellous autogenous block bone grafting (see chapter 5), and guided tissue regeneration (see chapter 3). Table 9-1 lists the classifications of ridge augmentation techniques according to the severity of the ridge deficiencies. Generally, if 4 to 10 mm of ridge thickness is available, a variety of office-based procedures can be considered. More severely resorbed or otherwise grossly deficient ridges require more extensive treatment.
Mucogingival reconstruction may also be required in anterior maxillary restoration cases. If horizontal and vertical dimensions of the ridge deficiency are within 3 mm of their original contour, good results can be achieved using soft tissue augmentation procedures, such as pedicle connective tissue grafts and free onlay or inlay connective tissue grafts harvested from the palatal mucosa. These grafting procedures can be performed prior to implant placement or during the submerged healing phase.51, 52, 53
Classification of ridge augmentation techniques
| Ridge thickness | Procedure |
|---|---|
| 8 to 10 mm | Barrier membranes alone |
| 7 to 8 mm | Particulate graft and barrier membrane with pin fixation |
| 6 to 7 mm | Osteotomes for ridge expansion |
| 5 to 6 mm | Allogeneic block of bone |
| 4 to 5 mm | Autogenous block of bone |
| 1 to 4 mm | Downfracture of the maxilla or titanium mesh crib (both with autogenous bone) or distraction osteogenesis |
Barrier Membranes
If the ridge is at least 8 to 10 mm in buccopalatal width and the interarch ridge relationship is appropriate, then an implant can usually be placed adequately in bone. On occasion, some grafting may be required for esthetics or to cover a few exposed threads of the implant. In this scenario, a barrier membrane with titanium reinforcement struts can be considered.8 Clinical experience and the published literature have shown that bone defects in a ridge of this width can be treated effectively without bone graft materials and using only guided bone regeneration (GBR). In fact, the results are so predictable that soft tissue management often becomes the most serious obstacle to successful use of implant-supported prosthetics in the anterior region.51
Use of barrier membranes for GBR in the maxilla, such as the Gore-Tex titanium-reinforced submerged membrane (W. L. Gore, Flagstaff, AZ), can follow a one- or two-stage approach. Embedded titanium struts allow the membrane to safely envelop the bone defect while effectively keeping the membrane off the bone (provided the titanium struts are bent appropriately and the membrane is tacked into position). If sufficient bone is available for placing the implant and primary stability is not a concern, then the membrane and implant can be placed simultaneously in a one-stage approach to treat any minor dehiscences or fenestrations. The membrane can be removed approximately 6 months later, and prosthetic treatment can commence. When local maxillary bone is insufficient for the placement of the implant because of the patient’s esthetic and functional needs, barrier membranes can be placed first to help regenerate the bone in the area of the defect. The membrane can then be removed approximately 9 months later, and the implant can be placed at a second-stage surgery. Prosthetic treatment can commence approximately 3 months after implant placement.
Particulate Graft and Membranes with Pin Fixation
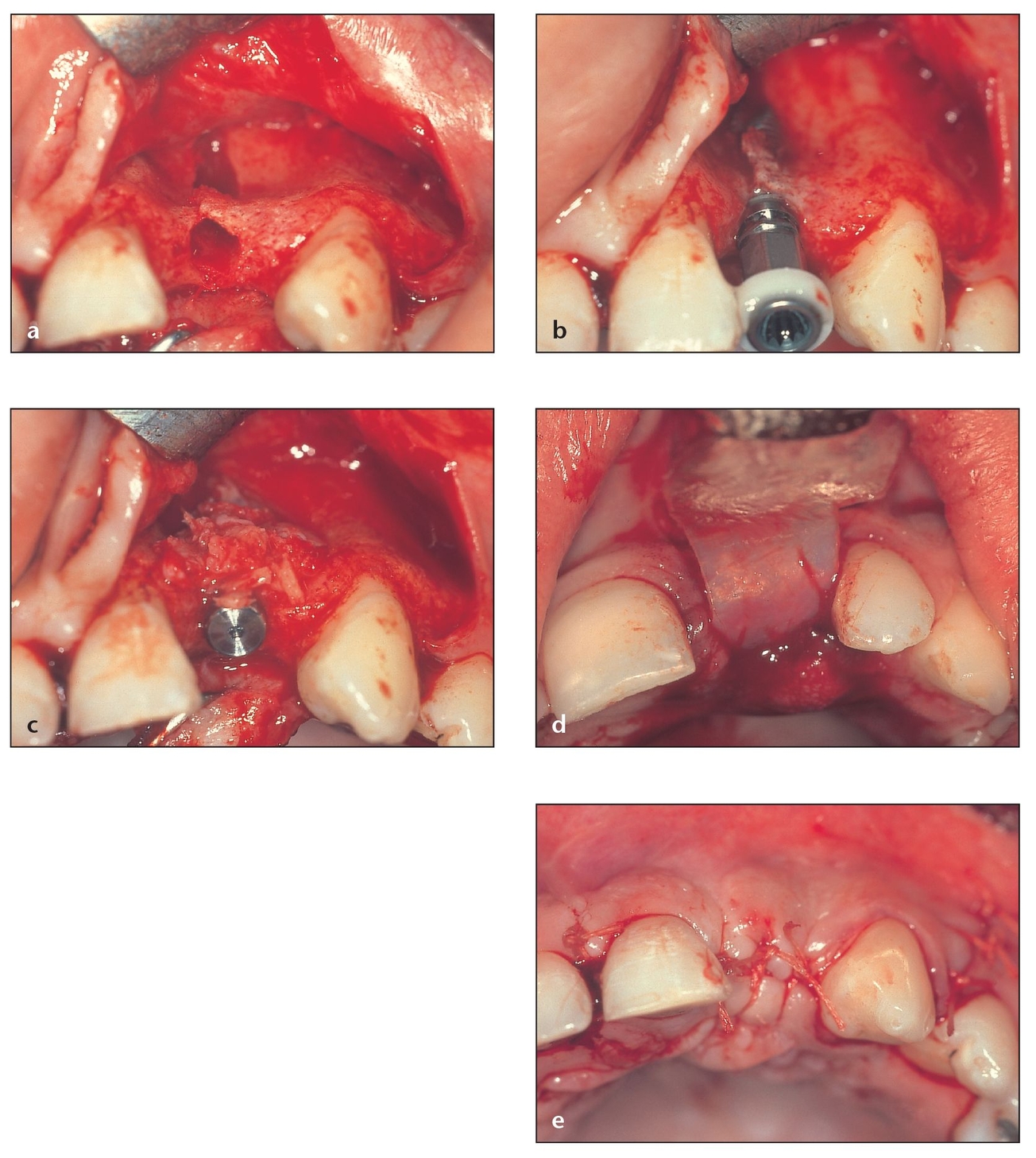
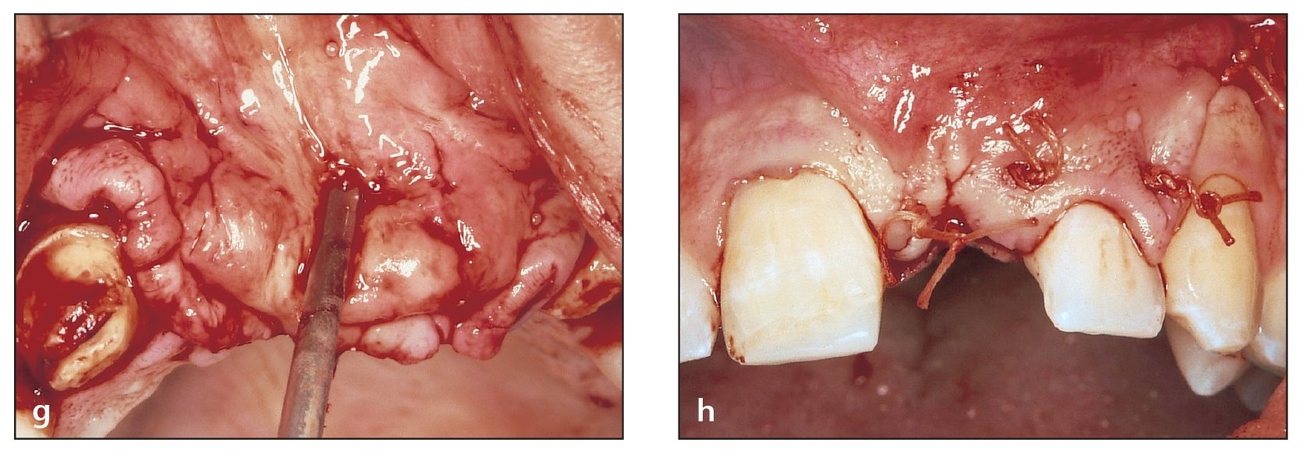
Fig 9-3 Use of barrier membranes in the maxilla following a one-stage approach.
