Community oral-health programs focus primarily on populations, including those who do not seek oral health care. Planning these programs should include involvement of the community, broadly defined to include individuals and organizations that represent those who can help design and implement it and those who could be affected by it. This article provides an overview of systematic approaches to planning and evaluating community oral health programs. Such approaches help ensure that stakeholders agree on the purpose of the program, work toward its success, and contribute toward its continuous improvement.
Community oral health programs
Dentistry traditionally has focused primarily on providing care to individual patients on a one-on-one basis. Most United States residents seek dental care from dentists in private practice, who diagnose disease, develop a treatment plan, and provide care. This model of care works reasonably well for much of the public but has several key deficiencies:
- •
There are financial, geographic, cultural, attitudinal, and other barriers that restrict access to private practice- based dental care for a large segment of the public;
- •
Despite policy statements and recommendations from organizations such as the American Academy of Pediatric Dentistry , preventive dental visits remain very rare among young children. It remains uncertain whether there is adequate capacity in the United States to provide dental care for all children by 12 months of age ;
- •
Prevention services often can be delivered in a more cost-effective manner in venues other than private dental offices;
- •
Dental public health problems frequently require policy initiatives, community-based initiatives, and environmental changes that are outside the scope of the individual private practice dental office.
Population versus individual approach
There are several key differences between a personal dental care approach and a community oral health approach to controlling oral disease in a population. Personal dental care requires an individual to visit a dentist, who then initiates care by taking a dental and medical history and conducting an examination. The dentist arrives at a diagnosis and develops a treatment plan. After obtaining the patient’s informed consent, the dentist renders dental care, collects his or her fee, and schedules the patient for a follow-up visit.
Community oral health programs follow steps analogous to those taken by an individual dentist but focus primarily on a population, including persons who do not or cannot access care, rather than just one patient in the chair. The director of a community oral health program collects the necessary information to identify community problems, much like an individual dentist diagnoses a patient’s condition. The director then uses that information to develop policies and programs to address the problem, just as the individual dentist develops a treatment plan. Finally, the community oral health program delivers services to the community, as a dentist would provide treatment. Those services likely include more than provision of patient-based clinical care.
Population versus individual approach
There are several key differences between a personal dental care approach and a community oral health approach to controlling oral disease in a population. Personal dental care requires an individual to visit a dentist, who then initiates care by taking a dental and medical history and conducting an examination. The dentist arrives at a diagnosis and develops a treatment plan. After obtaining the patient’s informed consent, the dentist renders dental care, collects his or her fee, and schedules the patient for a follow-up visit.
Community oral health programs follow steps analogous to those taken by an individual dentist but focus primarily on a population, including persons who do not or cannot access care, rather than just one patient in the chair. The director of a community oral health program collects the necessary information to identify community problems, much like an individual dentist diagnoses a patient’s condition. The director then uses that information to develop policies and programs to address the problem, just as the individual dentist develops a treatment plan. Finally, the community oral health program delivers services to the community, as a dentist would provide treatment. Those services likely include more than provision of patient-based clinical care.
Reach versus intensity
Because dental public health is focused on the oral health of communities and populations and always operates within the constraints of financing and feasibility, the types of services provided involve a balance between what might work best for an individual and what might be possible to deliver to entire populations. Often, programs that reach a wider audience but are less intensive for any one person—and therefore perhaps less effective at an individual level—may produce better population health outcomes than far more intensive interventions delivered to a much smaller group.
For example, intensive smoking cessation treatments, such as group behavior therapy programs, are more effective than self-help alone , but because so few smokers are willing to participate in such intensive programs, they will have almost no measurable effect in reducing the prevalence of smoking in a population. In comparison, weaker and relatively inexpensive interventions, such as increasing the cost of cigarettes through taxation and changing the environmental norm through workplace smoking restrictions, can lead to large reductions in smoking and, consequently, fewer smoking-related deaths .
Similar effects are possible with dental caries prevention programs. For example, community water fluoridation may have lower effectiveness than twice-a-year applications of fluoride varnish by a dental hygienist for an individual at high risk for caries , but water fluoridation may likely prevent much more disease in a population because of its reach.
Balancing individual rights and societal protection
Public health practice, particularly in the United States, frequently involves a contentious balance between individual rights and societal benefit. Motorcycle helmet laws typify this tension: despite overwhelming epidemiologic evidence that motorcycle helmets reduce fatalities and serious injuries, many motorcycle riders perceive such laws as an infringement on personal liberties . Proponents of motorcycle helmet laws argue that a burden is placed on society when an individual suffers injury or death from preventable motorcycle fatalities . Similar arguments of individual rights versus social good have been made regarding dental public health policies including, for example, community water fluoridation and school-based dental screening .
Planning and evaluating community oral health programs
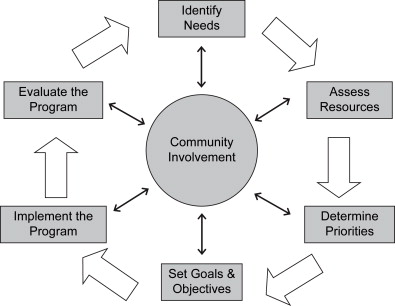
Planning may be defined as a systematic approach to defining a problem, setting priorities, developing specific goals and objectives, and determining alternative strategies and methods of implementation . Although typically described as a linear series of steps or as a cyclical process ( Fig. 1 ), program planning usually involves an ongoing, dynamic process with multiple interactions among the components. So, although the process is described as a series of steps, many of the activities involved in planning and evaluation can occur simultaneously or involve modifications along the way. For example, assessment of needs and resources can occur simultaneously, and the process of setting goals and objectives frequently involves reassessing the available resources to determine the feasibility of pursuing some program objectives.
Although there are many textbooks, book chapters, and journal articles on program planning, relatively few focus specifically on community oral health programs. The framework below draws on the expertise and experiences of state and local dental program directors, academicians, and organizations, as captured in “A Guide for Developing and Enhancing Community Oral Health Programs” .
Engage the community
A major key to successful community oral health program planning and implementation is involving community stakeholders in the process . Community organizations, leaders, and institutions should be engaged as coalition members and partners as early as possible in the planning process.
A coalition is a group of diverse individuals and organizations who work together to achieve a common goal. Participants usually represent key organizations or groups within the community. These individuals meet regularly to exchange ideas, reach a common goal, and create a group dedicated to improving the lives of community members around a particular issue.
Oral health coalitions provide several major advantages: (1) they help highlight the importance and magnitude of oral health needs in the community; (2) they leverage support from multiple organizations and individuals to increase the resources available to address oral health issues; (3) they involve community organizations in planning to help ensure that programs will be feasible and culturally acceptable to the community; (4) they help increase trust among groups; and (5) initiatives endorsed and supported by a broad range of groups are more likely than solo efforts to garner attention and support from elected officials and policymakers, who can help secure resources and policy changes to reach program objectives.
Although governmental dental public health authorities have a unique responsibility to promote and protect the oral health of the people, growing realization that government cannot do it alone has led to calls for increasing public-private collaborations . Public resources are always limited, and public health is just one of many societal priorities. The factors that impact public health come from a variety of sources and sectors, including employment, education, laws and policies, and social norms. Those sectors may need to be engaged in efforts to promote public health. There is a growing recognition that individuals, communities, and social institutions can form powerful collaborative relationships to improve health in ways that government alone cannot.
A partial list of potential coalition partners might include:
- •
Parent-teacher organizations
- •
Local chapters of professional groups, such as dental societies, dental hygiene associations, and primary care organizations
- •
Agencies that work with special needs populations, such individuals with disabilities
- •
Dental schools and dental hygiene programs
- •
Faith-based organizations
- •
Children’s health advocacy groups
- •
Service organizations for older adults
Identify oral health needs
Before launching an oral health program, it is essential to first assess the oral health status and needs of the community. Data needed to plan, monitor, and evaluate dental public health policies and programs come from a number of sources. Although national and state-level data may exist, it is almost always preferable to plan and evaluate using local or community-level data. There are a variety of sources for such data, which may be readily available or require original data collection.
Sociodemographic characteristics of the community
A wide range of information at the county or local level is available from the US Census Bureau. For example, the decennial census and periodic surveys, such as the American Community Survey , provide data on characteristics of the county or city such as age, race, ethnicity, housing units, educational attainment, household income, and poverty status. Data for a number of characteristics are available for geographic areas smaller than counties, such as census tracts, block groups, or blocks.
Water fluoridation status
Information on the community water fluoridation status of nearly all public water systems in the United States is available from the Centers for Disease Control and Prevention (CDC), Division of Oral Health, at http://apps.nccd.cdc.gov/MWF/Index.asp . The information is updated periodically based on monitoring data submitted to the Water Fluoridation Reporting System. Access to the original data can be requested from individual state oral health programs and tribes.
Cancer registries
State-based cancer registries are data systems that collect, manage, and analyze data about cancer cases and cancer deaths. In each state, health care facilities report these data to a central cancer registry. These cancer registries provide the ability to monitor trends in the number of new cases of oral cancer, oral cancer incidence rates (ie, number of new cases per 100,000 population), oral cancer survival rates, and cancer stage at the time of diagnosis. These statistics are available for the total population within each state, as well as by sex, age, and race, at http://apps.nccd.cdc.gov/uscs .
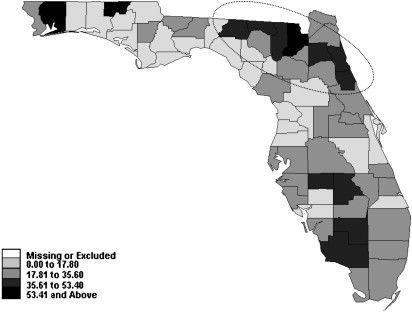
Cancer registries can usually provide oral cancer data for counties or cities, which is useful in targeting areas with unusually high rates of new cases or late-stage diagnosis. For example, analysis of cancer registry data in Florida helped to identify a multicounty area in the northeastern part of the state in which black males experienced a particularly high incidence rate ( Fig. 2 ), which led to the development of a local oral cancer awareness and screening program.
Clinical surveys
At least 15 state dental programs have conducted statewide clinical surveys within the past six years, although none included adults . Most states employed the Basic Screening Survey (BSS), which was developed by the Association of State and Territorial Dental Directors . The BSS was developed as a simple training and data collection tool that could be used by screeners with or without dental backgrounds. That approach was taken because nondental health professionals, such as public health nurses, sometimes have direct access to some population groups and because some states and communities have few public health dental professionals to assist in screening surveys. The BSS has components for collecting clinical oral health data for preschool-aged children, school children, and adults.
The primary barriers to collection of original clinical data are expense and logistic difficulties. Clinical surveys often require training personnel to conduct the examinations, traveling to multiple locations, obtaining portable or mobile dental equipment, adhering to infection control protocols, and gaining the cooperation and trust of school officials, parents, and children. Clinical surveys of adults are particularly difficult and expensive, which explains in part why there are almost no clinical data on adult oral health at the state or local levels.
Nonclinical oral health surveys
A good deal of information relevant to planning and evaluating oral health issues can be obtained from nonclinical surveys. These surveys involve collection of data via telephone, face-to-face interviews, or self-completed questionnaires but do not require clinical examination of participants. These types of surveys are often the most economically and logistically feasible ways to reach adults. Valid data on many relevant oral health topics can be covered through self-reported surveys.
One relatively cost-effective approach for gathering oral health-related data at the state, county, or local level is to partner with other organizations or agencies that will be conducting surveys and add relevant oral health questions. For example, the Behavioral Risk Factor Surveillance System (BRFSS) is a state-based, ongoing telephone survey on preventive health practices and risk behaviors that are linked to chronic diseases, injuries, and preventable infectious diseases . The BRFSS is administered in all states and the District of Columbia. All states include a core set of questions developed in conjunction with the CDC, several optional modules on a wide range of health topics, and a number of state-added questions. The BRFSS core questionnaire includes several oral health variables, including tooth loss, last dental visit, preventive care, and risk factors relevant to oral health. States frequently make their state-added questions available to groups working on health-related topics. States usually charge a fee per question added, but the cost is far less than that of a typical stand-alone telephone survey. A number of states periodically conduct county BRFSS surveys, in which the sample design allows estimates at the county level. Information on the BRFSS surveys is available at http://www.cdc.gov/brfss .
Health care providers, facilities, and programs
Information on the number and locations of area dentists, dental hygienists, and other licensed health care providers can usually be obtained from the state licensing authority. County and local dental societies also may be able to provide information on the number and location of dental specialists. The state government agency that oversees labor and employment frequently has data on the number and location of dental offices, clinics, and other health care facilities. Information on the number of providers participating in Medicaid or the State Children’s Health Insurance Program (SCHIP) is available at the state agency that oversees those programs. The Health Resources and Services Administration, Bureau of Health Professions (HRSA-BHP) has information on the criteria and application process for designation as a dental health professional shortage area (HPSA). HRSA-BHP offers a searchable database of HPSAs with information available at the state, county, and census tract levels.
Putting it together
Even the best data are meaningless unless they can be analyzed and interpreted. When planning to assemble existing information or collect original data, it is critical to identify the individuals or organizations that will help with those tasks. Expertise may reside in the local or state health department, the nearby dental school or school of public health, or consultants. Coalition members may be able to offer such services as part of their contribution to the program or identify expertise elsewhere.
Assess resources
As mentioned earlier, one major benefit of forming a community oral health coalition is to leverage resources. Although any one organization may lack the resources to address major oral health problems by itself, a collaborative effort may pool the limited resources from multiple parties to be able to achieve a common goal.
Resources may include expertise, funding, personnel, equipment, or access to other influential individuals and organizations. It is not possible to list all potential resources, but some sources to consider include:
Dental schools, dental hygiene programs, and dental assisting programs
These institutions may be able to provide expertise and assistance in collection of oral health data, delivery of prevention or treatment services, and access to portable or mobile dental equipment. In addition, faculty may be able to serve as expert speakers on oral health topics. Most universities have communications offices, which may be able to help promote the program if their faculty members are involved in the project.
Schools of public health
Schools of public health can provide assistance with design and conduct of surveys and data analysis. In addition, many schools of public health have established community links and may be able to facilitate connections with community leaders and organizations. Students in schools of public health frequently need to complete internships or research projects, and their participation in community oral health programs can be mutually beneficial.
Federally qualified community health centers
Federally qualified community health centers, or FQHCs, are nonprofit, consumer-directed corporations that serve as “safety net” providers, such as community health centers, public housing centers, outpatient health programs funded by the Indian Health Service, and programs serving migrants and the homeless . The main purpose of FQHCs is to enhance the provision of primary care services in underserved urban and rural communities. Most FQHCs provide dental services . These health centers may be able to assist with expertise, program implementation, and access to community boards of directors.
Area health education centers
The Area Health Education Centers (AHEC) program was developed by Congress in 1971 to recruit, train, and retain a health professionals workforce committed to underserved populations . The Health Education Training Centers (HETC) program was created in 1989 to provide programs for specific populations with persistent, severe, and unmet health needs. The AHEC and HETC programs are intended to leverage the resources of academic health centers to help address local community health needs. These programs can contribute substantial expertise and support in bringing dental students, residents, and faculty into underserved communities; developing and implementing service learning; and providing community education and wellness programs.
School nurses
Schools have long been major venues for reaching children to monitor oral health status and to deliver prevention and treatment services. Although not all schools have a nurse, school nurses play a vital role in ensuring the health of students, identifying health needs, and advocating for necessary resources. They can be a valuable resource in understanding the impact of oral health problems on learning, gathering data on the health status of the student population, and supporting delivery of oral health services in schools.
State and local dentistry and dental hygiene societies
Organized dentistry and dental hygiene societies can be critical resources in establishing dental public health programs. They bring a great deal of expertise to the process, and commitment from these organizations may be critical to long-term success.
Determine priorities and establish objectives
Setting priorities
Determining health priorities helps direct resources to the areas that matter most to community partners and that will have the greatest impact on oral health status. Few public health programs have the resources to address all oral health needs of the community. Therefore, after identifying the community’s oral health needs and assessing the available resources, it is necessary to establish priorities. The community should be involved in establishing those priorities, and the problem of greatest interest to the health professionals in the coalition may not necessarily be the priority of the community members. Some of the factors to consider in prioritizing needs may include:
The magnitude and seriousness of the problem
Problems that affect a large number of people may take priority over problems that affect a small number. However, the relative prevalence of various conditions must be balanced against the severity and impact of those conditions. A widespread condition with minimal impact on health or quality of life may have a lower priority than a less common condition that carries a risk of fatality if not prevented or controlled or significantly impacts on quality of life for those affected. For example, gingivitis may have a very high prevalence, but might be considered a much lower priority than addressing late-stage diagnosis of oral and pharyngeal cancer.
The potential for interventions to impact the public’s oral health
Ideally, there should be an evidence base indicating that there is an effective intervention for the problem. Spending resources on unproven preventive strategies or treatments may be wasteful.
The feasibility of intervening
In addition, possible interventions must be acceptable to the community, able to be delivered using available resources, and in compliance with state and local laws and regulations.
Developing program goals and objectives
Program goals are broad statements on the overall purpose of a program. Goals generally express the aspirations of the planners of the state of affairs that will exist in the future because of their efforts. Example of program goals might be “to eliminate racial disparities in oral cancer survival rates,” “to improve the oral health of nursing home residents,” or “to improve the oral health of the county’s toddlers and school children.”
Program objectives are more specific statements of the desired endpoints of the project. They are the means through which the project’s broader goals are attained. As with other elements of the planning process, the objectives must represent the input and agreement of all members of the oral health coalition. Objectives for designing and evaluating community oral health programs should meet basic SMART criteria :
-
Specific – they should describe an observable action, behavior, or achievement;
-
Measurable – there are systems, methods, or procedures to track or record the action upon which the objective is focused;
-
Achievable – the objective is realistic, based on current environment and resources;
-
Relevant – the objective is important to the program and is under the control of the program;
-
Time-based – there are clearly defined deadlines for achieving the objective.
The most recent and notable set of oral health objectives for the nation is included in the voluminous collection known as “Healthy People 2010 Objectives” , the third set of decennial United States health objectives. The chapter on oral health provides specific, measurable objectives to be achieved by the year 2010 to attain its stated goal: “Prevent and control oral and craniofacial diseases, conditions, and injuries and improve access to related services.” Each oral health objective has a specified target population, a quantifiable measure to be attained, and a deadline. For example, the first objective is: “Reduce the proportion of young children with dental caries experience in their primary teeth. Target: 11 percent. Baseline: 18 percent of children aged 2 to 4 years had dental caries experience in 1988–94.” Similarly, many states have established their own oral health objectives.
Once priorities have been established by the community oral health coalition and program goals and objectives have been agreed upon, the next step is to design and implement the program.
Implement the program
As with all previous steps, implementing a community oral health program requires the collaboration of individuals, organizations, and the community. Implementation involves identifying a series of specific activities that must occur to achieve the agreed-upon goals and objectives. Perhaps the most effective approach is to start with each objective and identify the activities that will be required to reach that objective. For example, one program objective might be: “By 2010, at least 50% of African-American men aged 35 years or older in Duval County, Florida, will report having been examined for oral cancer within the preceding 12 months.” Achieving that objective would likely require several program components, as shown in the example in Table 1 .



