Figure 2.17 (a) Intraoral picture of 52-year-old man with ankylosing spondylitis with occlusion on only both sides premolars. Anterior open bite 4 mm. (b) Maximal range of motion increases the inter-incisal distance to 8 mm.
H. Additional Examinations and Findings
- Radiological examination of neck with flexion and extension revealed no erosions and subluxations, but a possible fibro-osseous ankylosis between C3 and C4.
- Examination of general health, including blood samples, revealed an elevated C-reactive protein (CRP) of 33 g/L and erythrocyte sedimentation rate (ESR) of 25 mm/h. Other blood tests were within normal limits.
- Panoramic radiograph, TMJ MRI and computed tomography (CT) showed limited translatory movements bilaterally (Figure 2.18).
- CT with angiography showed, in addition to erosions and ankylosis, no embedded arteries.
- Resorption of the cranial base on left TMJ.
- Caries.
- Periodontal disease.
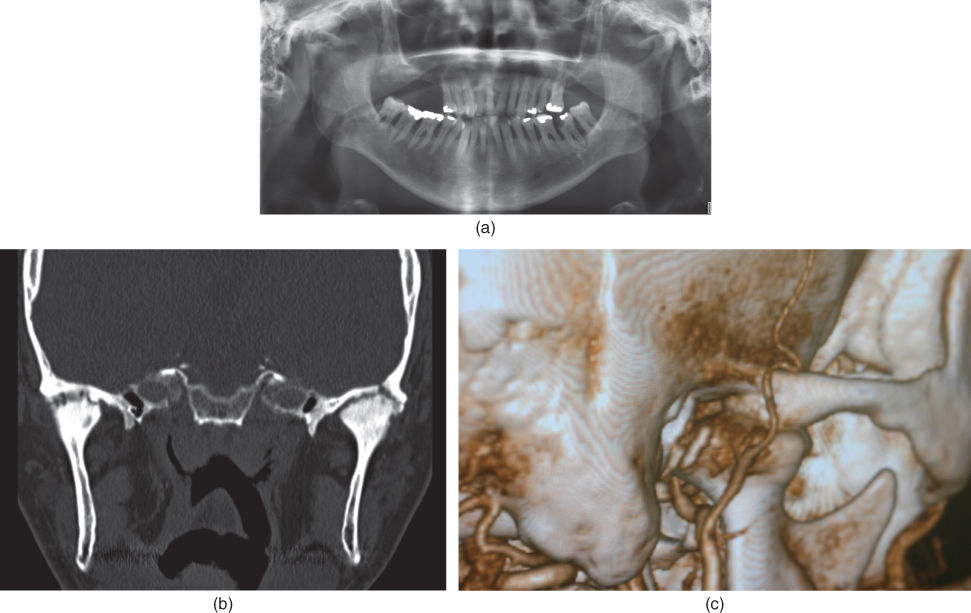
Figure 2.18 (a) Panoramic radiography illustrating dental and periodontal status and indicating pathology of both TMJs. (b) CT showing fibro-osseous changes in both TMJs. Left side with perforation to the cranial fossa. (c) CT with intravenous angiography of right-side TMJ with the maxillary and superficial temporal arteries in close relation to the TMJ. The arteries are not embedded by bone, and there is no stenosis in the arteries. Resorption of the superior and posterior part of the condyle is also observed.
I. Diagnosis/Diagnoses
Expanded DC/TMD
- Bilateral TMJ fibrous ankylosis.
DC/TMD
- Bilateral TMJ arthralgia.
Other
- Systemic ankylosing spondylitis.
J. Case Assessment
- Nutritional challenges. The patient could not attend regular meals with friends (e.g. at restaurants). He was unable to eat regular food without use of a food processer. In particular, as a chef in the petroleum production sector in the North Sea he could no longer maintain his professional career.
- Involvement of neck. This is of great importance if it is necessary to undergo general anaesthesia and intubation.
- Possible bilateral facial nerve paraesthesia after TMJ procedures may be a complication and, furthermore, cause eye problems, especially if it occurs bilaterally.
- After years with minimal use of masticatory muscles, they may be atrophied and the muscles will need comprehensive physical exercise to regain mobility and strength.
- Fibro-osseous or bony ankylosis with involvement of the cranial fossa may be a serious complication and may give intracranial infections.
K. Evidence-based Treatment Plan including Aims
Treatment goals
- Periodontal treatment.
- Dental treatment, inclusive of oral implants and prosthodontic restorations.
- Dental hygiene instructions.
- Physical therapy.
- To achieve the possibility to open jaw.
Management
- Bilateral ankylosis resection with interpositional dermis–fat graft. Procedure on left side as first operation and the right side operated 3 months later. Fat collected from the belly. Osteotomies were performed. No leakage of cerebrospinal fluid. After resection of the ankylotic condyles the maximum assisted opening was increased to 40 mm (Figures 2.19 and 2.20).
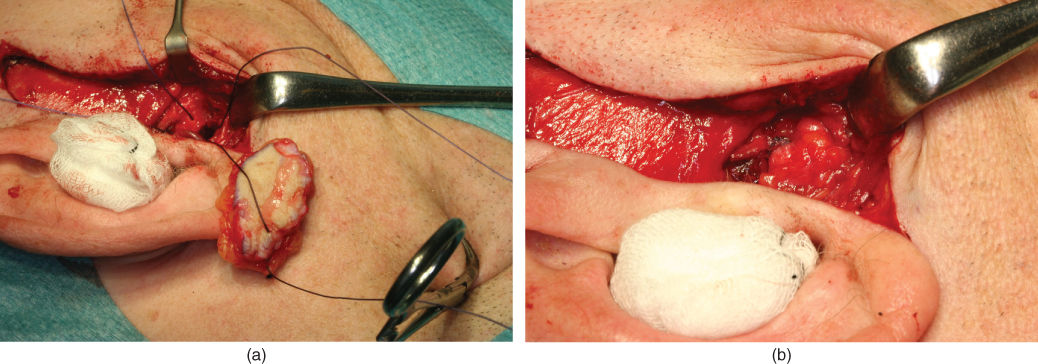
Figure 2.19 (a) Right-side ankylosis resection with placement of dermis–fat graft secured with sutures to the zygomatic arch. (b) After right TMJ ankylosis resection and placement of dermis–fat graft in the TMJ space.

Figure 2.20 Maximal range of motion 40 mm at 6 months after bilateral TMJ ankylosis resection and placement of dermis–fat graft.
L. Prognosis and Discussion
- No facial nerve paraesthesia was observed after the operations. The occlusion was stable with no vertical anterior open bite and 4 mm horizontal open bite. Physical therapy was instituted once a week, together with general physical therapy of the other joints involved. Dental and periodontal treatments were started. The plan to do implant surgery and prosthodontic treatment was not done since the patient was very satisfied with the situation.
- Re-ankylosis is possible in cases with both unilateral and bilateral fibrous or bony ankylosis. Treatment decision is difficult. Should one use ankylosis resection with ramus–condyle unit reconstruction with a prosthetic total joint or interpositional arthroplasty?
- Treatment of TMJ ankylosis with total joint prosthesis may be more predictable with regard to achieving a good occlusion compared with interpositional arthroplasty. On the other hand, total joint replacement often gives less lateral and protrusive mandibular motion.
- The reason for operation of the two sides with a 3 month interval was first the possibility of involvement of the cranial fossa on the left side, evaluation of the occlusion after resection of one side and evaluation of possible facial paraesthesia. If some complications had appeared on the one side, there was the option to cancel the operation on the other side.
- If re-ankylosis appears, one has to consider reoperation where the use of total joint replacement may be necessary.
- Facial nerve paraesthesia – if bilateral this may be a serious complication due to dryness of the eyes, with possible blindness as a result.
- Perforation to the cranial fossa may be a serious complication in cases where the arthritic process has resorbed the articular fossa.
- Alternative treatment plans could be either alloplastic total joint prosthesis or resection of ankylotic condyle with bone transplantation from rib, hip or fibula.
Background Information
- Fibrous ankylosis of the TMJ is a rare condition that may affect one or both TMJs (Loveless et al., 2010).
- The aetiology may be trauma, iatrogenic causes due to previous surgical interventions or to inflammatory diseases such as immunological diseases (e.g. rheumatoid arthritis, ankylosing spondylitis, juvenile idiopathic arthritis) (Loveless et al., 2010).
- The ankylosis will in most cases appear gradually with decreased mandibular motion as one of the clinical signs. Pain may or may not be a present.
- Erosion, destruction, bone remodelling and bone formation may be seen in the development of the fibrous ankylosis.
- Radiographically, an orthopantomogram may give the first indication of pathology of the TMJs.
- CT or CBCT is the best radiographic examination for TMJ ankylosis. MRI may give additional information about active inflammation. CT with angiography is recommended to evaluate possible vessels inside the ankylosed part of the TMJ.
- Erosion of the fossa may be a part of the process, and the cranial fossa may be involved in the resorption and bone remodelling.
- Even if there is ankylosis, the patient may have some degree of mandibular movement because of the elasticity of the mandible.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


