Temporomandibular disorders (TMD) refer to a large group of musculoskeletal disorders that originate from the masticatory structures . There are two broad types of TMD: those primarily involving the muscles and those primarily involving the temporomandibular joints. Muscle disorders are far more common than intracapsular disorders. This article focuses on the intracapsular disorders and is limited to the most common types encountered in the dental practice. The article begins with a brief review of normal temporomandibular joint (TMJ) anatomy and function followed by a description of the common types of disorders known as “internal derangements.” Nonsurgical management is suggested based on the long-term scientific documentation. This article represents a brief review of these conditions. Other references are suggested for more in depth information .
Normal function of the temporomandibular joint
For clinicians to effectively manage dysfunction of the temporomandibular joint, they must have a sound understanding of normal joint function because the treatment goal for a patient with dysfunction is to re-establish normal function. A clinician cannot manage a disorder without a sound understanding of order.
The temporomandibular joint represents the articulation of the mandible to the temporal bone of the cranium ( Fig. 1 ). The bony components of the joint are separated by a structure composed of dense fibrous connective tissue called the articular disc. Like any mobile joint, the integrity and limitations of the joint are maintained by ligaments. Ligaments are composed of collagenous fibers that have specific lengths. Ligaments do not actively participate in normal function of the joint; rather, they act as guide wires to restrict certain movements (border movements) while allowing other movements (functional movements). If joint movements consistently function against ligaments, the length of the ligaments can become altered. Ligaments have a poor ability to stretch, and therefore, when this occurs, they often elongate. This elongation creates a change in joint biomechanics and can lead to certain clinical changes discussed in this article.
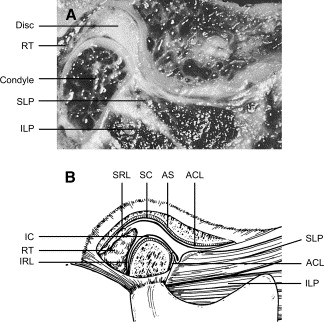
Careful examination of the condyle and disc reveals that the disc is attached to the condyle medially and laterally by the discal collateral ligaments ( Fig. 2 ). These ligaments allow rotation of the disc across the articular surface of the condyle in an anterior and posterior direction while restricting medial and lateral movements. The range of anterior and posterior rotation of the disc is also restricted by ligaments. The inferior retrodiscal lamina limits anterior rotation of the disc on the condyle, whereas the anterior capsular ligament limits posterior rotation of the disc ( Fig. 1 ).
The morphology of the disc is extremely important. It is thinnest in the intermediate zone, thicker in the anterior border, and thickest in the posterior border. The condyle articulates on the intermediate zone of the disc and is maintained in this position by constant interarticular pressure provided by the elevator muscles (masseter, temporalis, and medial pterygoid). Although the pressure between the condyle, disc, and fossa can vary according to the activity of the elevator muscles, some pressure is maintained to prevent separation of the articular surfaces. If contact between the articular surfaces is lost, a condition of dislocation exists (dislocation means separation of the articular surfaces).
Posterior to the disc are the retrodiscal tissues. These tissues are highly vascularized and well innervated. Anterior to the condyle-disc complex are the superior and inferior lateral pterygoid muscles. The inferior pterygoid muscle inserts on the neck of the condyle, whereas the superior lateral pterygoid muscle inserts on the neck of the condyle and the articular disc ( Fig. 1 ). The inferior lateral pterygoid is active with the depressing muscles (mouth opening), and the superior lateral pterygoid muscle has been shown to be active in conjunction with the elevator muscles (mouth closing) . The superior lateral pterygoid muscle seems to be a stabilizing muscle for the condyle–disc complex, especially during unilateral chewing.
When the condyle–disc complex translates down the articular eminence (ie, the mouth opening), the disc rotates posteriorly on the condyle ( Fig. 3 ). The superior surface of the retrodiscal tissues is unlike any other structure in the joint. The superior retrodiscal lamina is composed of loose connective tissue and elastin fibers that allow the condyle–disc complex to translate forward without damage to the retrodiscal tissues. In the closed mouth position, the superior retrodiscal tissues are passive and have little influence on disc position. During full mouth opening, the superior retrodiscal lamina is fully stretched and produces a posterior, retractive force on the disc ( Fig. 3 ). This is the only structure in the temporomandibular joint capable of providing a retractive force on the articular disc.
