9 Laser-Enhanced Removable Prosthetic Reconstruction
However, a removable prosthesis may be the only treatment plan available for many patients because of finances or underlying medical conditions. Blanchaert1 lists diabetes, disorders of bone metabolism, radiotherapy, and chemotherapy as important factors in the decision to place implants. Smoking is also a significant contraindication to implant treatment. Holahan et al.2 found that implants placed in smokers were 2.6 times more likely to fail than implants placed in nonsmokers. Mundt et al.3 found similar results in their study of 663 implants placed in 159 patients. Michaeli et al.4 reported an increased risk for failure in diabetic patients. A diagnosis of Paget’s disease or other diseases of bone may also contraindicate placement of implants, depending on the quality of the bone.5
The general advantages of using lasers during removable prosthetic treatment planning are essentially the same as when using lasers in periodontal, pedodontic, cosmetic, or oral surgical treatment plans. Kesler6 enumerated the advantages of using lasers in removable prosthetics as follows:
Excision of Epulis Fissuratum
Kruger7 describes the conventional (blade) correction of epulis: excision of the fold if small, or submucosal dissection followed by sharp submucosal excision, with suturing of the flap to the periosteum. However, this method frequently fails because of extensive contracture of the vestibule, with loss of height. This will exacerbate the problem: a denture that does not properly fit in the vestibule. Lack of relapse and contracture is one advantage of using a laser versus conventional techniques.
Keng and Loh8 used a carbon dioxide (CO2) laser to remove epuli from 20 patients, with follow-up at 1 day, 1 week, and 2, 3, 4, and 8 weeks postoperatively and continuously over 2 years. No patient experienced hemorrhage, infection, aspiration, or pain that could not be relieved by common oral analgesics. No sutures or packing was used, and healing was uneventful. All patients had stable results. Interestingly, many patients were apprehensive about conventional (scalpel) surgery but agreed to participate in the study if a laser would be used. This major advantage of patient perception of the advantages of laser surgery over conventional surgery was supplemented by a second advantage: lack of wound contraction and relapse. Other advantages of laser surgery included lack of scarring, good re-epithelialization, and precise tissue destruction. The authors concluded that the CO2 laser represents a significant advance for the management of epulis fissuratum.8
In a larger study involving 126 patients with epulis, Barak et al.9 concluded that the CO2 laser is ideal for this procedure. Other authors evaluating laser treatment of epulis also report positive results. Gaspar and Szabo10 reported a relapse rate after epulis reduction with conventional methods of 12.8% versus 7.9% for laser methods. They also performed a successful epulis reduction in a hemophiliac patient with no adverse affects. Komori et al.11 performed epulis removal on seven patients using a CO2 laser without anesthesia. All lesions were successfully removed with no pain reported by the patients during the procedure.
There are no contraindications to the use of lasers for epulis treatment. Moritz12 describes the removal of an epulis in a 64-year-old diabetic patient and of an irritation fibroma interfering with a maxillary denture in an 83-year-old patient. No complications or adverse postoperative sequelae occurred in either patient.
Typical Laser Removal of Epulis Fissuratum
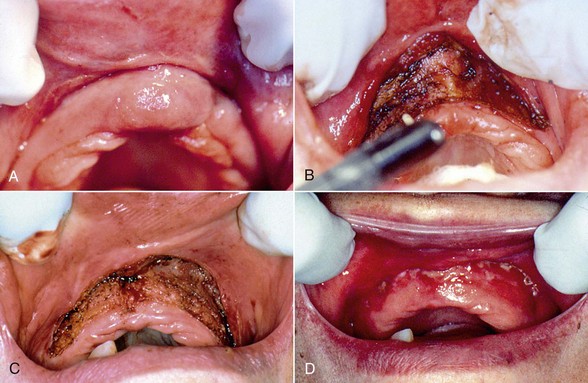
A 64-year-old edentulous man presented with elongated rolls of tissue in the maxillary mucolabial fold area (Figure 9-1, A). He was functioning with a poorly fitting, 20-year-old complete denture with no major symptoms. The flabby tissue appeared to have a central groove from the extension of the denture flange. This condition, epulis fissuratum, also called denture-induced fibrous hyperplasia (DIFH), is a common consequence of an improperly fitting denture and can generally be diagnosed based on the patient’s clinical history and findings. Laser excision is generally suggested; if the lesion size is relatively small, however, laser ablation will suffice. Because these lesions may represent a squamous cell carcinoma that has proliferated around a denture flange, suspicious tissues should be managed with excision and biopsy to eradicate the disease and rule out malignancy.13
The procedure is completed by excising the tissue beginning at the lateral margins, then proceeding toward the midline bilaterally, while retracting the tissue away from the alveolar ridge (Figure 9-1, B). If bleeding occurs, hemostasis can be achieved by defocusing the laser. A denture tissue conditioner material (e.g., Coe Comfort) should be placed in the existing denture for comfort; except for removal during daily cleaning, the patient should wear this while tissue is granulating. A fibrous coagulum will form during the initial phases of healing (Figure 9-1, C), which should not be confused with infection. Complete healing occurs within a few weeks, and if necessary, the old prosthesis may be discarded and a new prosthesis fabricated (Figure 9-1, D).
Vestibuloplasty
A common condition involves alveolar bone resorption with shallow vestibular depth, resulting in a patient’s inability to wear a denture with the desired comfort and function. Although traditionally this has been treated surgically using a scalpel, the CO2 laser is ideal in this situation for a bloodless supraperiosteal vestibuloplasty, with excellent results. Neckel14 treated 40 patients requiring vestibuloplasty with either traditional scalpel surgery or a laser. Results showed equivocal gain in vestibular height between the two groups, but with less postoperative pain and discomfort in the laser group.
Beer and Beer15 performed CO2 laser maxillary vestibuloplasty in 10 patients whose vestibular height ranged from 3 to 7 mm. A laser incision was performed from the second molar region of one side all the way to the second molar region of the contralateral side. After laser treatment, the patients’ old prostheses were adjusted with denture material to support the new vestibular heights. At the conclusion of the study, all the vestibules were increased a minimum of 3 to 8 mm. Many of the patients showed increases of 10 to 12 mm with no relapse. No complications were seen at follow-up 6 to 10 months postoperatively.
Laser Technique
Figure 9-2 illustrates a technique for laser vestibuloplasty in a patient requiring excision of an epulis and a vestibuloplasty. After administration of local anesthetic, the anterior vestibule is tensed by pulling the lower or upper lip outward. The laser is then used to create a supraperiosteal dissection.16 The tension maintained on the lip allows effortless establishment of an adequate plane of dissection. The tissue margin is then maintained in place with sutures or a stent. If desired, an autogenous or allogeneic soft tissue graft can be used to cover the denuded area. Immobilization of the graft is key to its survival, which can be accomplished with suturing or placement of a stent.17
In patients not undergoing soft tissue grafting, postoperative discomfort is minimized and may be further reduced by initial, continuous wear of a soft-relined denture or a tissue-conditioned denture, although this is not mandatory. In patients with significant resorption of the mandible, the genioglossus and mylohyoid muscle attachments often preclude adequate extension of the lingual flange of the denture.18 In this case a floor-of-mouth lowering procedure can be performed to increase lingual vestibular height. This can be done with a laser as previously described, again using supraperiosteal dissection and either sutures or a stent to fix the lowered tissue in place. At least half the musculature attached to the genial tubercles should remain to ensure adequate function of the tongue and oropharyngeal muscles.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses