Chapter 1
Defining Success and Failure
Aim
To review the methods of evaluating the outcome of endodontic treatment, explain the reasons for reported variations of success rate and describe the criteria for success and failure.
Outcome
After studying this chapter, the practitioner should have an understanding of how the concepts of success and failure are defined, the process of evaluating treatment outcome, and the principles of justifying remedial treatment.
Terminology
Endodontic treatment is used as a generic term to cover the whole spectrum of pulp and periapical therapy. Root canal treatment describes a specific procedure for treating the dental pulp when irreversible damage has occurred, or when vitality is compromised by disease or injury. Although there is a distinction between the terms, in this book, endodontic treatment and root canal treatment are used interchangeably, as in common usage.
Introduction
It has been said that there is no such thing as failure, just different degrees of success. There is some truth in this statement and it highlights the difficulties of defining success and failure objectively. Therefore, before looking at how to manage endodontic failure, it is pertinent to consider how failure may be defined.
The Strindberg Concept
The traditional, standard notion of success and failure is based on the stringent criteria encapsulated by the so-called “Strindberg Concept”. According to Strindberg (1956) the only satisfactory postoperative outcome, after a predetermined postoperative period, is clinically a symptom-free tooth and radiologically the appearance of a normal periapex. Put simply, “success” is defined as the lack of visible signs of disease while “failure” is defined as the presence of any signs or symptoms indicating disease. Such a concept is very “black and white”, with a definite cut-off point.
The “Strindberg Concept” is based exclusively on our knowledge of the disease process and represents an “ideal” concept of disease. It can, however, be perceived as being too dogmatic and inflexible for use in everyday clinical practice.
Methods of Evaluating Treatment Outcome
In theory, there are three methods (clinical, radiological and histological) available to evaluate the results of endodontic treatment (Fig 1-1).
Fig 1-1 Methods of evaluating treatment outcome.
Clinical Evaluation
The patient is questioned about any symptoms experienced, whether the tooth feels normal and is comfortable in function. A clinical examination is then carried out to look for signs of disease such as the presence of:
-
a swelling
-
a sinus tract (Fig 1-2a) or
-
tenderness.

Fig 1-2 Signs of failure. (a) Clinical – a buccal sinus tract. (b) Radiological – a periapical radiolucent area.
An absence of abnormal clinical signs and symptoms is considered indicative of success. There is an element of subjectivity, however, when assessing treatment outcome clinically. Although there is little question if overt signs or symptoms of disease are present, a patient’s lack of symptoms may not necessarily mean that the tooth is disease-free and will remain symptom-free. Chronic lesions may have varying presentations, with the patient being unaware of their presence perhaps until, with little warning, alterations in the host/microbial balance transform the dormant lesion into an acute phase; this is something we have all witnessed often.
Radiological Evaluation
Radiographs of the tooth are taken and processed using a standardised technique to ensure a good quality, undistorted image. The radiographs are viewed on a light-box, with magnification and ideally with extraneous light blocked off (Fig 1-3). The following are evaluated:
-
quality of the root filling: in particular, its length and density
-
periodontal health, including the width of the apical and lateral periodontal ligament space
-
presence, location, size and nature of the margin of any radiolucencies (Fig 1-2b) or radiopacities.

Fig 1-3 Radiographs are viewed on a light-box using a film magnifying cone.
In essence, the task is to detect any features that are not consistent with the radiographic characteristics of healthy periapical tissues. If available, previous radiographs should be used for comparison to ascertain any differences in radiographic appearance with time (Fig 1-4).
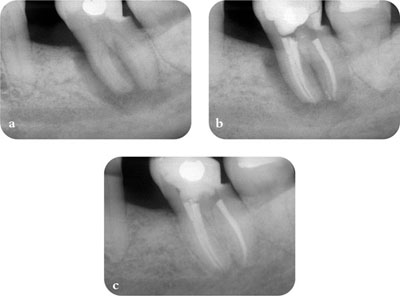
Fig 1-4 Previous radiographs should be used for comparison when assessing treatment outcome. (a) Pre-op radiograph. (b) Post-op radiograph. (c) Two-year review radiograph.
A major problem with the radiological assessment of treatment outcome is that:
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


