Chapter 1
Essentials of infection control
WHY DO WE NEED INFECTION CONTROL IN DENTISTRY?
Dentists are exposed to a wide variety of potentially infectious microorganisms in their clinical environment. The transmission of infectious agents from person to person or from inanimate objects within the clinical environment resulting in infection is known as cross-infection.
The protocols and procedures involved in the prevention and control of infection in dentistry are directed to reduce the possibility or risk of cross-infection occurring in the dental clinic, thereby producing a safe environment for both patients and staff.
All employers have a legal obligation under the Health and Safety at Work Act 1974 to ensure that all their employees are appropriately trained and proficient in the procedures necessary for working safely. They are also required by the Control of Substances Hazardous to Health (COSHH) Regulations 2002 to review every procedure carried out by their employees which involves contact with a substance hazardous to health, including pathogenic microorganisms. Employers and their employees are also responsible in law to ensure that any person on the premises, including patients, contractors and visitors, is not placed at any avoidable risk, as far as is reasonably practicable.
Thus, the concept of the risk of cross-infection is an important one in dentistry. We do not deal in absolutes, but our infection control measures are directed towards reducing, to an acceptable level, the probability or possibility that an infection could be transmitted. This is usually measured against the background infection rate expected in the local population; i.e. the patient or dental operative system is placed at no increased risk of infection when entering the dental environment. Infection control guidance in dental surgery has developed from an assessment of the evidence base, consideration of the best clinical practice and risk assessment (Figure 1.1).
How we manage the prevention of cross-infection and control the risk of spread of infection in the dental clinic is the subject of this book.
Figure 1.1 The basis of the development of infection control guidance in dental surgery.
RELATIVE RISK AND RISK PERCEPTION
Risk has many definitions and is perceived by the dental profession and the public in different ways which can have an impact on the perception of the public and dental staff as to how safe it is in the dental clinic. For example, risks which are under personal control, such as driving a car, are more acceptable than the risks of travelling by aeroplane or train. Thus, the public often perceives travelling by car to be safer than by air even though the accident statistics do not support this perception. Unseen risks such as infection and particularly those with frightening consequences such as AIDS or MRSA are predictably most alarming to the profession and the public. Risks can be clinical, environmental, financial, economic or political, as well as those affecting public perception and reputation of the dentist.
What makes risks significant? There are a number of criteria which make risks significant and worthy of concern:
- Potential for actual injury to patients or staff
- Significant occupational health and safety hazard
- The possibility of erosion of reputation or public confidence
- Potential for litigation
- Minor incidents which occur in clusters and may represent trends
Understanding what is implied by the term hazard is important when we consider the control of infection. This may be defined as a situation, or substance, including microorganisms, with the potential to cause harm. Thus, risk must take into account not only the likelihood or probability that a particular hazard may impact on the patient or dental staff but the severity of the consequences if it did impact on people.
RISK ASSESSMENT AND THE MANAGEMENT DECISION-MAKING PROCESS
It is the role of managers of dental practices to manage risk. The Management of Health and Safety at Work Regulations 1999 requires employers to carry out a risk assessment as an essential part of a risk management strategy. Infection control is an application of risk management to the dental clinical setting.
Risk control in dentistry is a single-tier approach in which all patients are treated without discrimination as though they were potentially infectious. This approach was previously referred to as universal precautions and has been replaced by standard precautions which treat all body fluids, with the exception of sweat, as a source of infection and include a series of measures and procedures designed to prevent exposure of staff or patients to direct contact with infected body fluids. Specifically, dental health care workers (HCWs) should provide barriers to exchange of blood, saliva and gingival fluid between operator and patient and patient and operator.
Decisions made within an organisation, and within practice, should take into account the potential risks that could directly or indirectly affect a patient’s care. If risks are properly assessed, the process can help all health care professionals and organisations set their priorities and improve decision-making to reach an optimal balance of risk, benefit and cost. If dental teams systematically identify, assess, learn from and manage all risks and incidents, they will be able to reduce potential and actual risks, and identify opportunities to improve health care.
Risk assessment has the following benefits for delivery of dental health care:
- Strives for the optimal balance of risk by focusing on the reduction or mitigation of risk while supporting and fostering innovation, so that greatest returns can be achieved with acceptable results, costs and risks
- Supports better decision-making through a solid understanding of all risks and their likely impact
- Enables dentist to plan for uncertainty, with well-considered contingency plans which cope with the impact of unexpected events and increase staff, patient and public confidence in care that is delivered
- Helps the dentist comply with published standards and guidelines
- Highlights weakness and vulnerability in procedures, practices and policy changes
HOW TO PERFORM A RISK ASSESSMENT IN A DENTAL PRACTICE
A risk assessment in dental practice involves five stages:
Stage 1: Look for the hazards
- Divide your work into manageable categories
- Concentrate on significant hazards, which could result in serious harm or affect several people
- Ask your employees for their views; involve the whole dental team
- Separate activities into operational stages to ensure that there are no hidden hazards
- Make use of manufacturers’ datasheets to help you spot hazards and put risks in their true perspective
- Review past accidents and ill-health records
Stage 2: Who might be harmed?
- Identify all members of staff at risk from the significant hazard
- Do not forget people who only come into contact with the hazard infrequently, e.g. maintenance contractors, visitors, general public and people sharing your workplace
- Highlight those persons particularly at risk who may be more vulnerable, e.g. the young, people with disabilities, inexperienced or temporary workers and lone workers
Stage 3: Evaluate the level of risk
- The aim is to reduce all risks to a low level
- Determine for each significant hazard if the remaining risk, after all precautions have been taken, is high, medium or low
- Concentrate on the greatest risks first
- Examine how work is actually carried out and identify failures to follow procedures or practices
- Need to comply with legal requirements and standards
- The law says that you must do what is reasonably practical to keep your workplace safe
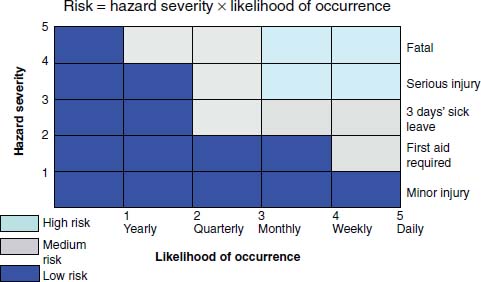
A numerical evaluation of risk can be made to help prioritise the need for action and allow comparison of relative risk. Risk is equal to severity multiplied by likelihood. Assign a score of 1–5 for each, with a total value of 16–25 equating to high risk, 9–15 to medium risk and >8 to low risk (Figure 1.2).
Figure 1.2 Graph showing how hazard severity and likelihood of occurrence are related to risk.
Stage 4: Record your findings
Record the significant findings of your assessment and include significant hazards and important conclusions.
Information to be recorded:
- Activities or work areas examined
- Hazards identified
- Persons exposed to the hazards
- Evaluation of risks and their prioritisation
- Existing control measures and their effectiveness
- What additional precautions are needed and who is to take action and when
Stage 5: Review your assessment
Risk assessment is a continuing process and must be kept up to date to ensure that it takes into account new activities and hazards, changes in processes, methods of work and new employees.
You must document your findings but there is no need to show how you did your assessment, provided you can show that a proper check was made and you asked who might be affected, and that you dealt with all the obvious significant hazards taking into account the number of people who could be involved, that the precautions taken are reasonable, and that the remaining risk is low.
HIERARCHY OF RISK MANAGEMENT CONTROL
Following a risk assessment is necessary to implement a plan to control the observed risk. The plan of action must set out in priority order what additional controls are necessary, and aim to reduce risks to an acceptable level and comply with relevant legal requirements. You must also establish a reasonable time scale for comple/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses