CHAPTER 6
Harvesting Bone from the Mandibular Symphysis
The mandibular symphysis is a good source for procuring smaller grafts, such as those generally used for implant procedures.1, 2 The anterior mandible offers either a block or a particulate configuration of bone. In a block configuration, the symphysis can typically provide a sufficient amount of bone for increasing width deficiencies by 4 to 7 mm, length deficiencies by 15 to 20 mm (about one to three teeth), and height deficiencies by 10 mm. Studies on cadavers suggest this site can yield an average block of 21 × 10 × 7 mm or more.3, 4 Although the ascending ramus may provide more graft material, the mandibular symphysis provides a block graft with more cancellous bone than do other intraoral sites.5 Unlike the ramus, which studies have shown is a viable source for autogenous bone for ridge augmentation procedures,6, 7, 8, 9 the symphysis yields corticocancellous particulate material in addition to a block graft. As a donor site, the anterior mandible offers moderate to relatively low morbidity10 and minimal graft resorption following placement.11, 12, 13, 14, 15, 16 This autogenous source has been used successfully to restore many types of defects, including Class III ridge defects (both vertical and buccal bone loss) in the anterior maxilla and other locations (as a block configuration) 17, 18, 19, 20, 21 and for sinus elevations (as a particulate configuration).11, 22, 23, 24, 25, 26, 27, 28, 29
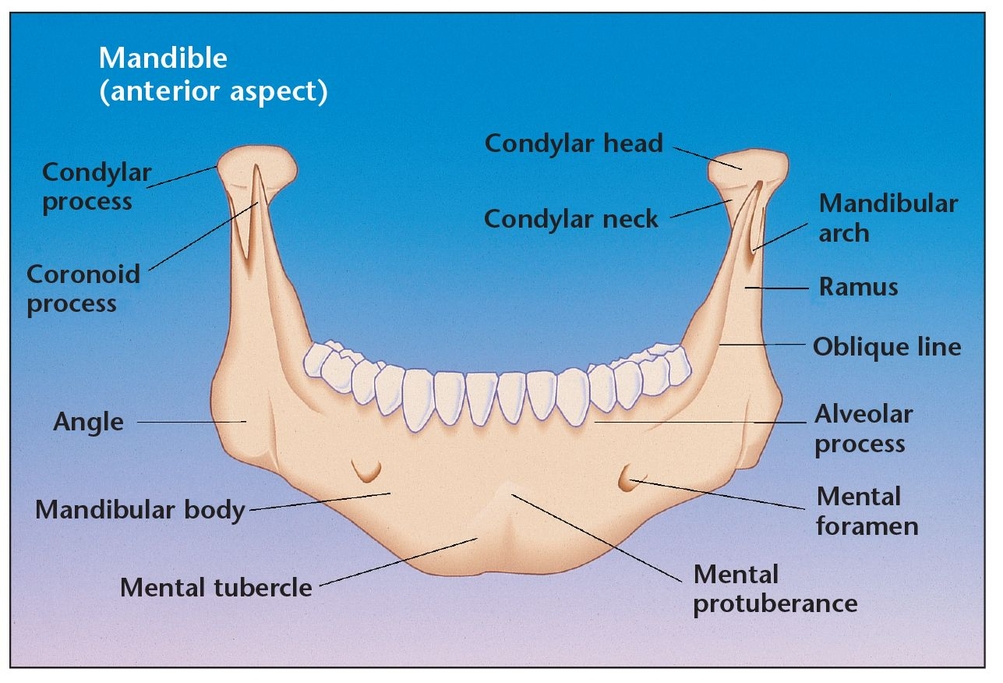
Before attempting block graft harvesting from the mandibular symphysis, the clinician should have extensive knowledge of the anatomic landmarks of the mental area (including the inferior alveolar nerve path and anterior loop, mental foramen, incisive nerve, and mandibular width) as well as the probable anatomic variations from case to case.
