10
Office-based sedation
The goal of this chapter is to aid the dentist and dental hygienist in managing pain and anxiety and modifying behavior to safely complete dental procedures in patients with developmental disorders. Developmental and chronologic age both affect a patient’s ability to control his or her behavior for a dental procedure (AAPD 2007–2008; Maxwell & Yaster 1996). Young patients and severely developmentally disabled patients may require deeper levels of sedation to gain control of their behavior (Maxwell & Yaster 1996). Therefore, the dentist should consider the need for deep sedation. However, for more cooperative patients, traditional behavior management/guidance such as distraction, tell-show-do, guided imagery, topical anesthesia, and hypnosis may reduce the need for or depth of pharmacologic sedation (AAPD 2007–2008; Kennedy & Luchman 1999; Newton et al. 2003).
DEFINITIONS
Many definitions of sedation for dentistry have been used over the years. The most recent documents defining sedation and anesthesia are from the House of Delegates Meeting of the American Dental Association (ADA) in 2007 (ADA 2007a, 2007b). Clinical standards for sedation in dentistry parallel the guidelines established by the American Society of Anesthesiologists (ASA 2002). The American Academy of Pediatric Dentistry (AAPD) and the American Academy of Pediatrics (AAP) also maintain guidelines for sedation of the pediatric patient, defined as any patient under the age of 21 (AAPD 2007–2008).
The following definitions for levels of sedation are excerpted from the ADA, AAPD, and AAP guidelines (AAPD 2007–2008; ADA 2007a, 2007b):
Note: ”In accord with this particular definition, the drug(s) and/or techniques used should carry a margin of safety wide enough to render loss of consciousness unlikely. Repeated dosing of an agent before the effects of previous dosing can be fully appreciated may result in a greater alteration of the state of consciousness than is the intent of the dentist. Further, patients whose only response is reflex withdrawal from repeated painful stimuli would not be considered to be in a state of moderate sedation” (Malamed 2010).
SPECTRUM OF ANESTHESIA AND SEDATION
In 1937, Arthur Guedel, MD, introduced the concept of anesthetic signs and stages. His early work was based on the use of di-ethyl ether for general anesthesia. He showed that as patients were administered increasing quantities of ether they moved through four distinct stages. The stages represent a continuum or spectrum progressing from no sedation to general anesthesia (Douglas 1958).
Figure 10.1 Guedel’s early work.
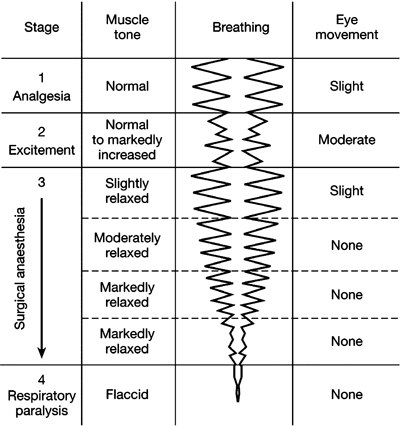
Figure 10.1 illustrates Guedel’s early work graphically. (Harrison-Calmes 2002). In stage 1, the analgesia phase, consciousness is not lost. Between stages 2 and 3, consciousness is lost. Dentists who have not been trained in the use of deep sedation and general anesthesia need to limit their practice to stage 1, the analgesia phase.
Although Guedel’s work is still tenable, it has been revised and adapted to include new drugs and techniques. This is particularly true as it relates to ambulatory sedation and anesthesia for dental procedures. The dentist must understand that as drugs are given they produce an outcome along a ”spectrum of pain and anxiety control” (Malamed 2010). Different drugs administered via different routes will produce various levels of sedation or anesthesia.
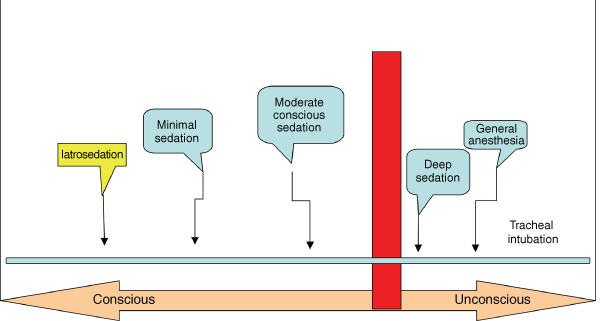
Figure 10.2 shows the spectrum. At the left there is no sedation or anesthesia. Moving right, there are levels of conscious sedation up to the vertical bar. The bar represents loss of consciousness. To the right of the bar is deep sedation/general anesthesia. It is paramount that the dentist understands where he or she is on the spectrum and where he or she wants to be.
Figure 10.2 Sedation spectrum.
Rescue
The concept of ”rescue” is essential to safe sedation. Recognizing that levels of sedation and anesthesia are along a continuum, it is paramount that the provider be able to rescue a patient from unintended entry to a more profound level of CNS depression (AAPD 2007–2008; Malamed 2010; Cote et al. 2000; Hoffman et al. 2002; AHA 2002). The ASA in their guidelines include and stress the concept of rescue during the administration of sedation by ”non-anesthesiologists” in an effort to reduce morbidity and mortality.