(a) Bone dehiscence has occurred at the time of implant placement.
(b) Good stability is achieved despite implant exposure.
(c) Autogenous bone is obtained from the newly formed socket during careful drilling and is sufficient to provide good coverage in this patient.
(d) A resorbable collagen membrane is cut to fit the area and placed at the site.
(e) The flap should be placed exactly in its original position with passive closure and sutured to achieve primary closure.
If the ridge is at least 7 to 8 mm bucco-palatally, a membrane with some particulated graft material should be considered. The graft material can consist of autogenous bone, an allograft (such as demineralized or mineralized freeze-dried bone [FDBA]), or an alloplast/xenograft. Autogenous grafts regenerate bone, while alloplasts and xenografts create an osteoconductive scaffolding to facilitate bone regeneration. Allografts with collagen54, 55 or other types of resorbable membranes (eg, AlloDerm [LifeCell, Branchburg, NJ]),56, 57 including fixed bioabsorbable membranes,58 can be used for ridge augmentation (Fig 9-3). However, the literature generally reports more predictable results with nonresorbable membranes, even when placed simultaneously with implants (Fig 9-4).59 The best results have been obtained when implant placement is delayed for several weeks and when only a single implant is placed.60
Several researchers have demonstrated the effective use of GBR even in cases of more severe bone loss. In one study, human DFDBA was used with submem-branous space creation to augment bone prior to implant placement.61
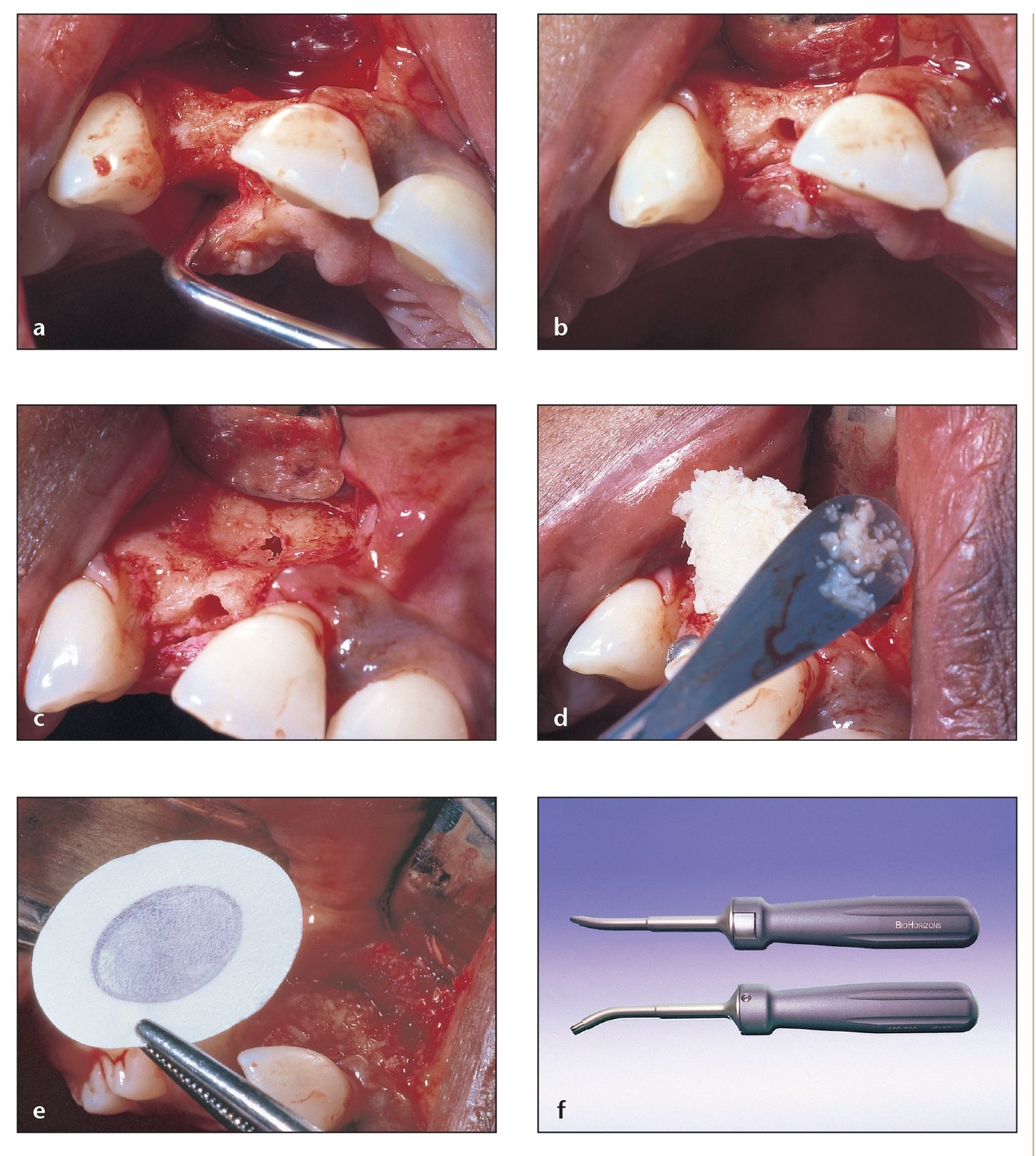
Fig 9-4 If the ridge is at least 8 to 12 mm in buccopalatal width, dehiscences can be corrected with the use of GBR membranes with or without bone graft materials.
(a) A single-tooth site in the anterior maxilla also poses a challenge in terms of bone height and width and the need to provide symmetry with the contralateral site.
(b) A single-tooth edentulous site can present the illusion of containing good bone width and height; concavities filled with connective tissue can give the appearance of having a good thickness of bone, even when palpated.