Biology of the Mandibular Symphysis As a Donor Site
An understanding of the biologic, mechanical, and topographic aspects of the mandible is essential for proper evaluation of the structure as a source of autologous bone grafts (Fig 6-1).30, 31, 32, 33 The most popular graft donor sites are chosen for their cancellous cellular density or for their block configuration to provide structural support. Harvested endosteal osteoblasts and cancellous marrow stem cells must be transferred to the jaw in a viable state and placed into tissue that has sufficient vascularity to diffuse nutrients to the cells before revascularization. New capillaries can then bud into the graft to form a more permanent vascular network. The osteocompetent marrow cells are quite resilient, capable of living outside natural bone for at least 4 hours without losing more than 5% of their viability if stored appropriately.14
Cortical membranous grafts revascularize more quickly than endochondral grafts, contain denser cancellous elements,34 and resorb considerably less.35, 36, 37 This fact may explain why chin grafts, which consist primarily of cortical bone with few osteogenic cells, show good incorporation, less volume loss, and shorter healing times than grafts from the ilium. The biochemical similarity between bone from the mandibular symphysis and the maxillofacial region may partly explain this superior incorporation. 14 Although some research suggests that there is little difference in results when chin or iliac crest grafts are used38 and that use of the iliac crest results in generally low morbidity,39 a histologic study comparing maxillary bone grafts with either ilium or chin donor material also revealed a better bone quality result when chin grafts were used.18
Using the mandibular symphysis as a donor site allows the clinician to operate in the same field as the recipient site. This ability is often an important benefit to patients, particularly those who are only partially edentulous. Although cutaneous scarring is eliminated with an intraoral donor site, some patients raise concerns about chin deformation. Deformation is not ordinarily a problem with the procedure, but the clinician may take additional steps to prevent it by placing a fill material at the donor site. Chin ptosis can also be avoided if the clinician takes care not to completely deglove the mandible and, most importantly, if he or she sutures the tissues back to their original position.
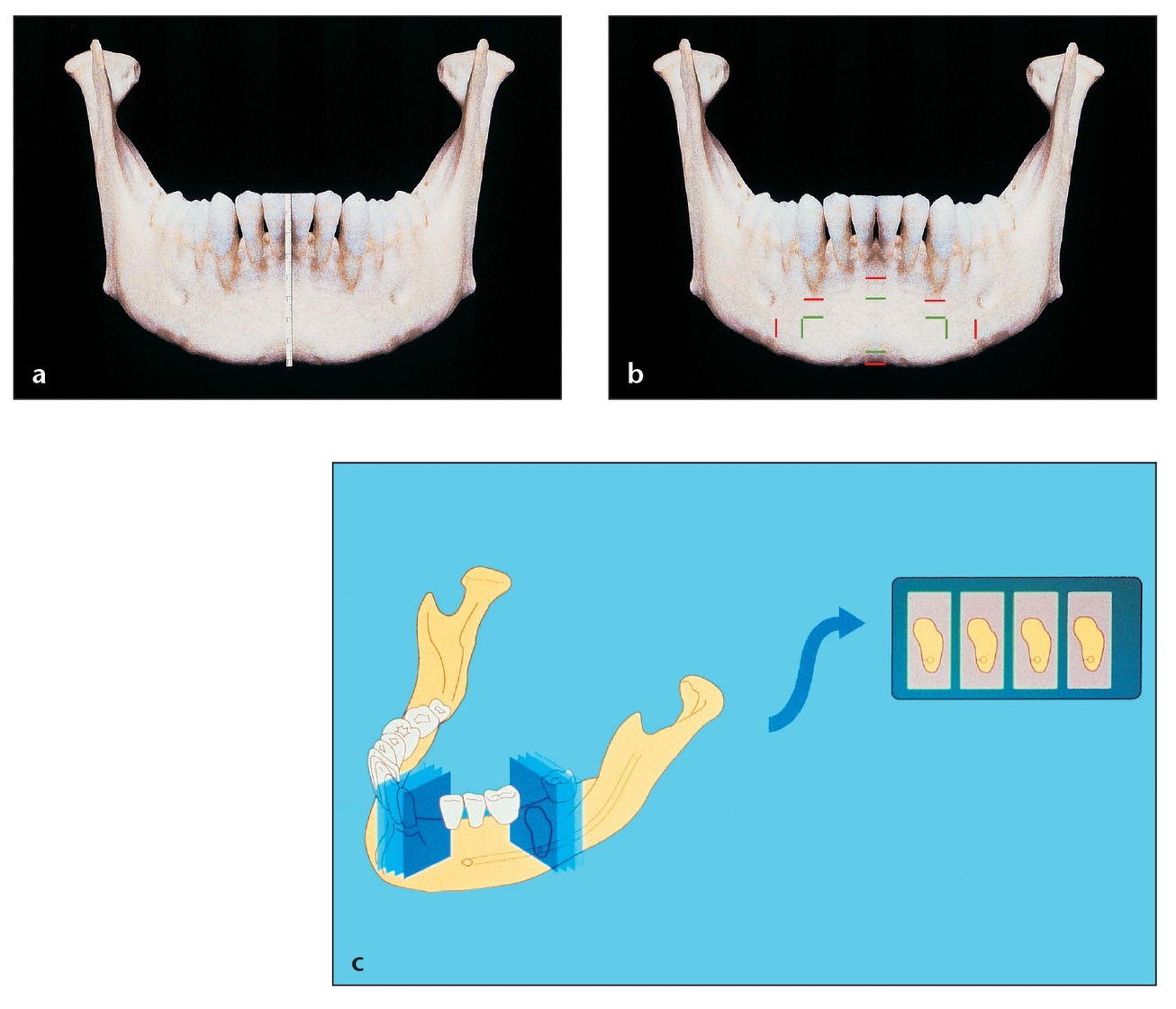
(a) Accurate measurements of the apices of the anterior mandibular teeth must be obtained through methods such as periapical radiographs, so that safety markings can be made prior to harvesting bone from the anterior mandible.