Because sedation is a continuum, it is not always possible to predict how an individual patient will respond. Hence, practitioners intending to produce a given level of sedation should be able to rescue patients whose level of sedation becomes deeper than initially intended. Individuals administering Moderate Sedation should be able to rescue patients who enter a state of deep sedation, while those administering deep sedation should be able to rescue patients who enter a state of general anesthesia (ASA 2002).
Sedation can also be accomplished without the use of drugs. It is known as iatrosedation. Techniques include acupressure, acupuncture, biofeedback, electronic dental anesthesia, and hypnosis (Malamed 2010). Iatrosedation may provide an alternative to traditional sedation and/or general anesthesia for patients with developmental disorders. However, for purposes of this chapter, we will focus on the use of pharmacotherapy to obtain a desired outcome.
Communication is the key to successful sedation. The dentist and dental hygienist cannot ignore the power of good communication with the patient. Knowing the patient’s developmental and chronological age will help the provider meet the patient at his or her level. There is no substitute for good verbal and nonverbal communication that is developmentally age appropriate. It has been shown that good communication has the potential to remove a patient’s fear and anxiety and allow treatment to proceed in a ”normal” fashion (Malamed 2010). More often, however, good communication facilitates the acceptance of pharmacosedation with a successful outcome.
PHYSICAL STATUS CLASSIFICATION
Dental treatment can have profound effects on both the physical and psychological ”well-being” of patients with developmental disorders. It is important that prior to any dental treatment a complete physical and psychological assessment be done. This information is necessary to provide high-quality care and prevent serious complications.
Physical and psychological assessments allow the dentist to determine if a patient will tolerate a procedure and/or determine if an alternative modality is needed. Medical and psychological histories should guide the dentist in choosing a treatment modality. Physical evaluation should include a medical history questionnaire, a physical examination, and a discussion with the patient, parent, and/or caregiver. With information collected, the dentist can establish a physical status classification and determine risk factors. Medical consults can be obtained as needed and the appropriate treatment planned, which may include pharmacosedation (Malamed 2010).
In 1962, the ASA adopted a classification system for estimating medical risk for a patient receiving general anesthesia for a surgical procedure. It is what is now referred to as the ASA Physical Status (PS) Classification System (ASA 1963). The system has remained virtually unchanged and has since been adopted for evaluation of medical risk associated with all surgical procedures regardless of anesthetic technique (Fleisher 2005; Lagasse 2002).
The ASA Physical Status Classification System (ASA 1963):
If the procedure to be performed is an emergency an ”E” is added to the above classification system (e.g., ASA PS 2E). In outpatient medical and dental settings ASA PS 5 and ASA PS 6 have been eliminated (ASA 1963).
Patients who are ASA PS 1 and 2 are generally considered appropriate candidates for minimal, moderate, or deep sedation in the dental office (AAPD 2007–2008). Most mild developmental disorders are ASA PS 2 patients. Individuals in the ASA PS classes 3 and 4 require individual consideration, particularly for moderate and deep sedation (AAPD 2007–2008; Malviya et al. 1997). Dentists are encouraged to consult with appropriate subspecialties when necessary for patients at increased risk. Remember, the ultimate responsibility and liability rest with the dentist who decides to treat or not treat.
SEDATION
The sedation of patients with developmental disorders needing oral health care represents a unique clinical challenge. Consideration must be given to such factors as the patient’s age and corresponding levels of cognitive and coping skills. Because of patient extremes in responsiveness and acceptability of treatment modalities, the intended goals and outcomes of sedation will vary depending on a host of factors. These guidelines should aid clinicians in achieving the benefits of sedation while minimizing associated risks and adverse outcomes for the patient.
The ideal sedation should:
Once the decision has been made to use pharmacosedation, the dentist must consider what drugs to use and how to administer the drug. Choosing a method for delivery to a patient with a developmental disorder will vary depending on desired level of sedation and the patient’s willingness to cooperate. Cooperative patients with developmental disorders who require less sedation often receive sedative agents via the oral route, whereas uncooperative patients with limited cognitive skills often require induction via the intra-muscular route followed by an IV to administer additional agents.
Drugs may be administered to the patient with a developmental disorder via the following routes:
Oral and rectal sedation are termed enteral sedation. The drug is administered directly into the gastrointestinal tract (GI) with systemic absorbtion occuring across the entire membrane. This is different from other routes in which drug absorption occurs directly into the systemic circulation, known as parenteral sedation.
The oral route is the most popular route used for sedation in dentistry. It has several advantages over the parenteral routes, which include acceptance by patients, low cost, ease of administration, decreased incidence of adverse reaction, and no equipment needed for delivery (Malamed 2010). However, oral sedation does have some significant disadvantages, such as reliance on patient compliance, a prolonged latent period, erratic and incomplete absorption from the GI tract, inability to titrate, inability to lighten or deepen sedation as needed, and a prolonged duration of action. With oral sedation, adding more medicine after the initial dose is usually not recommended.
The rectal route is similar to the oral route in its advantages and disadvantages. It is primarily used in diaper-age patients and patients who are either unwilling or unable to take drugs by mouth (Malamed 2010; Flaitz 1986; Jensen & Matsson 2001). The rectal route bypasses a portion of the GI tract (stomach), therefore a quicker and more profound sedation may be noticed. As with oral sedation, it is not recommended to add additional medicine after the initial dose.
Topical administration of a drug works well for nonkeratinized skin. Therefore, topical anesthetics are highly effective at relieving pain associated with intraoral injections of local anesthesia (Carr & Horton 2001). Topical applications of drugs in dentistry are usually limited to local anesthetics. With topical anesthetics there is more allergic potential (localized, not systemic) because of their benzocaine-based formulation.
Intranasal administration has become increasingly popular in pediatrics. It is easily administered to resistant, uncooperative, or precooperative patients (Malamed 2010; Fukota et al. 1993; Fuks et al. 1994; Lam et al. 2005). Although there is brief discomfort with administration, absorption is directly into the systemic circulation, making the drug rapidly bioavailable. There is reduced time to onset and total time spent in the office, when compared with oral sedation. Midazolam, a water-soluble benzodiazepine, is the most commonly used drug via the intra-nasal route (Malamed 2010; Fukota et al. 1993; Fuks et al. 1994; Lam et al. 2005; Walbergh et al. 1991). The mucosal atomization device (MAD) is the preferred method for nasal administration.
Inhalation drug administration is when gaseous agents pass from the nose or mouth to the trachea and lungs into the cardiovascular system. There are a variety of agents available for inhalational sedation and anesthesia. In dentistry, nitrous oxide/oxygen sedation is the main drug used for inhalation sedation (Malamed 2010; Jastak & Donaldson 1991). It is easily titrated to effect, with minimal side effects or complications. Disadvantages of nitrous oxide are that it is not a potent anesthetic, so there may be failure. Also, a delivery system is required with a fail-safe and scavenging system. The equipment must be calibrated annually and there needs to be adequate office ventilation to prevent chronic exposure to personnel administering the sedation.
Sublingual drugs are administered under or beneath the tongue (hypoglossal). Transmucosal drugs are delivered through mucous membranes. With sublingual and transmucosal administration, the drug enters directly into the systemic circulation, bypassing the enterohepatic system. Avoidance of the hepatic first-pass effect makes the drug rapidly bioavailable. Nitroglycerin, for relief of anginal pain, is an example of a drug commonly given via the sublingual and transmucosal route. In dentistry, benzodiazepines and opiates for sedation and pain control may be delivered via the sublingual or oral transmucosal route (Malamed 2010; Hosaka et al. 2009). This route of delivery may have limited application for the noncooperative patient, such as one with a moderate to severe developmental disorder.
Subcutaneous injection is where the drug is administered beneath the skin into the subcutaneous tissue. The rate of absorption into the CVS is directly proportional to the vasculature in the area of injection. The slow rate of absorption may limit the usefulness in dentistry.
The intra-muscular route is a parenteral technique in which the drug is injected directly into the muscle. Advantages include rapid onset and rapid onset of maximal clinical effect. Disadvantages are prolonged deep sedation, possible injury to tissues at injection site, and overdose. This route of administration is often not predictable and does not allow for titration to effect. Ketamine, a dissociative anesthetic, is the most commonly used drug via the intramuscular route and is often used for sedation and induction of the uncooperative patient with a developmental disorder (Sinner & Graf 2008). Skilled and experienced anesthesia providers familiar with anatomy may inject ketamine through the clothing of uncooperative patients with developmental disorders.
The intravenous route of drug administration represents the most effective method of predictable adequate sedation for most patients (Malamed 2010). Advantages to this route include rapid onset with short duration of latent period, and a shortened recovery. Disadvantages include complications at venipuncture site and risk for overdose. IVs may often be difficult to obtain on patients with developmental disorders. Many drugs given via IV do not have reversals; therefore the dentist must be prepared to manage deeper sedation and other complications such as allergic reactions, which may not be seen with other less effective modes of delivery (Malamed 2010).
A variety of drugs are available for sedation of the patient with a developmental disorder. These primarily include nitrous oxide/oxygen inhalation sedation, benzodiazepines, sedative hypnotics, and opioids. Table 10.1 lists available drugs for sedation.
Table 10.1 Commonly Used Drugs for Sedation of the Patient with a Developmental Disorder
| Inhalation Agents Nitrous Oxide/Oxygen Sedation |
Barbiturates Methohexital Sodium Thiopental |
| Benzodiazepines Diazepam Midazolam Lorazepam Triazolam |
Hypnotics Chloral Hydrate Alpha Agonists Clonidine |
| Opioid Agonists Fentanyl Morphine Meperidine Alfentanil, Sufentanil and Remifentanil* |
Dexmedetomidine Antihistamines Hydroxyzine Diphenhydramine Promethazine |
| Dissociative Anesthetics Ketamine* |
Anticholinergics Atropine |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


