10
Radiographic Analysis of Acquired Pathological Dental Conditions
This chapter will discuss the lesions that would be acquired after the eruption of the tooth. Some may have no clinical importance. In contrast, some may jeopardize the tooth and cause tooth loss. In this chapter, tooth wear, resorption, pulp calcification, and hypercementosis will be discussed.
Tooth Wear
Tooth wear is the result of three processes: (1) abrasion, (2) attrition, and (3) erosion. Tooth wear can be a challenging problem for the clinician due to its subtle early changes, confusing etiology, and the dilemma as to when or how to manage the etiology. (Harpenau et al., 2011). It is well-recognized that individual wear mechanisms rarely act alone but interact with each other. For example, potentiation of abrasion by erosive damage to the dental hard tissues is the major factor in occlusal and cervical wear (Addy and Shellis, 2006).
Attrition
Attrition is a process in which the wear of the occlusal, incisal, or interproximal surfaces of the teeth is produced by interaction and friction between maxillary and mandibular teeth. Attrition leads to the loss of enamel, dentin, or restoration, reduction in tooth length, and significant dimensional changes in facial morphology (Berry and Poole, 1976) (Figure 10.1).
Figure 10.1 Clinical image of maxillary and mandibular anteriors with attrition.
Courtesy of Dr. D. Chvartszaid.

More than 90% of the population have one or more severe attrition facets (Seligman et al., 1988). Generally, a greater attrition has been reported in males than in females (Hugoson et al., 1988; Johansson, 1992; Seligman et al., 1988). Extensive tooth wear among primitive peoples has mainly been attributed to abrasive particles in their diet. In present-day industrialized populations, other factors such as masticatory habits and parafunctions, saliva composition, dietary variables, digestive disturbances, and industrial environmental factors define the extent of attrition and tooth loss (Hugoson et al., 1988). Attrition is a physiological aging process and does not require a particular treatment, except observation. Throughout a lifetime, teeth are not lost in an irregular manner. In fact they are worn away by attrition while the human masticatory system and continuing tooth eruption maintain an efficient function as an evolving compensatory mechanisms (Begg, 1938; Newman, 1999). However, this process may become symptomatic and pathological due to bruxism where a continued dental attrition can lead to a breach of the occlusal enamel, exposing the less wear-resistant dentin. In such a case, the loss of dental hard tissue becomes accelerated and the dental pulp may become involved in extreme conditions (Ingle, 1960). A recent systematic review has found some evidence that correlates attrition and anterior spatial (van ‘t Spijker et al., 2007). However, no evidence was found suggesting that absent posterior support necessarily leads to increased attrition, or whether there is any relationship between attrition and temporomandibular dysfunction (van ‘t Spijker et al., 2007). It seems to be a correlation between attrition and self-reported bruxism. In particular, the occurrence of four clinical signs, posterior or anterior dental attrition, abfractions, and occlusal pits, was associated with self-reported bruxers (Tsiggos et al., 2008).
Clinical Findings of Attrition
Matching occlusal wear between arches, shiny wear facets on restorations, and increased risk for fracture of tooth and restorative structure are among the clinical findings of attrition (Harpenau et al., 2011).
Radiographic Findings of Attrition
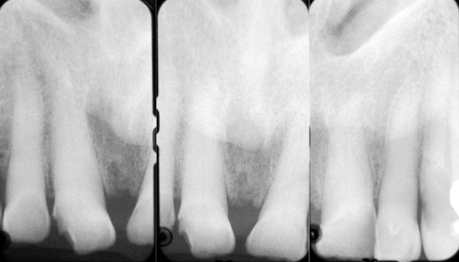
On the radiograph, attrition is viewed as a mild wear of incisal and occlusal surfaces of teeth involved. Depending on the stage of the wear, the crown looks shorter, and volume of the pulp declines due to the deposition of secondary dentine or of amorphous dentine with age (Ketterl, 1983). Widening of periodontal ligament (PDL) can be seen if the tooth is mobile and occasionally there is evidence of hypercementosis (Lam, 2009) (Figure 10.2).
Clinical Management of Attrition
Physiologic attrition does not require treatment.
Abrasion
Abrasion is a process in which tooth wear is produced by interaction and friction between teeth and other materials that leads to the loss of enamel, dentin, or restoration. Abrasion of teeth, as a result of brushing with dentifrices, was demonstrated more than a century ago (Miller, 1907). In particular, overly vigorous and improper toothbrushing in a back and forth motion with heavy pressure can cause abrasion with a V-shape wedge in the cervical area of teeth (Grippo et al., 2004, Gillette and Van House, 1980).
This type of abrasion begins apical to the cementoenamel junction and then progresses to dentin. It eventually undermines the enamel with the loss of the original cementoenamel junction (Litonjua et al., 2004). Among other causes for abrasion are improper use of dental floss and toothpicks, partial denture clasps, oral habits such as chewing tobacco, biting on hard objects (such as pens, pencils, or pipe stems), opening hair pins with teeth, and biting fingernails. Abrasion can also be seen among tailors or seamstresses who sever thread with their teeth, shoemakers and upholsterers who hold nails between their teeth, glassblowers, and musicians who play wind instruments (i.e., occupational abrasion) (Grippo et al., 2004). Similar to attrition, based on the level of wear, dentin can be exposed. This communication with the oral cavity can result in pulpal pathosis and an accompanying periapical lesion. However, in most cases, pulpal pathosis and periapical pathosis do not occur because of the ability of the pulp to lay down dentin as the pulp recedes (Meister et al., 1980).
Clinical Findings of Abrasion
Abrasional lesions can be seen usually as faciocervical concavities that are more broad than deep, in particular among those individuals with an abrasive diet and usually on prominent teeth in the arch such as canines, premolars, and mesiobuccal aspects of first molars. Abrasion may affect several teeth in a row with a “band” of abrasive damage with an increased hypersensitivity (Harpenau et al., 2011). (Figure 10.3)
Radiographic Findings of Abrasion
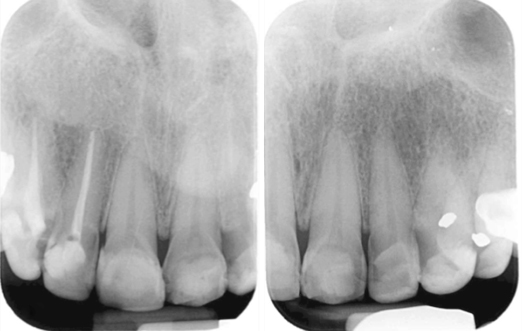
A toothbrush abrasion can be seen on radiograph as well-defined semicircular or semilunar shape radiolucent defects in cervical level of the tooth. The borders of defect show increased radiopacity. The pulp chambers appear obliterated (Lam, 2009) (Figures 10.4 and 10.5).
Figure 10.4 Radiographic image of abrasion of the cervical areas of mandibular incisors these incisor teeth. Note the obliteration of the pulp chambers and reduction in size of the root canals.
Courtesy of Dr. E. Basrani.

Figure 10.5 Radiographic image of abrasion of the cervical areas of mandibular left molars, evident from excessive and improper use of dental floss.
Courtesy of Dr. N. Singh.

Clinical Management of Abrasion
Elimination of the cause of abrasion is the priority in the management. Restorative procedure may be indicated in excessive cases.
Erosion
Erosion is a multifactorial process of dissolution of enamel and underlying dentin by acidic substances without bacterial involvement. This chemical process is irreversible, and it leaves teeth susceptible to damage due to wear over the course of a person’s lifetime (Wang and Lussi, 2010). The following factors were shown to be triggers for tooth erosion (Dietschi and Argente, 2011; Gandara and Truelove, 1999):
Clinical Findings of Erosion
The clinical appearance of dental erosion includes broad concavities and cupping on smooth surface enamel and increased incisal translucency, which can have undesirable esthetic implications (Gandara and Truelove, 1999). This type of tooth wear can be seen on nonfunctional surfaces and can result in the loss of dental anatomy such as occlusal grooves, cusps, and flat surfaces (Harpenau et al., 2011). Furthermore, loss of enamel can lead to dentin exposure and hypersensitivity, even progressing as far as resulting in pulp exposure in some extreme cases (Gandara and Truelove, 1999).
Radiographic Findings of Erosion
The findings appear as radiolucent defects on the crown with well-defined or diffused margins (Lam, 2009) (Figure 10.6).
Figure 10.6 Radiographic image of erosion of the cervical areas of maxillary incisors.
Clinical Management of Erosion
The clinical signs of dental erosion are initially subtle and the patient remains asymptomatic, unaware, and uninformed (Curtis et al., 2011). However, more advanced situations may require endodontic therapy. Therefore, early detection of the potential causes (such as part of the dietary analysis of high-risk individuals) and the prevention and modification of behavioral factors of dental erosion is an essential component of managing this condition. With restorative treatment of erosion, esthetic consequences can be addressed. However, without eliminating the cause of the erosion, the destructive process will likely to continue.
Abfraction
Abfraction (from the Latin words “ab,” or away, and “fractio,” or breaking) is the loss of cervical tooth structure caused by tensile and compressive forces during tooth flexure at a location away from loading (Figure 10.7). These biomechanical loading forces exerted on the teeth can be static, as in swallowing and clenching, or they can be cyclic as in chewing (Grippo, 1991). The clinical appearance of abfraction is a deep, narrow, V-shaped notch in the cervical area (facial aspect) which often affect a single tooth with excursive interferences or eccentric occlusal loads (Harpenau et al., 2011). There is a controversy over abfraction being a distinct clinical entity or a primary factor in cervical lesions (Litonjua et al., 2003). Regardless, abfraction might potentiate wear by abrasion and/or erosion (Addy and Shellis, 2006).
Resorption
Root resorption is the loss of dental hard tissues as a result of clastic activities that is physiological in the primary dentition and a pathologic phenomenon in the permanent dentition (Patel et al., 2010). Based on the location, root resorption can be classified to internal and external.
Internal Root Resorption
Internal root resorption is an inflammatory condition that results in the progressive destruction of the internal aspect of the root and dentinal tubules along the middle and apical thirds of the canal walls without adjunctive deposition of hard tissues adjacent to the resorptive sites (Patel et al., 2010). It involves an elaborate interaction between inflammatory cells, resorbing cells, and hard tissue structures (Ne et al., 1999). Histological findings include inflammation of pulpal tissues with the inflammatory infiltrate consisting predominantly of lymphocytes and macrophages, with some neutrophils, dilated blood vessels, and the presence of numerous, large, multinucleated odontoclasts occupying resorption lacunae on the canal walls. The coronal pulp would become necrotic with bacteria being evident either in the necrotic coronal pulp tissue or within the dentinal tubules adjacent to the lesion (Wedenberg and Zetterqvist, 1987). A prerequirement is the disruption of the odontoblast layer and predentin so that the activated clastic cells can adhere to the intraradicular mineralized dentin (Masterton, 1965). A subgroup of internal root resorption is internal replacement resorption, which is defined as the resorption of the intraradicular dentin accompanied by subsequent deposition of a metaplastic bone/cementum-like tissues instead of true dentin (Patel et al., 2010)./>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses