1 Anatomic Sciences
1.0 GROSS ANATOMY
1.1 Head and Neck
1.1.1 Oral Cavity
Vascular supply
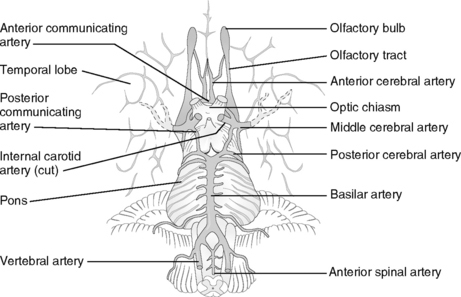
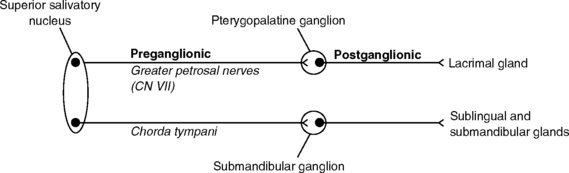
Figure 1-1 Inferior view of the brain: circle of Willis.
(From Moore NA, Roy WA: Gross and Developmental Anatomy, St. Louis, Mosby, 2002.)
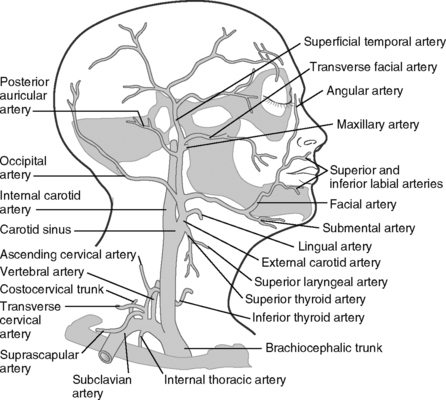
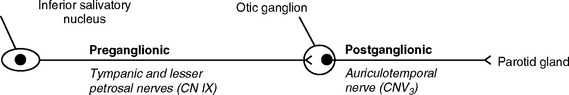
Figure 1-2 Lateral view of arteries of the neck and superficial head.
(Modified from Moore NA, Roy WA: Gross and Developmental Anatomy, St. Louis, Mosby, 2002.)
TABLE 1-1 MAJOR BRANCHES OF THE FACIAL ARTERY AND THE STRUCTURES THEY SUPPLY
| BRANCHES | STRUCTURES SUPPLIED |
|---|---|
| Ascending palatine artery | Soft palate, tonsils, pharynx |
| Tonsillar artery | Tonsils, tongue |
| Glandular artery | Submandibular gland |
| Submental artery | Submandibular gland, mylohyoid and anterior digastric muscle |
| Inferior labial artery | Lower lip |
| Superior labial artery | Upper lip |
| Lateral nasal artery | Nose |
| Angular artery | Eyelids, nose |
TABLE 1-2 BRANCHES OF THE THREE MAJOR DIVISIONS OF THE MAXILLARY ARTERY AND THE STRUCTURES THEY SUPPLY
| BRAN CHES OF THE THREE MAJOR DIVISIONS | STRUCTURES SUPPLIED |
|---|---|
| Mandibular division | |
| Inferior alveolar artery (IAA) branches | |
| Deep auricular artery | Tympanic membrane |
| Anterior tympanic artery | Tympanic membrane |
| IAA (dental branches) | Mandibular posterior teeth and surrounding tissues |
| Mylohyoid artery | Mylohyoid muscle, floor of mouth |
| Incisive artery | Anterior teeth and surrounding tissues |
| Mental artery | Chin, lower lip |
| Middle meningeal artery | Meninges of the brain, dura of bones in the skull |
| Pterygoid division | |
| Deep temporal arteries | Temporalis muscle |
| Pterygoid arteries | Pterygoid muscles |
| Masseteric artery | Masseter |
| Buccal artery | Buccinator, buccal mucosa |
| Pterygopalatine division | |
| Posterior superior alveolar artery | Maxillary posterior teeth, maxillary sinus |
| Infraorbital artery, including anterior and middle superior alveolar, orbital, and facial branches | Maxillary anterior teeth, orbital area and lacrimal gland |
| Greater palatine artery | Hard palate, lingual gingiva of maxillary posterior teeth |
| Lesser palatine artery | Soft palate, tonsils |
| Sphenopalatine artery | Nasal cavity |
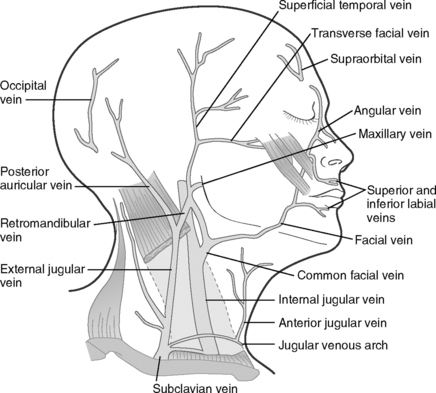
Venous drainage
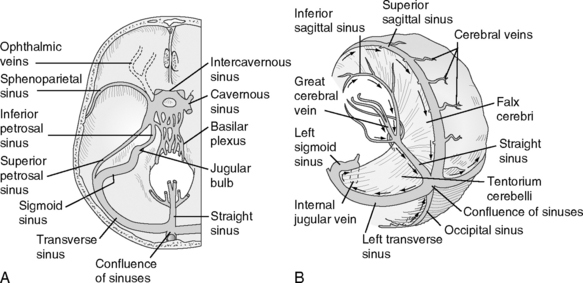
Figure 1-3 Dural venous sinuses. Arrows note the direction of blood flow.