During opening and closing, the disc and condyle move together, not because of ligamentous attachments, but because of two fundamental features: the morphology of the disc and interarticular pressure (pressure between the articular surfaces). Because some degree of interarticular pressure is always present, the condyle maintains itself on the thinnest intermediate zone of the disc. The thicker anterior and posterior borders of the disc force it to translate with the condyle during mouth opening and closing. It is the disc’s morphology, therefore, that requires it to move with the condyle. If there is an alteration in interarticular pressure or a change in the morphology of the disc, condyle–disc movement can be altered. This begins the biomechanical changes associated with internal derangements.
Intracapsular disorders of the temporomandibular joint
Once change occurs in the structure of the condyle–disc complex, normal biomechanics can be altered. This alteration results in specific clinical signs and symptoms. It is by these signs and symptoms that a classification of disorders can be developed. Intracapsular disorders fall into one of two broad types: derangements of the condyle–disc complex and structural incompatibility of the articular surfaces . Because of the brevity of this article, only derangements of the condyle–disc complex are discussed. These conditions include disc displacements with reduction and disc dislocations without reduction. In this section each category is described according to etiology, anamnestic, or history findings and clinical characteristics.
Disc displacement with reduction
Derangements of the condyle–disc complex arise from breakdown of the normal rotational movement of the disc on the condyle. This loss of normal disc movement can occur when there is elongation of the discal collateral ligaments and the inferior retrodiscal lamina. If the inferior retrodiscal lamina and the discal collateral ligament are elongated, the disc can be positioned more anteriorly by pull of the superior lateral pterygoid muscle. If this anterior pull is constant, a thinning of the posterior border of the disc may allow the disc to be displaced in a more anterior position ( Fig. 4 , position 1). With the condyle resting on a more posterior portion of the disc or retrodiscal tissues, an abnormal translatory shift of the condyle over the posterior border of the disc can occur during opening. Associated with the abnormal condyle–disc movement is a click that may be initially felt just during opening (single click) ( Fig. 4 , position 3) but later may be felt during opening and closing of the mouth (reciprocal clicking) ( Fig. 4 , position 8).

Etiology
The most common etiologic factor associated with breakdown of the condyle–disc complex is trauma. This may result from macrotrauma or microtrauma. Macrotrauma represents a single, often sudden, episode of trauma, such as a blow to the jaw . Open mouth macrotrauma commonly produces elongation of the ligaments, whereas closed mouth trauma is more often associated with impact loading of the articular surfaces. Microtrauma is a produced by mild, frequent forces over a long period. Chronic muscle hyperactivity, such as bruxism, is an example of microtrauma. Although not well documented, chronic muscle hyperactivity may contribute to internal derangement disorders when significant orthopedic instability is present .
History
It is common for a history of trauma to be associated with the onset of joint sounds. There may or may not be pain accompanying the disc displacement with reduction. If pain is present, it is intracapsular and associated with the dysfunction (the click).
Clinical characteristics
Examination reveals joint sounds during mouth opening and often during mouth closure. Disc displacement is characterized by a normal range of jaw movement during opening and eccentric movements. Any limitation is due to pain and not to a true structural dysfunction. When reciprocal clicking is present, the two clicks normally occur at different degrees of mouth opening, with the closing click usually occurring near the intercuspal position. Pain, if present, is directly related to joint function.
If the inferior retrodiscal lamina and discal collateral ligaments become further elongated and the posterior border of the disc sufficiently thinned, the disc can slip or be forced completely through the discal space. Because the disc and condyle no longer articulate, this condition is referred to as a “disc dislocation” ( Fig. 4 ). If the patient can manipulate the jaw to reposition the condyle over the posterior border of the disc, the disc is said to be reduced. This represents a progression of the disc movement and may be accompanied by the patient report of joint catches and getting stuck. The patients may describe having to move the jaw around a little to get it back to functioning normally. The catching may or may not be painful, but if pain is present it is directly associated with the dysfunctional symptoms.
Disc dislocation without reduction
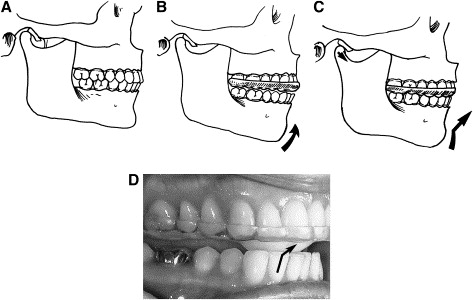
As the elasticity of the superior retrodiscal lamina is lost or the disc undergoes morphologic change, recapturing of the disc becomes more difficult. When the disc is not reduced, the forward translation of the condyle forces the disc further anteriorly ( Fig. 5 ). This is clinically called a “closed lock” because the disc dislocation does not allow full mouth opening.
History
Most patients who have a history of disc dislocation without reduction know precisely when the dislocation occurred. They can readily relate it to an event such as biting into an apple or waking up with the condition. They report that the jaw is locked closed so that normal mouth opening cannot be achieved. Pain is commonly associated with dislocation without reduction. When pain is present, it usually accompanies trying to open beyond the point of joint restriction. The history also reveals that clicking occurred before the onset of locking but not since the disc dislocation has occurred.
Clinical characteristics
The range of mouth opening is commonly between 25 and 30 mm, and the mandible often deflects toward the involved joint during maximum opening. At the maximum point of opening, there is a hard end feel. In other words, if mild, steady, downward forward pressure is applied to the lower incisors, there is no increase in mouth opening. Eccentric movement is relatively normal to the ipsilateral side but restricted to the contralateral side. Loading the joint with bilateral manual manipulation is often painful because the condyle is seated on the retrodiscal tissues.
Nonsurgical management of intracapsular disorders
The correct management of TMJ intracapsular disorders is predicated on two factors: making a correct diagnosis and understanding the natural course of the disorder. Each of the categories of internal derangements represents a clinical condition that is treated in a particular manner. An incorrect diagnosis leads to mismanagement and treatment failure.
Successful management of intracapsular disorders is also based on the clinician’s understanding of the natural course of the disorder. Although the sequence of internal derangements is often clinically evident, it does not account for the outcome of all intracapsular disorders. The presence of chronic, unchanging, asymptomatic joint sounds suggests that intracapsular disorders are not always progressive. Epidemiologic studies reveal that asymptomatic joint sounds are common . This poses an interesting question: If all joint sounds are not progressive, which sounds should be treated? It is my opinion that only joint sounds associated with pain should be considered for treatment provided that the pain is intracapsular in origin. In other words, patients who present with extracapsular muscle pain and a painless clicking joint should not be managed for the intracapsular disorder. Doing so leads to treatment failure because it does not address the source of the pain. Most painless joint sounds do not seem to lead to any major progressive disorders .
The management of disc displacement with reduction and disc dislocation without reduction is discussed separately because data suggest they should be managed differently.
Disc displacement with reduction
Definitive treatment for disc displacement with reduction (and disc dislocation with reduction) is to re-establish a normal condyle–disc relationship. Although this may sound relatively easy, it has not proven to be so. During the past 30 years, the dental profession’s attitude toward management of intracapsular disc derangements has changed greatly. In the early 1970s, Farrar introduced the anterior positioning appliance. This appliance provides an occlusal relationship that requires the mandible to be maintained in a forward position ( Fig. 6 ). The position selected is one that places the mandible in the least protruded position that re-establishes a more normal condyle–disc relationship. This is usually achieved clinically by monitoring the clicking joint. Although eliminating the click does not always denote successful reduction of the disc , it is a good clinical reference point for beginning therapy.
The idea behind the anterior positioning appliance was to position the condyle back on the disc (ie, to “recapture the disc”). It was originally suggested that this appliance be worn 24 h/d for as long as 3 to 6 months. Although this appliance is helpful in managing certain disc derangement disorders, its use has changed considerably due to results of recent studies.
It was quickly discovered that the anterior positioning appliance was useful in reducing painful joint symptoms . When this appliance successfully reduced symptoms, a major treatment question was asked: What’s next? Some clinicians believed that the mandible needed to be permanently maintained in this forward position . Dental procedures were suggested to create an occlusal condition that maintained the mandible in this therapeutic relationship. Accomplishing this task was never a simple dental procedure . Others felt that once the discal ligaments repaired, the mandible should be returned to its normal position in the fossa (the musculoskeletally stable position), and the disc would remain in proper position (recaptured). Although one approach is more conservative than the other, neither is supported by long-term data.