(b) Panoramic, periapical, and lateral cephalometric radiographs help establish the working space for bone harvesting, enabling the clinician to avoid tooth apices, the mental foramen, and the mandible’s inferior border. Using radiographs, the vital structures to avoid can be measured and marked as indicated in red. The green marks indicate the periphery of the safe zone for harvesting.
(c) Determining the shape and thickness of the anterior mandible at the level where the bone blocks will be taken is essential. A sagittal view with a simple lateral cephalometric radiograph can aid in assessing shape and thickness, along with palpation of the buccal and lingual walls. Computed tomography scans can help determine bone thickness in cases with limited harvesting area.
Many patients do experience reduced sensitivity in the chin or anterior mandibular teeth following procurement from the mandibular symphysis. These effects are typically minimal and eventually disappear, but patients must be informed about this possibility.40, 41 Such sensory changes may be caused by a stretching of the mental nerve or by a disruption of the incisive canal contents, even when an appropriate border depth is maintained below the apices of the anterior tooth roots during chin bone harvesting.11,18 Proper procurement technique, as described in the next section, minimizes this risk, as does careful patient selection (Fig 6-2).
Patients who are not good candidates for using the mandibular symphysis as a graft donor site include (1) those whose mandibles exhibit long anterior tooth roots; (2) those who have inadequate mandibular height or width for sufficient graft procurement; and (3) those who have a defect exhibiting gross vertical loss or who require width augmentation that spans more than four teeth.
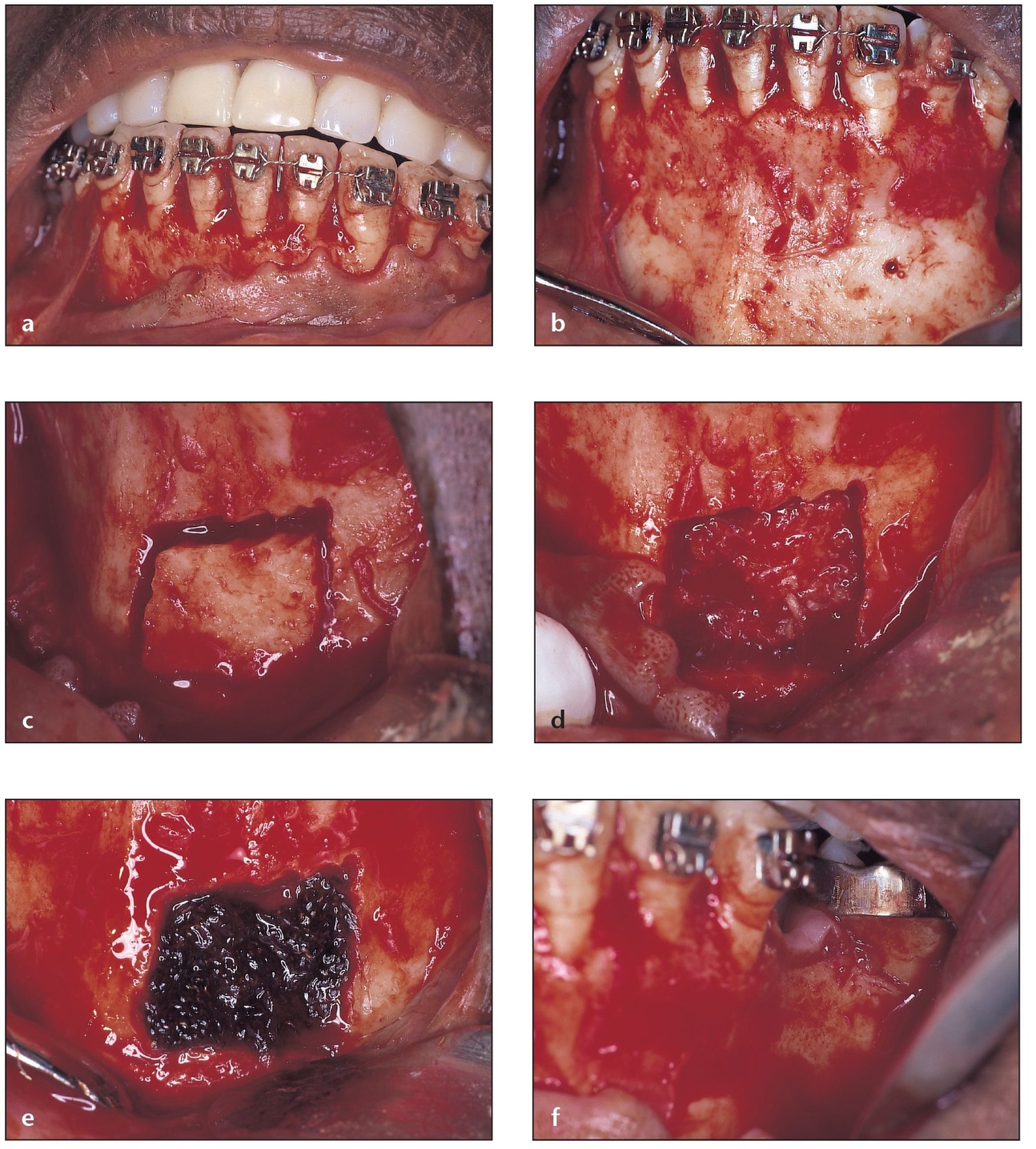
Fig 6-3 The intrasulcular method is indicated for patients with a low vestibule, a tense mentalis posture, and a donor site free of abnormal periodontal circumstances.
(a) An intrasulcular incision is used for this patient, who has thick, flat papillae and broad tooth contacts, requiring a bone graft to an adjacent area (the left posterior mandible). Here, access can be gained to both the donor and recipient sites with one flap. The mental nerve should be protected during flap reflection.