(c) Although it had the appearance of adequate bone, flap reflection reveals a deep concavity that gives way to bone dehiscence during drilling.
(d) In this patient, the placement of allogeneic particulate bone with the membrane was preferred.
(e) A Gore-Tex membrane was chosen for this patient because it provides good adaptation and coverage to the area. This non-resorbable membrane will be removed during the stage 2 procedure.
(f) The use of the Auto-Tac system (BioHorizons, Birmingham, AL) with resorbable or nonresorbable tacks is ideal to help keep the membrane immobilized.
Osteotomes for Ridge Expansion
If the ridge is at least 6 to 7 mm, then osteotomes can be used to expand and augment the ridge to provide appropriate amounts of bone for function, and the ridge can generally be modified to provide good esthetics as well.
Fig 9-5 Osteotomes can be used to expand and augment the ridge to provide appropriate bone for function. The bone is compacted and relocated rather than removed, increasing the chances of implant survival.
(a) Osteotomes of increasing diameter (0.03 to 0.06 mm) are used to create an osteotomy to accommodate a specific implant system. (From Saadoun AP, Le Gall MG. Implant site preparation with osteotomes: Principles and clinical application. Pract Periodontics Aesthet Dent 1996;8:453–463. Used with permission.)
(b) Preoperative view showing a thin ridge in the anterior maxilla missing four incisors. A flap is reflected in order to gain access and visibility.
(c) The flap is reflected and retracted to expose the ridge.
(d) A surgical template is positioned to determine the appropriate osteotomy sites.
(e) The smallest diameter drill for the particular implant system is used first to reach the correct depth for the implant, which is then selected.
(f) An osteotome of the same diameter as the drilled osteotomy (or slightly larger, eg, 0.03 mm or less) is introduced into the site. Osteotomes of larger diameter are used to reach the appropriate depth based on the size of implant to be placed. The osteotomes are either slowly rotated in by hand or by gentle tapping with a mallet. The final osteotome should approximate the implant shape and diameter.