In early short-term studies , the anterior positioning appliance proved to be much more effective in reducing intracapsular symptoms than the more traditional stabilization appliance. This led to the belief that returning the disc to its proper relationship with the condyle was an essential part of treatment. The greatest insight regarding the appropriateness of a treatment modality is gained from long-term studies. Forty patients with various derangements of the condyle–disc complex were evaluated 2.5 years after anterior positioning therapy and a step-back procedure . None received occlusal alterations. It was reported that 66% of the patients still had joint sounds, but only 25% were still experiencing pain problems. If the criteria for success in this study were the elimination of pain and joint sounds, then success was achieved in only 28%. Other long-term studies have reported similar findings. If the presence of asymptomatic joint sounds is not a criterion for failure, then the success rate for anterior positioning appliances rises to 75%. The issue that must be addressed, therefore, is the clinical significance of asymptomatic joint sounds.
Joint sounds are common in the general population. In many cases , it seems that they are not related to pain or decreased joint mobility. If all clicking joints progressed to more serious disorders, then this would be a good indication to treat every joint that clicked. The presence of unchanging joint sounds over time indicates that the structures involved can adapt to less than optimum functional relationships.
Long-term studies reveal that anterior positioning appliances are not as effective as once thought. They seem to be helpful in reducing pain in 75% of the patients, but joint sounds seem to be much more resistant to therapy, and their persistence does not always indicate a progressive disorder. These studies provide insight into how the joint responds to anterior positioning therapy. In many patients, advancing the mandible forward temporarily prevents the condyle from articulating with the highly vascularized, well innervated, retrodiscal tissues. This is the likely explanation for an almost immediate reduction of intracapsular pain. During the forward positioning, the retrodiscal tissues undergo adaptive and reparative changes . These changes result in dense fibrosis connective tissues that can be loaded by the condyle in the absence of pain.
Discs generally are not recaptured by anterior positioning appliances . Instead, as the condyle returns to the fossa, it moves posteriorly to articulate on the adapted retrodiscal tissues. If these tissues have adequately adapted, loading occurs without pain. The condyle functions on the newly adapted retrodiscal tissues, although the disc is still anteriorly displaced. The result is a painless joint that may continue to click with condylar movement ( Fig. 7 ). At one time the dental profession believed that the presence of joint sounds indicated treatment failure. Long-term follow-up studies have given the profession new insight regarding success and failure. We, like our orthopedic colleagues, have learned to accept that some dysfunction is likely to persist once joint structures have been altered. Controlling pain while allowing joint structures to adapt seems to be the most important role of the therapist.
A few long-term studies support the concept that permanent alteration of the occlusal condition can be successful in controlling most major symptoms. This treatment requires extensive dental therapy, and one must question the need when natural adaptation seems to work well for most patients. Reconstruction of the dentition or orthodontic therapy should be reserved for patients who present with a significant orthopedic instability.
The continuous use of anterior positioning appliance therapy is not without consequence. A certain percentage of patients who wear these appliances may develop a posterior open-bite. A posterior open-bite is likely the result of a reversible, myostatic contracture of the inferior lateral pterygoid muscle. When this condition occurs, a gradual relengthening of the muscle can be accomplished by converting the anterior positioning appliance to a stabilization appliance, which allows the condyles to assume the musculoskeletally stable position. This can also be accomplished by slowly decreasing use of the appliance.
The degree of myostatic contracture that develops is likely to be proportional to the length of time the appliance has been worn. When these appliances were first introduced, it was suggested that they be worn 24 h/d for 3 to 6 months. With 24-hour use, the development of a posterior open bite was common. The present philosophy is to reduce the time the appliance is being worn to limit the adverse effects on the occlusal condition. For most patients, full-time use is not necessary to reduce symptoms. The patient should be encouraged to wear the appliance only at night to protect the retrodiscal tissues from heavy loading (bruxism). During the day, the patient should not wear the appliance so that the mandible can return to its normal position. In most instances, this allows a mild loading of the retrodiscal tissue during the day, which enhances the fibrotic response of the retrodiscal tissues. If the symptoms can be adequately controlled without daytime use, myostatic contracture is avoided. This technique is appropriate for most patients, but if significant orthopedic instability exists, symptoms may not be controlled.
If the symptoms persist with only night-time use, the patient may need to wear the appliance more often. Daytime use may be necessary for a few weeks. As soon as the patient becomes symptom free, the use of the appliance should be gradually reduced. If reduction of use creates a return of symptoms, then the time allowed for tissue repair has not been adequate or orthopedic instability is present. It is best to assume that inadequate time for tissue repair is the reason for the return of symptoms. The anterior positioning appliance should therefore be reinstituted and more time given for tissue adaptation.
When repeated attempts to eliminate the appliance fail to control symptoms, orthopedic instability should be suspected. When this occurs, the anterior positioning appliance should be converted to a stabilization appliance that allows the condyle to return to the musculoskeletally stable position. Once the condyles are in the musculoskeletally stable position the occlusal condition should be assessed for orthopedic stability. If obvious orthopedic instability exists, dental procedures may need to be considered. In this author’s experience, the need for dental procedures is rare.
Supportive therapies
In addition to appliance therapy, the patient should be educated about the mechanics of the disorder and the adaptive process that is essential for treatment. When pain is present, the patient needs to be encouraged to decrease loading of the joint when ever possible. Softer foods, slower chewing, and smaller bites should be promoted. The patient should be told not to allow the joint to click whenever possible. If inflammation is suspected, a nonsteroidal anti-inflammatory drug, such as ibuprofen (600–800 mg, three times a day), may be prescribed. Moist heat or ice can be used if the patient finds either helpful. Active exercises are not usually helpful because they cause joint movements that often increase pain. Passive jaw movements may be helpful, and distractive manipulation by a physical therapist may assist in healing. These general principles are appropriate for most intracapsular disorders.
Disc dislocation without reduction
In the case of disc displacement with reduction, the anterior positioning appliance re-establishes the normal condyle–disc relationship. Fabricating an anterior positioning appliance for a patient who has a disc dislocation without reduction aggravates the condition by forcing the disc further forward. Patients who present with disc dislocation without reduction ( Fig. 5 ) need to be managed differently.
When the condition of disc dislocation without reduction is acute, the initial therapy should include an attempt to reduce or recapture the disc by manual manipulation. This manipulation is most successful with patients who are experiencing their first episode of locking. In these patients, there is a great likelihood that tissues are healthy and with minimal morphologic changes. Patients who have a long history of locking are likely to present with discs and ligaments that have undergone changes that will not allow reduction of the disc. As a general rule, when patients report a history of being locked for a week or less, manipulation is often successful. In patients who have a longer history, success begins to decrease rapidly.
The success of manual manipulation for the reduction of a dislocated disc depends on three factors. The first factor is the level of activity in the superior lateral pterygoid muscle. This muscle must be relaxed to permit successful reduction. If it remains active because of pain, it may need to be injected with local anesthetic before any attempt to reduce the disc. Second, the disc space must be increased so the disc can be repositioned on the condyle. When increased activity of the elevator muscles is present, the interarticular pressure is increased, making it more difficult to reduce the disc. The patient needs to be encouraged to relax and avoid forcefully closing the mouth. Third, the condyle must be in the maximum forward translatory position. The only structure that can produce a posterior or retractive force on the disc is the superior retrodiscal lamina, and if this tissue is to be effective, the condyle must be in the most forward protrusive position.
The first attempt to reduce the disc should begin by having the patient attempt to self-reduce the dislocation. With the teeth slightly separated, the patient is asked to move the mandible to the contralateral side of the dislocation as far as possible. From this position the mouth is opened maximally. If this is not successful at first, the patient should attempt this several times. If the patient is unable to reduce the disc, assistance with manual manipulation is indicated. The thumb is placed intraorally over the mandibular second molar on the affected side. The fingers are placed on the inferior border of the mandible anterior to the thumb position. Firm but controlled downward force is exerted on the molar at the same time that upward force is placed by the fingers on the outer inferior boarder of the mandible in the anterior region. The opposite hand helps stabilize the cranium above the joint that is being distracted. While the joint is being distracted, the patient is asked to assist by slowly protruding the mandible, which translates the condyle downward and forward out of the fossa. It may be helpful to bring the mandible to the contralateral side during the distraction procedure because the disc is likely to be dislocated anteriorly and medially, and a contralateral movement moves the condyle into it better.
Once the full range of laterotrusive excursion has been reached, the patient is asked to relax for 20 to 30 seconds while constant distractive force is applied to the joint. The clinician needs to be sure that unusual heavy forces are not placed on the uninvolved joint. Always ask the patient if he or she is feeling any discomfort in the uninvolved joint. If there is discomfort, the procedure should be immediately stopped and begun again with the proper directional force placed. A correctly performed manual manipulation to distract a TMJ should not jeopardize the healthy joint.
Once the distractive force has been applied for 20 to 30 seconds, the force is discontinued, and the fingers are removed from the mouth. The patient is asked to lightly close the mouth to the incisal end-to-end position on the anterior teeth. The patient is asked to relax for a few seconds and then to open wide and immediately return to this anterior position (not maximum intercuspation). If the disc has been successfully reduced, the patient should be able to open to the full range (no restrictions). When this occurs, the disc has likely been recaptured, and an anterior positioning appliance is immediately placed to prevent clenching on the posterior teeth, which would likely redislocate the disc. At this point, the patient has a normal condyle–disc relationship and should be managed in the same manner as discussed for the patient who has a disc dislocation with reduction, with one exception.
When an acute disc dislocation has been reduced, it is advisable to have the patient wear the anterior positioning appliance continuously for the first 2 to 4 days before beginning only night-time use. The rationale for this is that the dislocated disc may have become distorted during the dislocation, which may allow it to redislocated more easily. Maintaining the anterior positioning appliance in place for a few days may help the disc reassume its more normal shape (thinnest in the intermediate band and thicker anterior and posterior). If the normal morphology is present, the disc is more likely to be maintained its normal position. If this disc has permanently lost its normal morphology, it is difficult to maintain its position. This is why manual manipulations for disc dislocations are attempted only in acute conditions when the likelihood of normal disc morphology exists.
If the disc is not successfully reduced, a second and possibly a third attempt can be attempted. Failure to reduce the disc may indicate a dysfunctional superior retrodiscal lamina or a general loss of disc morphology. Once these tissues have changed, the disc dislocation is most often permanent.
If the disc is permanently dislocated, what types of treatments are indicated? This question has been asked for many years. At one time it was felt that the disc needed to be in its proper position for health to exist. Therefore, when the disc could not be restored to proper position, a surgical repair of the joint seemed to be necessary. Over years of studying this condition, we have learned that surgery may not be needed for most patients. Studies have revealed that over time many patients achieve relatively normal joint function even with the disc permanently dislocated. With these studies in mind, it would seem appropriate to follow a more conservative approach that would encourage adaptation of the retrodiscal tissues. Patients who have permanent disc dislocation should be given a stabilization appliance that reduces forces to the retrodiscal tissues (ie, decrease bruxism) .
Supportive therapy
Supportive therapy for a permanent disc dislocation should begin with educating the patient about the condition. Because of the restricted range of mouth opening, many patients try to force their mouth to open wider. If this is attempted too strongly, it aggravates the intracapsular tissues, producing more pain. Patients should be encouraged not to open too wide especially immediately after the dislocation. With time and tissue adaptation, they will be able to return to a more normal range of movement (usually > 40 mm) . Gentle, controlled jaw exercise may be helpful in regaining mouth opening , but care should be taken to not be too aggressive, which may lead to more tissue injury. The patient must be told that this may take a year or more for full range to be attained.
The patient should be told to decrease hard biting, to avoid chewing gum, and to avoid anything that aggravates the condition. If pain is present, heat or ice may be used. Nonsteroidal anti-inflammatory drugs are indicated for pain and inflammation. Joint distraction and phonophoresis over the joint area may be helpful.
When a joint is not able to adapt to a dislocated disc, pain may become a significant symptom. This pain forces the clinician into more aggressive approaches. Therapies that may need to be considered are arthrocentesis, arthroscopy, and arthrotomy.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


