Figure 4.24 Preoperative radiograph of teeth 24–26.
I. Diagnosis/Diagnoses
Other
- Symptomatic irreversible pulpitis tooth 26.
- Symptomatic apical periodontitis tooth 26.
J. Case Assessment
- The source of the patient’s pain in this case is inflammation of the pulp of the maxillary left first molar. The etiology of the pulpal inflammation is bacteria, likely due to a history of dental caries. Bacteria may also induce an inflammatory response in the pulp due to a crack or leaking restoration in the tooth.
- The patient’s history, signs, and symptoms are a classic example of pain due to symptomatic irreversible pulpitis.
- The diagnoses in this case were made based on the patient’s reported history of pain and the diagnostic test results. The patient’s history of pain, presence of spontaneous pain, and intense and lingering sensitivity to cold are all suggestive of a pulpal diagnosis of symptomatic irreversible pulpitis. This pulpal diagnosis was confirmed clinically by the hypersensitive and lingering response to the cold test. The periapical diagnosis of symptomatic apical periodontitis was made due to the presence of percussion sensitivity on the tooth. All diagnostic test results were assessed in relation to the adjacent teeth in the quadrant.
- The differential diagnosis could include reversible pulpitis or a non-odontogenic toothache. However, the patient’s history of pain, spontaneous pain, and lingering pain to cold clearly suggest a diagnosis of symptomatic irreversible pulpitis. In this case, the inflammation of the pulp has spread beyond the pulp and has begun to affect the periapical tissues, resulting in sensitivity to percussion.
K. Evidence-based Treatment Plan including Aims
- Treatment options for tooth 26 include: (1) nonsurgical root canal therapy, followed by a definitive build-up restoration and crown; (2) extraction, and (3) do nothing.
- The aim of the treatment is to remove the inflamed tooth pulp to eliminate the source of the patient’s pain. This can be accomplished through endodontic therapy or extraction of the tooth. After the inflamed tooth pulp is removed, the inflammation of the periapical tissues should resolve. If the patient elects to maintain the tooth through endodontic therapy, the tooth must be properly restored after root canal therapy. A crown restoration is recommended in order to prevent fracture of the tooth or recontamination of the root canal system through coronal leakage, and to provide long-term function for the patient.
- Emergency treatment plan: pulpectomy (Figure 4.25).
- Definitive treatment plan: nonsurgical root canal therapy.
- Restorative treatment plan: build-up and crown.

Figure 4.25 Extirpated tooth pulp.
L. Prognosis and Discussion
- The prognosis is favorable. When the inflamed tooth pulp is removed, the patient’s pain will resolve. If proper endodontic therapy and restoration are provided (Figure 4.26) there should be no further bacterial contamination of the root canal system. This will prevent the development of apical periodontitis, and the tooth should provide long-term function for the patient (Figure 4.27).
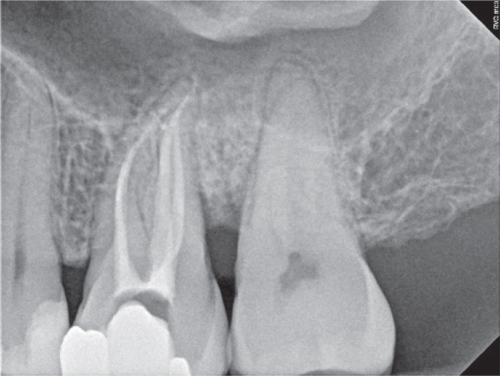
Figure 4.26 Postoperative radiograph.

Figure 4.27 The 1 year follow-up radiograph.
Background Information
- Nine percent of adult patients who visited a general dentist reported having pain related to the teeth and surrounding tissues within the past year (Horst et al., 2015). This dentoalveolar pain was the most frequently reported type of orofacial pain, and was reported more often by patients who did not receive regular dental care and those seeking treatment in community-based public health clinics (Horst et al., 2015). In a study of after-hours calls for a group of dentists over a 5-year period, 52% of calls recorded were related to acute pulpitis or apical periodontitis (Portman-Lewis, 2007). The most common treatment provided for these emergency patients was removal of the dental pulp (23% of patients) (Portman-Lewis, 2007). According to a survey of dentists in the USA in 2005–2006, over 22 million endodontic procedures including over 15 million root canals were performed annually by private practitioners in the USA (American Dental Association (ADA), 2007).
- Removal of the inflamed pulp tissue by a pulpectomy in cases of irreversible pulpitis provides significant pain relief (Menhinick et al., 2004). Removal of the pulp will eliminate the temperature sensitivity on the treated tooth. When inflammation of the pulp spreads from the coronal aspect of the tooth apically, the periapical tissues also become inflamed. The patient may then become sensitive to biting or chewing, and the clinician can reproduce this as percussion sensitivity during diagnostic testing. A pulpectomy will also help alleviate percussion sensitivity, although percussion sensitivity may take more time to completely resolve than temperature sensitivity.
Diagnostic Criteria
American Association of Endodontists (AAE) consensus conference for diagnosis of Symptomatic irreversible pulpitis (American Association of Endodontists (AAE), 2009).
Symptomatic irreversible pulpitis is based on subjective and objective findings that the vital inflamed pulp is incapable of healing and that root canal treatment is indicated. Characteristics may include sharp pain upon thermal stimulus, lingering pain (often 30 s or longer after stimulus removal), spontaneity (unprovoked pain), and referred pain. Sometimes the pain may be accentuated by postural changes, such as lying down or bending over, and over-the-counter analgesics are typically ineffective. Common etiologies may include deep caries, extensive restorations, or fractures exposing the pulpal tissues. Teeth with symptomatic irreversible pulpitis may be difficult to diagnose because the inflammation has not yet reached the periapical tissues, thus resulting in no pain or discomfort to percussion. In such cases, dental history and thermal testing are the primary tools for assessing pulpal status.
For Symptomatic apical periodontitis, see Case 4.8.
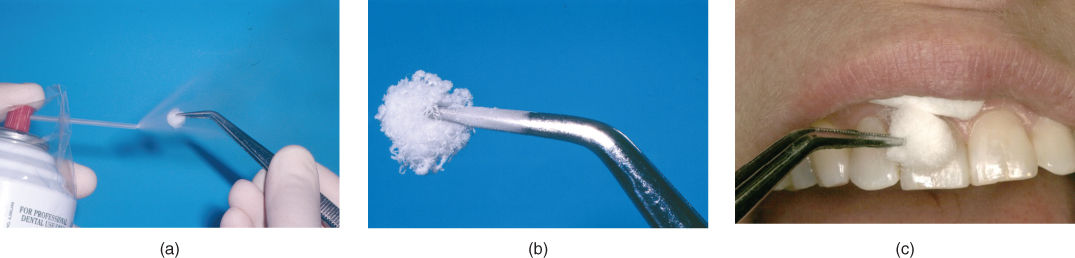
Figure 4.28 Cold testing. (a) Spraying refrigerant onto a #2 cotton pellet held by a cotton plier. (b) Cold cotton pellet ready for cold testing. (c) Placing cold cotton pellet on the facial surface of the tooth to be tested.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