Using osteotomes to expand a narrow anterior alveolar ridge prior to implant placement offers a particularly versatile approach for the clinician. Key advantages of the osteotome technique include minimal or no drilling, conservation of osseous tissue, improvement of bone density, and implant-to-bone interface with a denser bone. The osteotomy for an endosseous implant is created by removing bone from the site using drills of progressively larger diameter, the last of which is approximately the same diameter and length as the implant. Where dense bone predominates, this traditional drilling approach is generally appropriate. However, when poor-density bone predominates at the proposed implant site—which is most often the case in the maxilla—a more conservative approach should be used. Using osteotomes of progressively larger diameter that can be pushed or malleted into the alveolar ridge actually compacts the bone. The poor-density bone at the implant site is effectively relocated rather than removed, as it is through drilling, thus increasing the chances of an implant’s survival once it is in place (Fig 9-5). Other indications for ridge expansion include the need to improve esthetics, reduce maxillary undercuts, alter emergence angles, and match opposing landmarks.
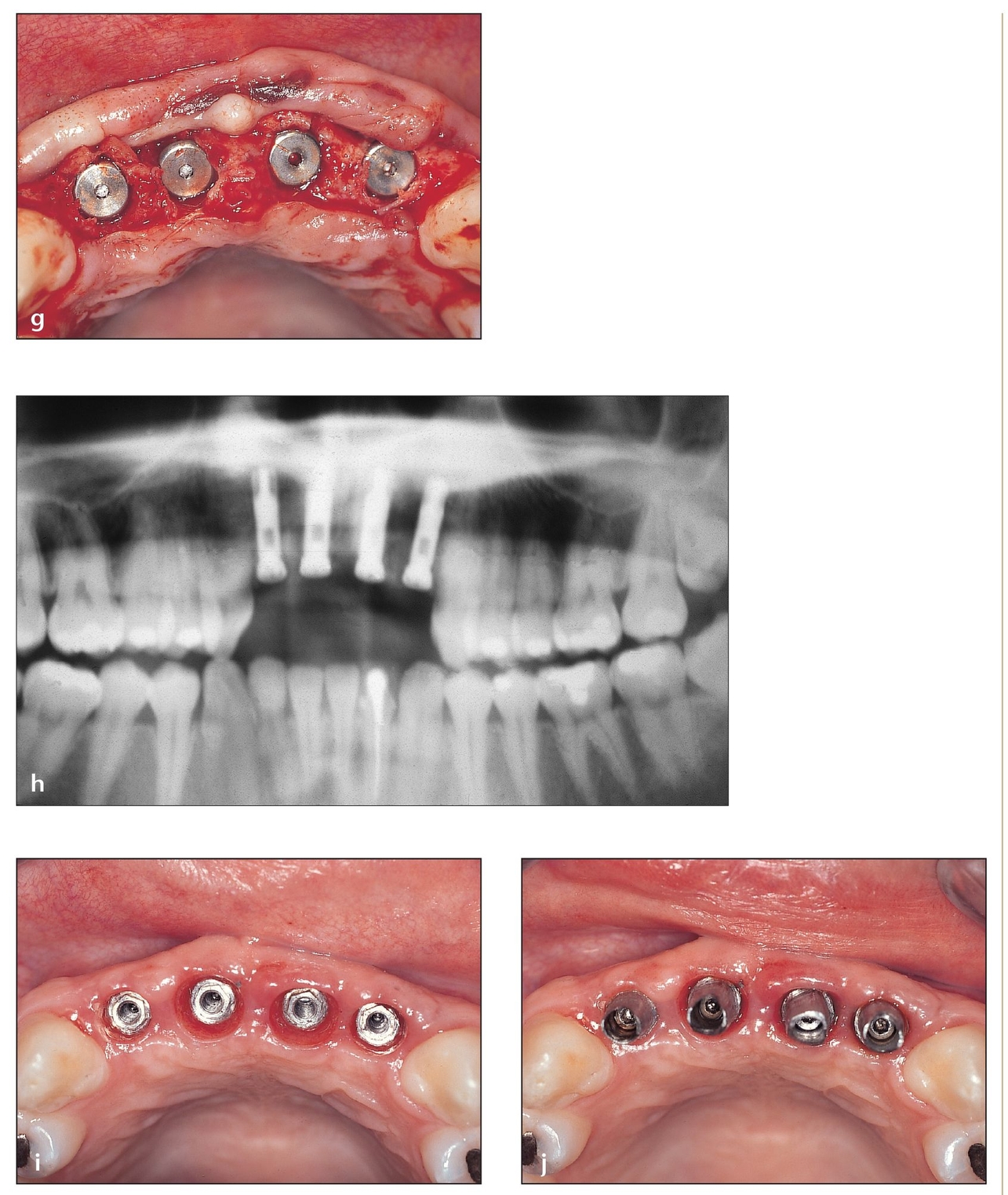
(g) The implant should have a self-tapping design. Implants of 3.75 × 15 mm are shown.