(From Moore NA, Roy WA: Gross and Developmental Anatomy, St. Louis, Mosby, 2002.)
Lymphatic drainage
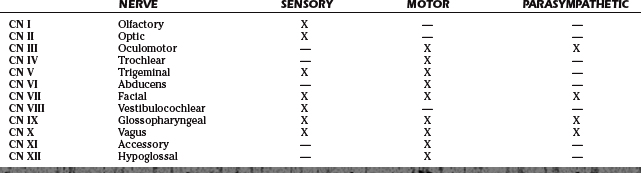
1.1.2 Cranial Nerves
Basic principles and definitions
TABLE 1-3 SUPERFICIAL LYMPH NODES
| PRIMARY NODE | TISSUES DRAINED | SECONDARY NODE |
|---|---|---|
| Submandibular nodes |
| LOCATION | STRUCTURES DRAINED | |
|---|---|---|
| Superior deep cervical lymph nodes | Inferior to the anterior border of the sternocleidomastoid muscles |
| AFFERENT | EFFERENT | |
|---|---|---|
| Corneal (blink) reflex | CN V1 | CN VII |
| Gag reflex | CN IX | CN X |
| Jaw jerk | CN V3 | CN V3 |
| Oculocardiac relex | CN V1 | CN X3 |
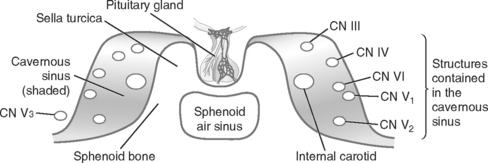
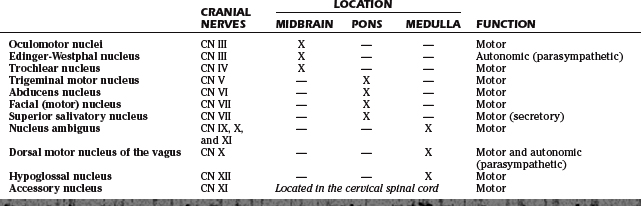
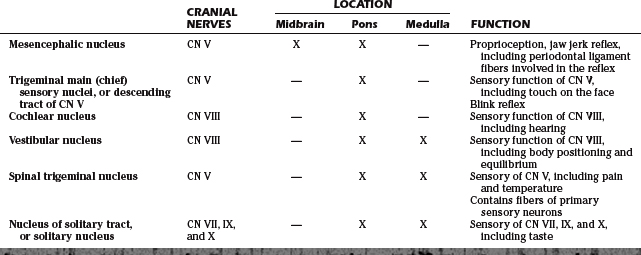
Cranial nerve nuclei
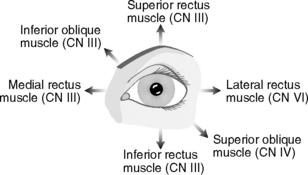
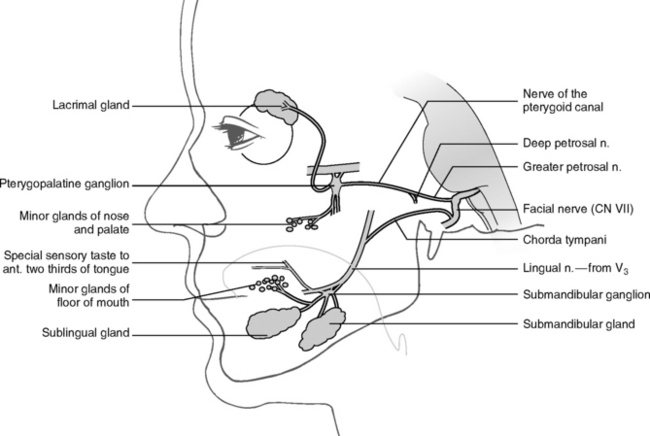
Cranial nerves
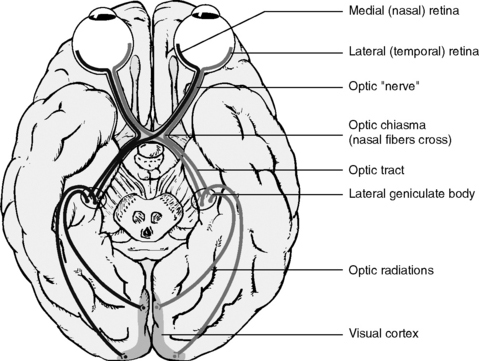
Figure 1-6 Optic pathway of CN II.
(Modified from Liebgott B: The Anatomic Basis of Dentistry, ed 2, St. Louis, Mosby, 2001.)
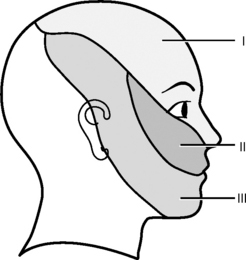
Figure 1-9 Sensory distribution for the three divisions of the trigeminal nerve.
(Modified from Fehrenbach M, Herring S: Illustrated Anatomy of the Head and Neck, ed 2, Philadelphia, WB Saunders, 2002.)
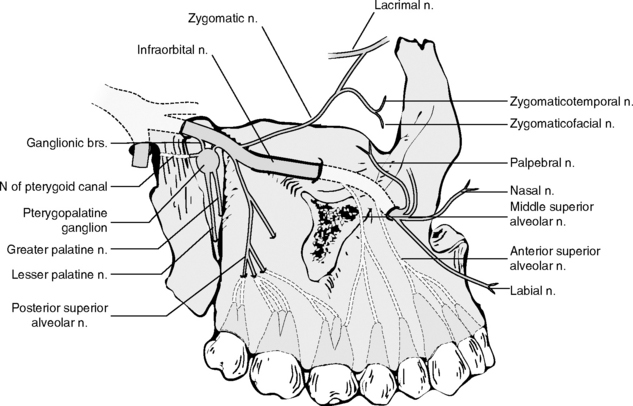
| V2 BRANCH | FUNCTION | DISTRIBUTION |
|---|---|---|
| Posterior superior alveolar nerve | Sensory | Maxillary second and third molars |
| Maxillary first molar: palatal and distobuccal root | ||
| Maxillary sinus | ||
| Middle superior alveolar nerve | Sensory | Maxillary first and second premolars |
| Maxillary first molar: mesiobuccal root | ||
| Anterior superior alveolar nerve | Sensory | Maxillary anterior teeth |
| Greater palatine nerve | Sensory | Posterior hard palate |
| Lingual gingiva of maxillary posterior teeth | ||
| Lesser palatine nerve | Sensory | Soft palate |
| Tonsils | ||
| Nasopalatine nerve | Sensory | Anterior hard palate |
| Lingual gingiva of maxillary anterior teeth |
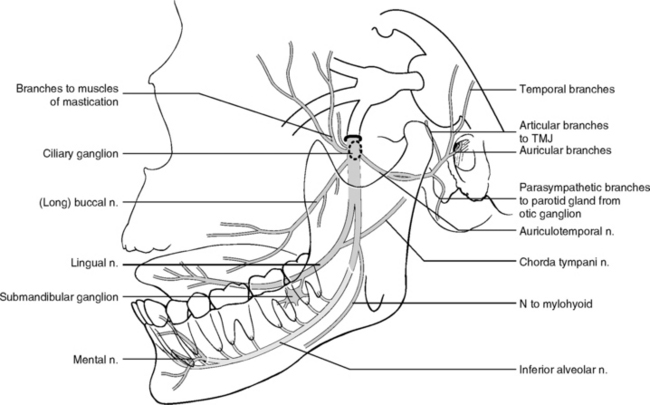
Figure 1-11 Branches of the mandibular division of the trigeminal nerve (CN V3).
(Modified from Liebgott B: The Anatomic Basis of Dentistry, ed 2, St. Louis, Mosby, 2001.)
TABLE 1-10 BRANCHES OF THE MANDIBULAR DIVISION OF THE TRIGEMINAL NERVE (CN V3)
| V3 BRANCH | FUNCTION | DISTRIBUTION |
|---|---|---|
| Long buccal nerve | Sensory | Cheek |
| Buccal gingiva of posterior mandibular teeth | ||
| Posterior buccal mucosa | ||
| Lingual nerve | Sensory | Lingual gingiva of mandibular teeth |
| Floor of mouth | ||
| Inferior alveolar nerve | Sensory | Mandibular posterior teeth |
| Mental nerve | Sensory | Chin |
| Lower lip | ||
| Anterior labial mucosa | ||
| Incisive nerve | Sensory | Mandibular anterior teeth |
| Auriculotemporal nerve | Sensory | TMJ |
| External auditory meatus | ||
| Auricle | ||
| Deep temporal nerves, anterior and posterior | Motor | Temporalis muscle |
| Masseteric nerve | Motor | Masseter muscle |
| Lateral pterygoid nerve | Motor | Lateral pterygoid muscle |
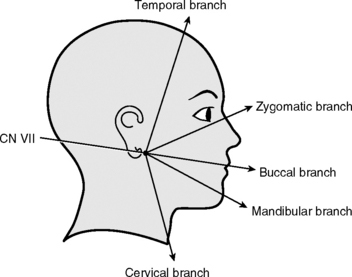
Figure 1-12 Facial nerve (CN VII): motor branches to the muscles of facial expression.
(Modified from Fehrenbach M, Herring S: Illustrated Anatomy of the Head and Neck, ed 2, Philadelphia, W. B. Saunders, 2002.)
Spaces and cavities of the head and neck
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses