Chapter 10
Maxillofacial surgery
Contents
Relevant sections; Oral cancer p. 416 , neck lumps p. 442 , TMJ p. 446 , Salivary glands p. 420, Clefts p. 170 , orthognathic surgery p. 168 Preprosthetic surgery p. 330 & p. 388.
Principal sources and further reading D. Mitchell 2006 An Introduction to Oral and Maxillofacial Surgery, OUP. J. Watkinson 2000 Head & Neck Surgery, Butterworth-Heinemann. ACS 2004 ATLS Core Course Manual. M. Yaremchuk 1992 Rigid Fixation of the Craniomaxillofacial Skeleton, Butterworth-Heinemann. J. Shah 2003 Oral Cancer, Dunitz. R. Cawson 1997 Pathology and Surgery of the Salivary Glands, Isis Medical Media. K Wolfe, F Holzle. 2005 Raising of Microvascular Faps, Springer. B. Jones 2008 Facial Rejuvenation Surgery, Mosby. L. Peterson 2004 Contemporary Oral and Maxillofacial Surgery, Mosby. Personal experience.
In general, maxillofacial surgery is a postgraduate subject which has evolved from oral surgery, with foundations in medicine, dentistry, and surgery. It is included here as an introduction to students, an aide-mémoire for junior hospital staff, and a guide for those who will be referring patients.
Advanced trauma life support (ATLS)
ATLS
is a system providing one safe way of resuscitating a trauma victim. It was first conceived in Nebraska, subsequently developed by the ACS, and has now reached international acceptance. It is not the only approach but it is one which works. It is highly recommended.
Trauma deaths
have a trimodal distribution. The first peak is within seconds to minutes of injury. The second is within the first hour, the ‘golden hour’, and is the area of main concern. The third is days to weeks later but may reflect management within the golden hour.
The core concept
behind ATLS is the primary survey with simultaneous resuscitation, followed by a secondary survey leading to definitive care.
Primary survey
This uses the mnemonic ABCDE on the basis of identifying and treating the most lethal injury first.
If all these can be established and monitored parameters are normalized, the patient’s chances of living are optimized.
X-rays
At this stage obtain a chest and pelvis film in the resuscitation room. Cervical spine film may help but cervical spine should remain immobilized until fully assessed if mechanism of injury suggests spinal trauma.
Reassess the ABCs
If all is stable move to the secondary survey, which is a head-to-toe examination of the patient. It is at this stage only that specific non-immediately life-threatening conditions should be identified and dealt with in turn.
Maxillofacial injuries
Other than those with a direct effect on the airway or cervical spine, or causing exsanguinating haemorrhage, should not be dealt with until the ABCs have been completed and this question should be asked of all referring doctors prior to accepting responsibility for a patient. Remember to exclude intracranial, visceral, and major orthopaedic injuries.
While ATLS is designed primarily for front-line physicians, modified courses for dental graduates are available, and strongly recommended to anyone who may undertake care of the trauma patient.
Primary management of maxillofacial trauma
The first consideration is whether the patient has suffered polytrauma, which may have multiple and life-threatening ramifications, or, as is more commonly the case, trauma confined to the face. In the former the prime concern is keeping the patient alive, and the maxillofacial injuries can await Rx (p. 452). Remember that isolated facial injuries rarely cause sufficient bleeding to induce hypovolaemic shock. Ask yourself: Can they see?
Airway
The brain can tolerate hypoxia for ~3min. Most conscious patients can maintain a patent airway if the oropharynx is cleared. Give all traumatized patients maximal O2 initially. Oral airways are not tolerated unless patient is unconscious. Nasopharyngeal airways are only of value if they can be inserted safely and kept patent. If the patient is unconscious and the airway is obstructed they should be intubated. If this is not possible, an emergency airway can be maintained by cricothyroid puncture with a wide-bore cannula. Long-term security of the airway can be achieved by surgical cricothyroidotomy as an emergency, or tracheostomy as a planned operation. Conscious patients with severe isolated facial trauma maintain their airway by sitting leaning forward; let them.
Cervical spine injuries
Until these are excluded, the patient should be immobilized; must balance with need to remove from spine boards ASAP (painful, prevent pressure sores). Use common sense to decide between immobilization and sitting leaning forward.
Bleeding
As above. Gunshot wounds and lacerated major vessels are exceptions which can cause extensive bleeding. Specific techniques to control naso- and oropharyngeal bleeding are: bilateral rubber mouth props to immobilize the maxilla; bilateral balloon catheters passed into the post-nasal space, inflated then pulled forward; and bilateral anterior nasal packs.
Scalp wounds
Can exsanguinate children; control with pressure and heavy full thickness sutures.
Head injuries
The main cause of death and disability in patients with isolated maxillofacial trauma. Assessment: p. 456. Do no further harm.
CSF leaks
Facial and skull # can create dural tears, leading to CSF rhinorrhoea (from the nose) or otorrhoea (from the ear). Although controversial, prophylactic antibiotics are used by many. A combination penicillin in high dose is often used, despite the fact that conventional antibiotics do not cross the healthy blood–brain barrier in adequate levels, the rationale being that the blood–brain barrier is damaged in these cases. It was the concern that low levels of antibiotic in the CSF would only suppress signs of meningitis whilst selecting resistant organisms that prompted influential recommendations against prophylaxis.1
Tetanus immunity
If in doubt give tetanus toxoid.
Analgesia
May not be needed. Avoid opioids if possible as they interfere with neuro-observations. If needed, use diclofenac 75mg IM bd or codeine phosphate 60mg IM 6 hourly.
Patients to admit
Any question of danger to the airway, skull #, history of unconsciousness, retrograde amnesia, bleeding, middle 1/3 #, mandibular # (except when very simple), malar # if +ve eye signs, children, and those with domestic or social problems. If in doubt admit. Place on, at least, initial hourly neurological observations (most will need 1/4 hourly obs initially). IV access and antibiotic. If not admitting, give the patient a head-injury card.
If teeth have been lost ensure they are not in the chest (CXR) or soft tissues.
X-rays
Assessing head injury
 All patients with recent facial trauma warranting hospital admission need at least initial assessment for head injury.
All patients with recent facial trauma warranting hospital admission need at least initial assessment for head injury.
Change in the level of consciousness is the earliest and most valuable sign of head injury.
A combination of the following is generally used.
Glasgow coma scale (GCS)
Eyes open
| • spontaneously | 4 |
| • to speech | 3 |
| • to pain | 2 |
| • do not open | 1 |
Best verbal response
| • orientated | 5 |
| • confused | 4 |
| • inappropriate | 3 |
| • incomprehensible | 2 |
| • none | 1 |
Best motor response
| • obeys commands | 6 |
| • localizes pain | 5 |
| • normal flexion | 4 |
| • abnormal flexion | 3 |
| • extension | 2 |
| • none | 1 |
Pulse and BP
↓ pulse and ↑ BP is a late sign of ↑ intracranial pressure.
Pupils
Measure size (1–8mm) and reaction to light in both pupils.
Respiration
↓ rate is a sign of raised intracranial pressure.
Limb movement
| Indicate | normal mild weakness severe weakness extension no response |
for arms and legs (record right and left separately if there is a difference).
CT scan
The definitive investigation. However, patients must never be transferred before correcting hypoxia and hypovolaemia.
Using GCS
Severe head injury &/or deterioration = call for help.
One accepted method of categorizing head-injured patients by severity using GCS is:1
| Severe | <8 |
| Moderate | 9–12 |
| Minor | 13–15 |
In addition:
A severe head injury is present if the following are seen:
Subtle signs of deterioration include:
A GCS of <6 in the absence of drugs has a dismal prognosis.
A change in GCS of 2 or more is significant. Beware changes in monitoring staff!
Optimizing outcome
You are preventing 2° brain injury:
Mandibular fractures
These are the commonest # of the facial skeleton (Figure 10.1). Most are the result of fights and road traffic accidents (the former appear to be increasing whereas the latter are decreasing as a result of seat belts, etc.). Rarely, they may be comminuted with hard and soft tissue loss, e.g. gunshot wounds.

Fig. 10.1 Malocclusion and abnormal mobility are pathognomonic of a fractured mandible.
Classification
The most useful is based on site of injury: dento-alveolar, condyle, coronoid, ramus, angle, body, symphyseal, or parasymphyseal. Further subclassification into unilateral, bilateral, multiple, or comminuted aids Rx planning. In common with all # they can be grouped into simple (closed linear #), compound (open to mouth or skin), pathological (# through an area weakened by other pathology), or comminuted; again, this influences Rx.
Muscle pull
Pull on # segments renders the # favourable or unfavourable depending on whether or not the # line resists displacement. This is of less importance than recognizing the # and its associated injuries.
Common
# Condylar neck # are commonest and range from easiest to most difficult. Often found with a # of the angle or canine region of the opposite side of the jaw. Rarely, bilateral condylar # is found with a symphyseal #—‘guardsman’s #’ from falling on the point of the chin. Angle # usually occurs through wisdom-tooth socket, and body # commonly through canine socket.
Diagnosis
History of trauma. Ask if the patient can bite their teeth or dentures together in the manner which is normal to them. Inability to do this and a lingual mucosal haematoma is pathognomonic of a mandibular #. Look at the face; there is usually bruising and swelling over the # site and sometimes lacerations. If the # is displaced, there may be gagging on the posterior teeth and the mouth hangs open. The saliva is usually bloodstained. The patient may complain of paraesthesia in the distribution of the IDN. Gentle palpation over the mandible will reveal step deformities, bony crepitus, and tenderness. All have trismus.
Examination of the mouth
May reveal broken teeth or dentures which should be removed. Suction the mouth to clean away blood clots prior to examining both the buccal and lingual sulcus. Look for step deformities in the occlusion, and examine the teeth. Palpate for steps in the lingual and buccal sulcus. If  is uncertain it is sometimes worth trying to elicit abnormal mobility across the suspected # site, using gentle pressure. In cases where you are very unsure, place one hand over each angle of the mandible and exert gentle pressure; this will produce pain if there is a #, even if it is only a crack #. Never perform this if you have proved otherwise that there is a #.
is uncertain it is sometimes worth trying to elicit abnormal mobility across the suspected # site, using gentle pressure. In cases where you are very unsure, place one hand over each angle of the mandible and exert gentle pressure; this will produce pain if there is a #, even if it is only a crack #. Never perform this if you have proved otherwise that there is a #.
X-rays
DPT and PA mandible are the essentials. Right and left lateral obliques if DPT is unobtainable. Rotated PA (helpful for # between the symphysis and canine region), IO periapicals, occlusal, high DPT, or reverse Townes for condyles, and CT are all second-line investigations which may help.
Preliminary Rx
(p. 454) Most patients will be admitted to hospital, nursed sitting up and leaning forward as this is the most comfortable position. Barrel bandages are a waste of time. Keep nil by mouth and maintain hydration by IV crystalloid. Compound # need antibiotics. Assess need for analgesia; LA, temporary immobilization with circumdental wire (bridle wire), parenteral NSAIDs, or opioids may be needed.
Mid-face fractures
The mid-facial skeleton is a complex composite of fine fragile bones, which rarely # in isolation. It forms a detachable framework which protects the brain from trauma. Severe trauma can move the entire mid-face downwards and backwards along the base of the skull, lengthening the face and obstructing the airway (clot and swelling exacerbates this). Most conscious patients, however, can compensate for this. # of the cribiform plate of the ethmoids can lead to dural tears and CSF leak (p. 454).
Orbit
The globe and optic nerve are well-protected by the bony buttress of the orbit. Most # lines pass around the optic foramen; however, swelling can cause proptosis. Late changes can include tethering and enopthalmos. Retrobulbar haemorrhage is an arterial bleed behind the globe following trauma. It presents as a painful, proptosed eye with decreasing visual acuity, and is a surgical emergency. The clot must be decompressed and evacuated. Medical management with mannitol 20% 2g/kg, acetazolamide 500mg and prednisolone at least 1mg/kg all IV may help while theatre is being arranged.
Bleeding
Severe bleeding is rare, but severe mid-facial trauma may lacerate the 3rd part of the maxillary artery, resulting in profuse bleeding into the nasopharynx which requires anterior and posterior nasal packs and possibly direct (endoscopic) ligation.
Classification
Mainly based on the experimental work of Rene Le Fort. Le Fort I # detaches the tooth-bearing portion of the jaw via a # line from the anterior margin of the anterior nasal aperture running laterally and back to the lower ⅓ of the pterygoid plate. Le Fort II detaches the true mid-face in a pyramidal shape (see Figure 10.2). Le Fort III detaches the entire facial skeleton from the cranial base, as Figure 10.2.
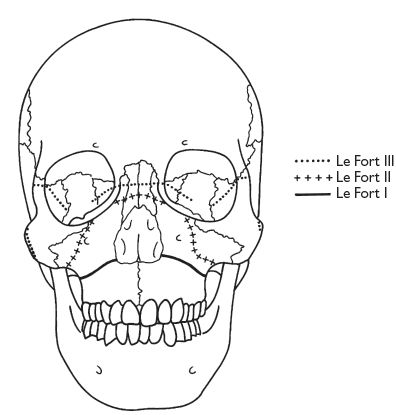
Fig. 10.2 Each line represents a different fracture line although these lines are in reality more often produced surgically, trauma being less predictable.
Diagnosis
Le Fort I may occur singly or associated with other facial #. The tooth-bearing portion of the upper jaw is mobile, unless impacted superiorly. There is bruising in the buccal sulcus bilaterally, disturbed occlusion, and posterior ‘gagging’ of the bite. Grasp the upper jaw between the thumb and forefinger anteriorly, place thumb and forefinger of other hand over the supraorbital ridges, and attempt to mobilize the upper jaw to assess mobility. Spring the maxillary teeth to detect a palatal split. Percussion of the upper teeth may produce a ‘cracked cup’ sound. Le Fort II and III # produce similar clinical appearances; namely, gross oedema of soft tissues, bilateral black eyes (panda facies), subconjunctival haemorrhage, mobile mid-face, dish-face appearance, and extensive bruising of the soft palate. Look for a CSF leak and assess visual acuity. Le Fort II # may also show infra-orbital nerve paraesthesia and step deformity in the orbital rim. Peculiar to Le Fort III # are tenderness and separation of the frontozygomatic suture, deformity of zygomatic arches bilaterally, and mobility of entire facial skeleton.
X-rays
Occipito-mental 10° and 30°, submento-vertex, lateral skull, postero-anterior skull only if C-spine is confirmed to be intact. Otherwise secure C-spine and await CT scan as the definitive imaging technique.
Preliminary Rx
as pp. 452, 454; definitive Rx, p. 464.
Nasal and malar fractures
Malar (or zygoma) #
A common and easily missed injury, usually the result of a blow with a blunt object (e.g. fist). The malar forms the cheekbone and resembles a four-pointed star on occipito-mental X-ray. The ‘star’ points to the maxilla (orbital margin and lateral wall of antrum), frontal bone, and temporal bone. # can involve the arch alone or the whole malar, which may or may not be displaced. The nature of the displacement is of value in planning the Rx.
Diagnosis
From history, examination, and X-ray. Bruising around eye with subconjunctival haemorrhage (unilateral) (Figure 10.3). Diplopia, a step deformity of the orbital rim, sometimes paraesthesia of the infra-orbital nerve, limitation of lateral excursion of the mandible on mouth opening, and unilateral epistaxis. There is often tenderness on palpation of the zygomatic buttress IO and usually some flattening of the cheek prominence.

Fig. 10.3 Presence of subconjunctival haemorrhage (seen here medially and laterally) is usually indicative of underlying fracture.
Orbital floor #
Main signs are those of the malar # (or middle 1/3 # if that is the presenting injury). Late signs are enopthalmos and tethering of inferior rectus, causing diplopia in upwards gaze. Also known as orbital blow-out #; fat and muscle herniates through the thin orbital floor (a similar injury can occur to the medial wall). Classically, seen on X-ray as ‘hanging drop sign’ (radiolucent fat hanging into antrum) (Figure 10.4). Confirm with coronal CT scan. Lateral wall &/or roof # are much less common.

Fig. 10.4 A coronal CT scan demonstrating prolapse of the contents of the left orbit into the maxillary antrum—the ‘hanging drop’ of a blow out fracture.
Nasal #
Simple nasal trauma is seen by a number of different specialities and considered rather trivial. This is unfair to the patients, as long-term results of nasal # leave a lot t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