(h) Postoperative radiograph showing implants in place.
(i) Occlusal view of the ridge shows the increased buccopalatal dimension created with osteotomes.
(j) Fixed abutments are shown on the dental implant in preparation for fixed prosthetics.
Allogeneic Block Bone Grafts
If the ridge is at least 5 to 6 mm bucco-palatally, then an allogeneic/FDBA should be considered. Allografts have been used for years as viable alternatives to autogenous bone grafts. They eliminate many of the disadvantages associated with autogenous grafts, including morbidity, limited volume and dimension of bone, and harvesting time. In cases requiring good structural support, such as ridge augmentation, blocks of allogeneic bone can be used predictably to serve as a scaffolding that will eventually resorb and be replaced with host bone (Fig 9-6).
Allogeneic bone materials should contain both the collagen and mineral components of bone. For example, the Puros J-block (Zimmer Dental, Carlsbad, CA) is harvested and processed to eliminate the cells, moisture, fats, and lipids but to maintain the collagen and mineral components. In general, the criteria for using allogeneic block grafts are the same as the criteria for using autogenous block grafts described later in this chapter, with the following exceptions:
- When an allogeneic bone block is used, both the recipient site and the block graft should be decorticated.
- Barrier membranes are required with autogenous blocks of bone only if more than 50% of the surface is particulated. However, with the allogeneic block, barrier membranes are recommended in all cases.
- The autogenous block does not require rehydration; however, the J-block is rehydrated prior to use, preferably in nonactivated platelet-rich plasma (PRP).
Corticocancellous Block Grafts
If the ridge is at least 4 to 5 mm wide, then an autogenous bone block should be used.9, 62, 63, 64, 65, 66 Ridges with a crestal width of less than 6 mm typically require bone grafting prior to implant therapy. On the facial and lingual areas, at least 2 mm of bone must surround the implant. Thus, for the clinician to place a 4-mm-diameter implant, an 8- to 10-mm bone bed is required buccolingually. While alloplastic grafting materials can be used to augment the ridge in the posterior maxilla and in the mandible,67 autogenous bone from the anterior mandible or the ramus is highly recommended for augmentation of the anterior maxilla requiring more than 4 to 5 mm of additional ridge width. Corticocancellous block grafts harvested from the chin (see chapter 6) or ramus (see chapter 5) typically will provide adequate bone to overcome width deficiencies in the anterior maxilla extending up to four teeth or to increase both height and width in the areas of one to two teeth.68, 69, 70, 71
For example, a 2003 study concluded that mandibular block onlay grafts offer extremely reliable results for increasing the width of the anterior maxilla before implant placement.72 Autogenous block grafts from the chin or ramus revascularize quickly and demonstrate a relatively low rate of resorption.73 A barrier membrane may also be useful if more than 50% of the grafted area is particulate graft material. In another 2003 study reporting the use of symphyseal bone cores for vertical augmentation of the alveolar ridge, sites were additionally grafted with DFDBA in conjunction with a titanium-reinforced expanded polytetrafluoroethylene (e-PTFE) membrane.74 Results of this study also indicated an increased ridge width.
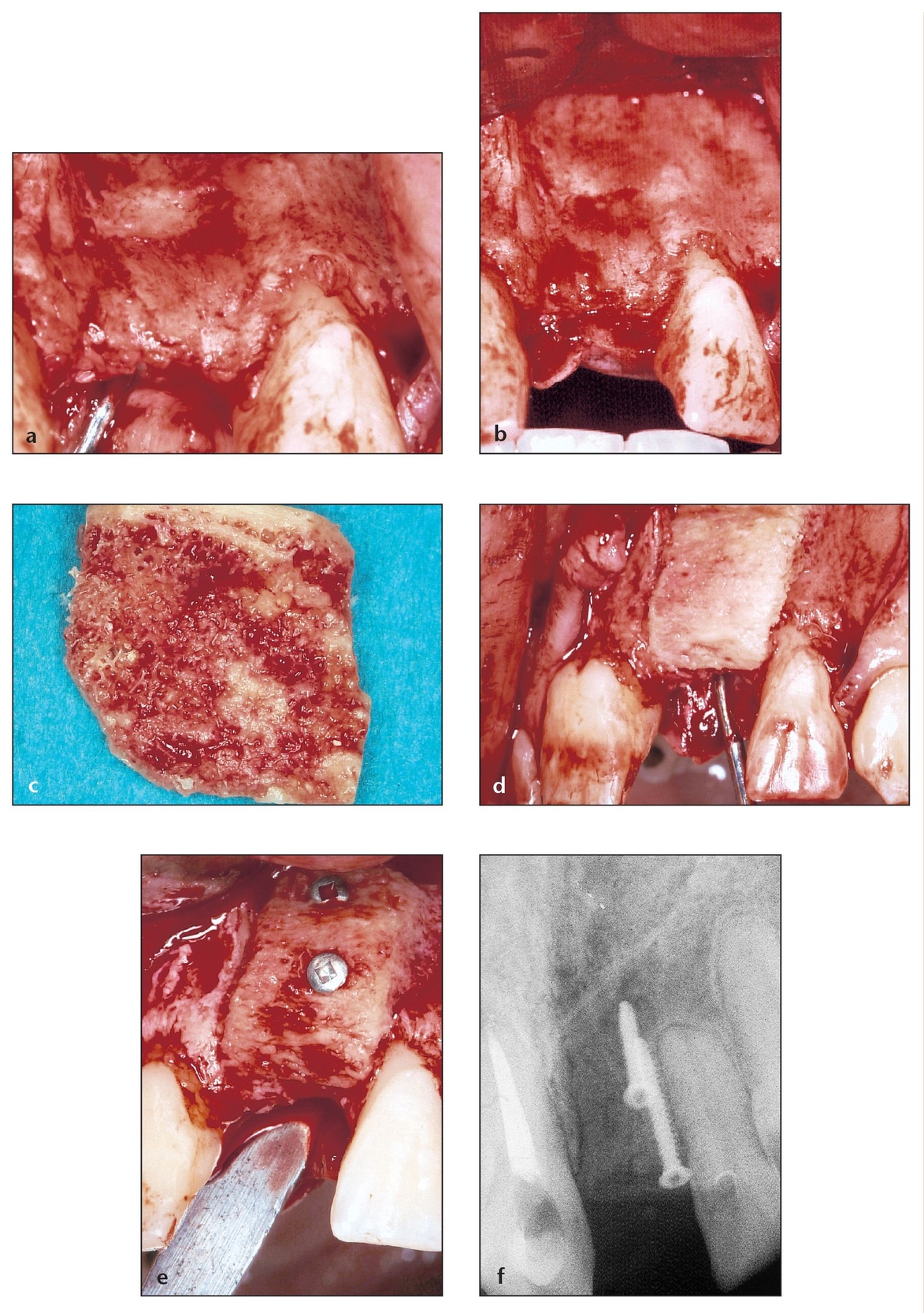
Fig 9-6 Particulate autografts, particulate allografts or alloplasts, and autogenous or allogeneic blocks are all valid options in the preplanning stage. Analyzing and evaluating the patient’s healing potential within the boundaries of the bone defect will determine the best option.
(a) Elevating a full-thickness flap with adequate release enables visualization and grafting of the defect area.
(b) The side with the ridge defect and the contralateral side need to match with respect to bony volume and anatomy.
(c) The block is sculpted for the best possible fit in the deficient area.
(d) The block is placed in the defect to check for adaptation and contoured as necessary for good fit and initial stability.
(e) Block grafts of any kind should be stabilized and screwed in place, preferably with more than one screw, to provide as much adaptation as possible to the host bone and to minimize rotation or micromovement.
(f) The retaining screws (shown radiographically) will be removed at the time of implant placement.
(g) Soft tissue dissection can provide a tension-free flap to reduce soft tissue dehiscence from adjacent muscle pull.
(h) The buccal flap is repositioned after careful dissection to permit it to be tension free. It was designed, replaced, and sutured so that both papillae remain intact.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


