1 Introduction
Anatomy
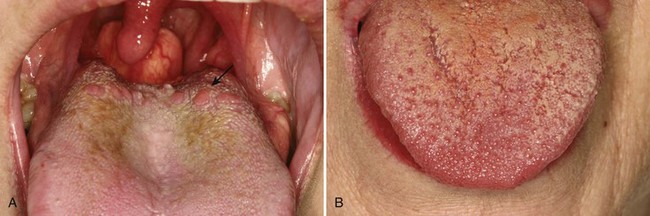
The oral mucosa varies clinically and histologically from site to site, and can be divided into keratinized and nonkeratinized mucosa (Fig. 1-1). Knowledge of clinical aspects of oral disease must be correlated with oral anatomy: for example, recurrent aphthous ulcers occur primarily on the nonkeratinized mucosa, whereas recurrent herpes simplex infections occur almost exclusively on the keratinized mucosa in immune-competent patients. The tongue dorsum but not ventrum is specialized for gustatory, masticatory, and deglutition functions. Taste buds are present within fungiform (dorsum), circumvallate (8 to 14 on the posterior dorsum), and foliate (posterior lateral tongue) papillae but not within filiform papillae (Fig. 1-2). The oral mucosa contains no submucosa per se because there is no muscularis mucosa or any other clearly recognizable histologic landmark that separates mucosa from submucosa. As such, the terms papillary, superficial, and deep lamina propria are preferable to submucosa. In general, the epithelium of the oral cavity is much thicker than that of the skin (Table 1-1; Figs. 1-3 to 1-9). Muscle is present fairly superficially on the tongue and slightly deeper on the buccal and labial mucosa. Minor salivary glands are predominantly mucous, although serous acini and demilunes are frequently seen (Fig. 1-10); they are present everywhere in the mouth except on the attached gingiva and tongue dorsum. Serous salivary glands with a smaller mucous component are frequently encountered on the anterior ventral (glands of Blandin-Nuhn) and posterior lateral and dorsal (glands of von Ebner) tongue, often invested in muscle. Lingual tonsils are located on the posterior dorsum and posterior lateral tongue.
| Site | Appearance |
|---|---|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses