Figure 3.30 En-face photograph of patient.

Figure 3.31 Orofacial pain locations confined to masseter muscles.
B. Symptom History
- Pain is constant and moderate: 6 (NRS 0–10).
- Quality is dull, tight; and chewing hard food or opening mouth, and stress make pain worse. Medication and relaxation are ameliorating factors.
- Awake bruxism is reported (OBCL).
- First episode of facial and head pain 2 years ago treated with sporadic use of muscle relaxant (cyclobenzaprine) and NSAIDs.
- Pain is getting worse since the first episode.
- No report of facial/head trauma, closed or opening locking of the jaw.
C. Medical History
- Patient has hypertension, diabetes type 2, migraine, and polycystic ovaries. She has been treated with propanol and metformin 550 mg.
- Presence of continuous body pain (Figure 3.32), unrelenting fatigue, and sleep disturbances for a year. The pain is widespread, involving both sides of the body. It is aggravated by emotional stress and weather changes. She reported fairly bad sleep quality and she often awoke in the morning without feeling fully rested and with a sensation of muscle fatigue.
- Levels of thyroid hormone, blood calcium, cholesterol and vitamin D are normal.
- Patient did not report any aerobic physical activity.
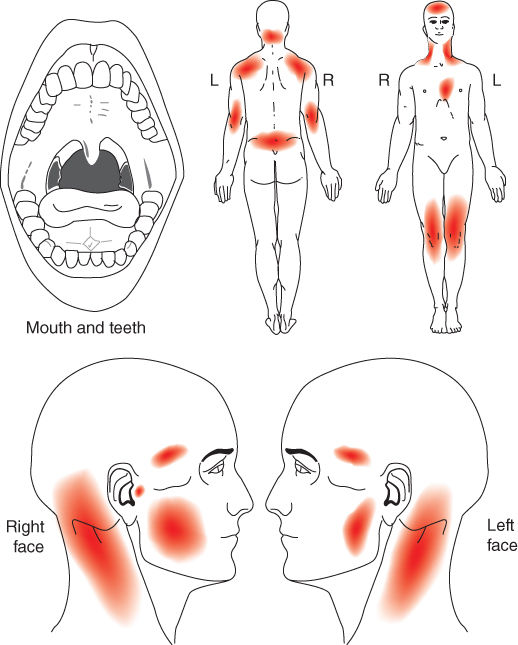
Figure 3.32 Pain drawing by patient.
D. Psychosocial History
- Patient reported loss of energy and reduced ability to concentrate in daily activities. She is under psychological treatment for anxiety disorder.
- GCPS revealed severe pain-related disability.
- PHQ-15 revealed a high number of physical symptoms.
- Fibromyalgia Symptom Scale was completed. The Widespread Pain Index (WPI) and Symptom Severity Score (SS) indicated that patient had fibromyalgia.
E. Previous Consultations and Treatments
- She visited a dentist 2 years ago. The diagnosis was TMJ arthralgia.
- She used a stabilization splint for a year without pain improvement.
- She is under orthodontic treatment.
F. Extraoral Status
Jaw movement capacity
- Straight with pain-free opening of 24 mm, maximum unassisted opening 31 mm, and maximum assisted opening 41 mm, including overbite.
- In opening movements, familiar pain was presented in bilateral temporalis, masseter, and TMJ.
- No restrictions or pain were observed in lateral and protrusive movements.
Temporomandibular joint
- No joint sound detected under manual inspection or reported by patient.
- TMJ palpation revealed familiar pain only in the right side.
Jaw muscles
- On the right side, the patient reported familiar pain with temporalis and masseter muscle palpation.
- On the left side, patient reported familiar pain with anterior temporalis and masseter (origin and body) palpation. Pain was also presented in middle and posterior temporalis.
- In bilateral masseter muscle, pressure, when maintained, elicited a referral pattern of pain to frontal and temporal area, reproducing the patient’s pain complaint.
Neck examination
- Familiar and referred pain to temporal and frontal areas when sternocleidomastoideus muscle was under sustained pressure.
G. Intraoral Status
- Teeth with braces. She presented an Angle Class I malocclusion with misalignment of the teeth.
- Wear facets were found in bilateral incisors and molars, along with indentation in tongue and buccal mucosa.
- No other significant findings.
H. Additional Examinations and Findings
- Patient was referred to a rheumatologist, who confirmed the diagnosis of fibromyalgia.
I. Diagnosis/Diagnoses
DC/TMD
- Myofascial pain with referral.
- Right TMJ arthralgia.
Expanded taxonomy for TMD
- Fibromyalgia.
Other
- Possible awake bruxism.
J. Case Assessment
- Patient fulfilled DC/TMD criteria for myofascial pain with referral. From the pain drawing it was evident that she had widespread pain, which is why she was asked to complete the WPI and SS. These indicated fibromyalgia, which was confirmed by a rheumatologist.
- The cause of the jaw pain could be muscle overload as daytime clenching was present, but was more likely a consequence of the generalized pain presenting also in jaw muscles.
- High psychological distress is commonly seen in fibromyalgia, and lack of energy and sleep disturbances are among the key symptoms.
- The high pain intensity in combination with the severe pain-related disability and psychological distress impair the prognosis, which is why multimodal and multidisciplinary treatment is recommended.
K. Evidence-based Treatment Plan including Aims
Patient education and self-management
- To improve symptoms and reduce disability levels and also manage expectations, information about diagnosis, treatment, and prognosis were given.
- Self management included:
- Visual reminders, like small stickers, strategically placed at home and at work and an application for smartphone (No Clenching app).
- Heat stimulation to improve pain by stimulation of muscle relaxation and vascular perfusion.
- Aerobic exercise (e.g., walking), to improve physical function, quality of life, and reduce pain. The “start low, go slow” strategy for any physical exercise program must be advised, which should limit adverse events and better assure adherence.
- Sleep hygiene (e.g., make sleep routine a priority, optimize relaxing sleep environment, provide advice on diet and exercise) was advised to improve sleep quality, pain scores, and mental well-being.
- To avoid the use of over-the-counter medication for pain; the overuse of these medications could contribute to pain chronification.
Pharmacologic management
- To reduce pain, naproxen 550 mg, two times a day was prescribed for 10 days. Naproxen was reported as effective for the treatment of painful TMJ.
- Amitriptyline 25 mg/day (once a day at bedtime) was prescribed for 30 days. After this period, dosage increased to 50 mg/day. Data from studies indicate that low doses (10–75 mg/day) of amitriptyline are effective for the treatment of fibromyalgia and also it is beneficial for chronic TMD pain. The analgesic effect of TCAs is thought to be independent of antidepressant effect and it should be related to their ability to increased efficacy of pain modulation, increasing the availability of serotonin and norepinephrine at the synaptic junction. Pain modulation seems to be compromised not only in fibromyalgia, but also in masticatory myofascial pain patients.
Jaw movement rehabilitation
- To improve jaw function, coordination exercises with her tongue behind the upper incisors were recommended as they can decrease pain and increase range of motion.
L. Prognosis and Discussion
- A number of health-care specialists (physical therapist, rheumatologist, and psychologist) were required to collaborate on the patient’s care. The step-by-step approach is an important way, rather than trying to solve everything at once.
- More frequent visits may be useful to emphasize the important role of multimodal treatment and to help the management of early treatment’s adverse effects, which could improve patient’s engagement in all therapies.
- The questionnaires and assessment tools, like VAS and Axis II DC/TMD criteria, must be used to assess the impact of pain across multiple domains (sleep, physical, and emotional symptoms) during follow-up sessions and to develop and prioritize treatment goals with a focus on the symptoms and domains most affected.
- Amitriptyline can improve symptoms and function; however, if necessary, it could be substituted in follow-up visits by others medications with different action to influence transmission of sensory signals via central nociceptive pathways.
- Informing patients with TMD and fibromyalgia of the limitations of treatments as well as potential benefits could be helpful. For example, medications will help to reduce symptoms but may not eliminate them altogether. However, a reduction in symptoms may allow the patient to engage in self-management and exercises.
Background Information
- Fibromyalgia is a dysfunctional syndrome with a prevalence of 2% in the general population, more frequently in females, increasing with age (Clauw, 2009).
- Patients with fibromyalgia present with chronic widespread pain and a variety of physical symptoms, including sleep disturbance, fatigue, decrements in physical functioning, and disruptions in psychological functioning such as memory problems, mood disturbances, and concentration difficulties (Clauw, 2015).
- Fibromyalgia has been shown to be very familial/genetic coupled, and environmental factors (e.g., early life trauma, physical trauma, some infections, emotional stress) may play a prominent role in triggering the development. Fibromyalgia is characterized by central disturbance with dysfunction in endogenous noxious inhibition systems, amplification in pain processing, sleep disturbance, and dysautonomia (Woolf, 2011).
- The classification of fibromyalgia according to the American College of Rheumatism (ACR; Wolfe et al., 1990) has for long been the most used for diagnosis (Fundamental points 2). New clinical criteria for the diagnosis of fibromyalgia have recently been proposed (Wolfe et al., 2011). These criteria involve WPI and SS, but exclude counting tender points as previously required by the criteria from the ACR (Fundamental points 2). There is, however, no consensus regarding which criteria should be used (Staud et al., 2010).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