(b) The flap is reflected to expose the donor and recipient sites, to provide adequate visualization of the surgical sites, and to minimize harm to the flap during graft harvesting.
(c) A template created at the recipient site is used to cut an appropriate-sized block at the donor site.
(d) After the block is removed, additional cancellous marrow can be harvested with a no. 2 Molt curette (G. Hartzell & Son, Concord, CA).
(e) After removal of the necessary cancellous marrow, the donor site is packed with Avitene (MedChem Products, Woburn, MA) for hemostasis and then later with a bone putty or allogeneic graft material.
(f) The recipient site is the area of the missing mandibular left first molar. The ridge width is inadequate for implant placement and requires grafting to augment it.
Methods for Harvesting Monocortical Bone Blocks from the Mandibular Symphysis
The clinician obtains the chin bone graft from below the apices of the mandibular incisors and canines. Panoramic and lateral cephalometric radiographs should be taken so that the clinician can evaluate the donor site; he or she must locate the mental foramen as well as determine the form and size of the anterior teeth and the volume of bone available for harvesting. The anteroposterior dimension of the anterior mandible should be determined on a lateral cephalometric radiograph. Additionally, periapical radiographs can be used to determine the measurements of the mandibular tooth roots. It is also important for the clinician to evaluate the recipient site before obtaining the donor material. This evaluation allows the clinician to assess the amount of donor bone needed, to carefully plan the incision and flap reflection design, and to identify any unforeseen complications that preclude harvesting the bone graft. Local anesthesia includes bilateral mandibular blocks of 0.5% bupi-vacaine with 1:200,000 epinephrine and 2% lidocaine with 1:100,000 epinephrine or articaine with 1:100,000 epinephrine, which are locally infiltrated in the labiobuccal vestibule.
(g) The recipient site is shaped to accommodate the block and perforated with a small drill to add bleeding points for the release of endosteal osteoblasts for optimal bone maturation.
(h) The harvested block is shaped and modified to provide for optimal fit in the defect.
(i) The block graft is set in place to ensure proper fit before stabilization and the creation of fixation screw holes.
(j) The block is fixed in place with screws. The small voids are mortared with particulate graft. Graft material can then be placed in the donor site, and the area is ready for flap replacement and suturing.
There are three incision options for accessing the donor site, depending on the mandible’s musculature and the periodontal status of the mandibular anterior teeth.42, 43 Each has distinct indications, advantages, and disadvantages.
Intrasulcular Method
This straightforward method is indicated for patients with a low vestibule, a tense mentalis posture, and a donor site free of abnormal periodontal circumstances. An intrasulcular incision is made on the facial aspect of the anterior mandibular teeth, as far distal as the canines. A full-thickness flap and the fibrous periosteal layer are then reflected apically to expose the anterior surface of the mentum. The advantages of this incision method include minimized bleeding and trauma and facilitated flap retraction. Disadvantages include suturing difficulty as well as possible recession and loss of bone at the alveolar crest resulting from surgical trauma and loss of periosteal blood supply to part of the facial plate, which can occur if the bone labial to the teeth is thin enough to eliminate marrow space between the cortical bone plates (Fig 6-3).44
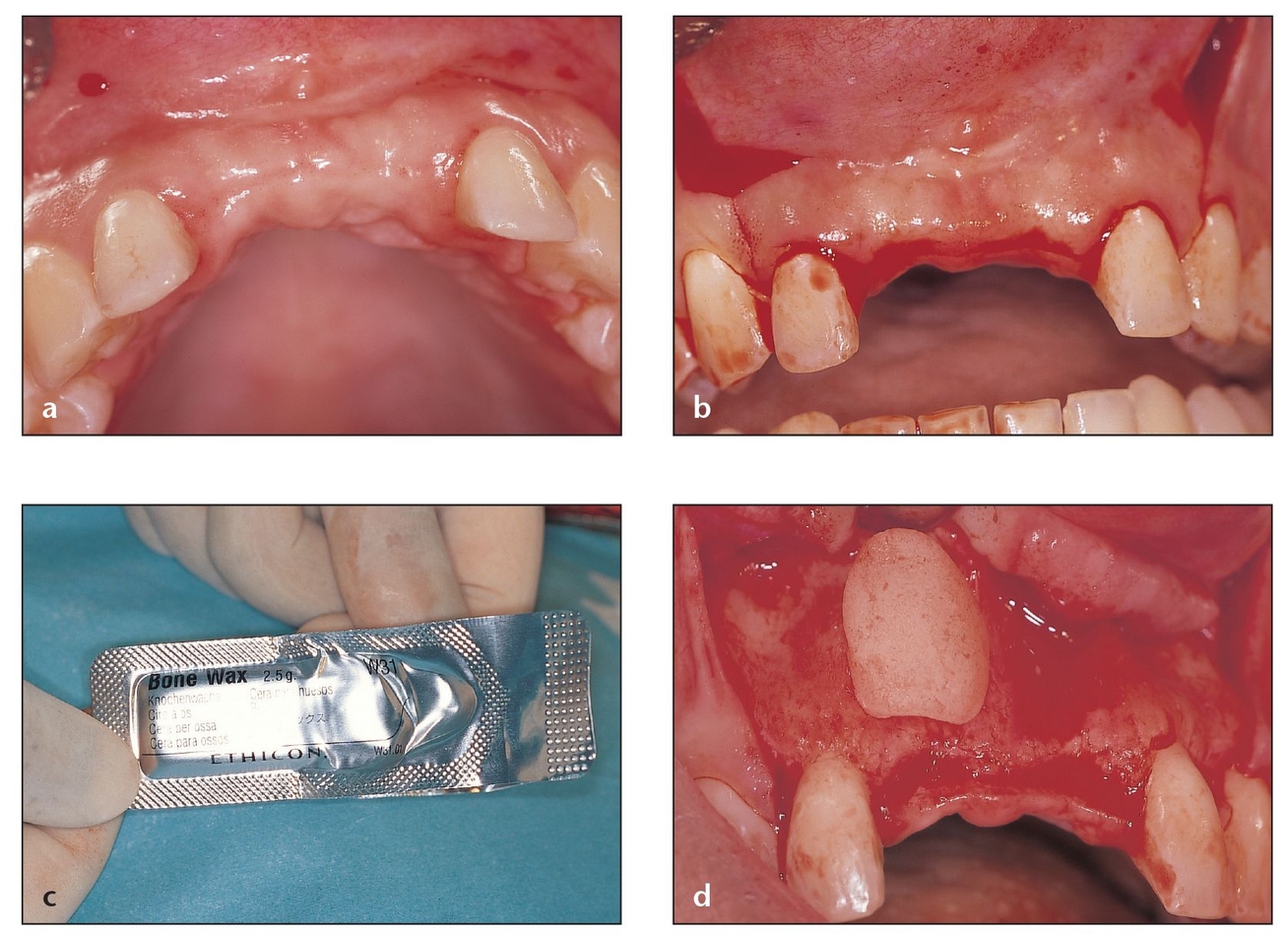
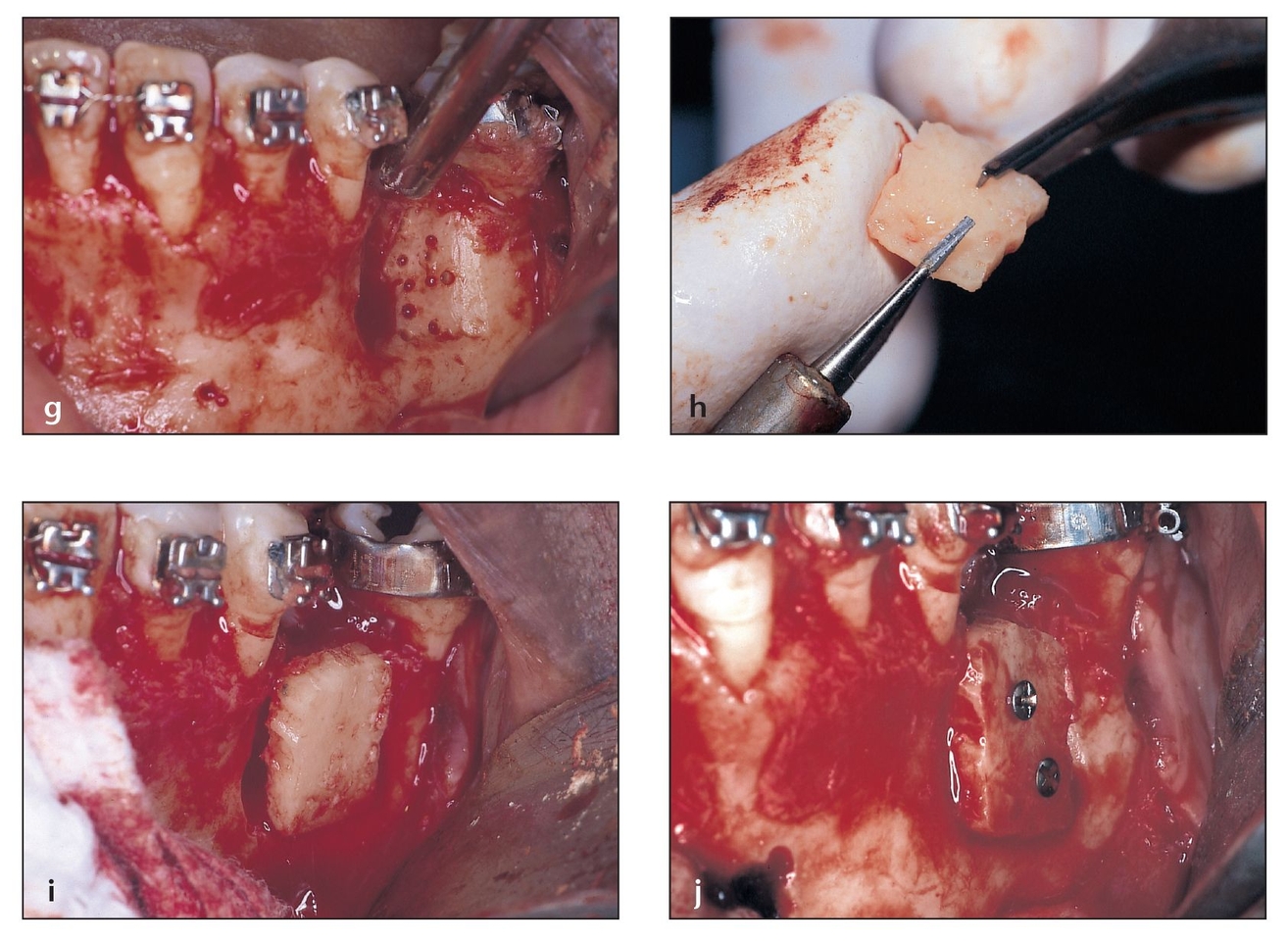
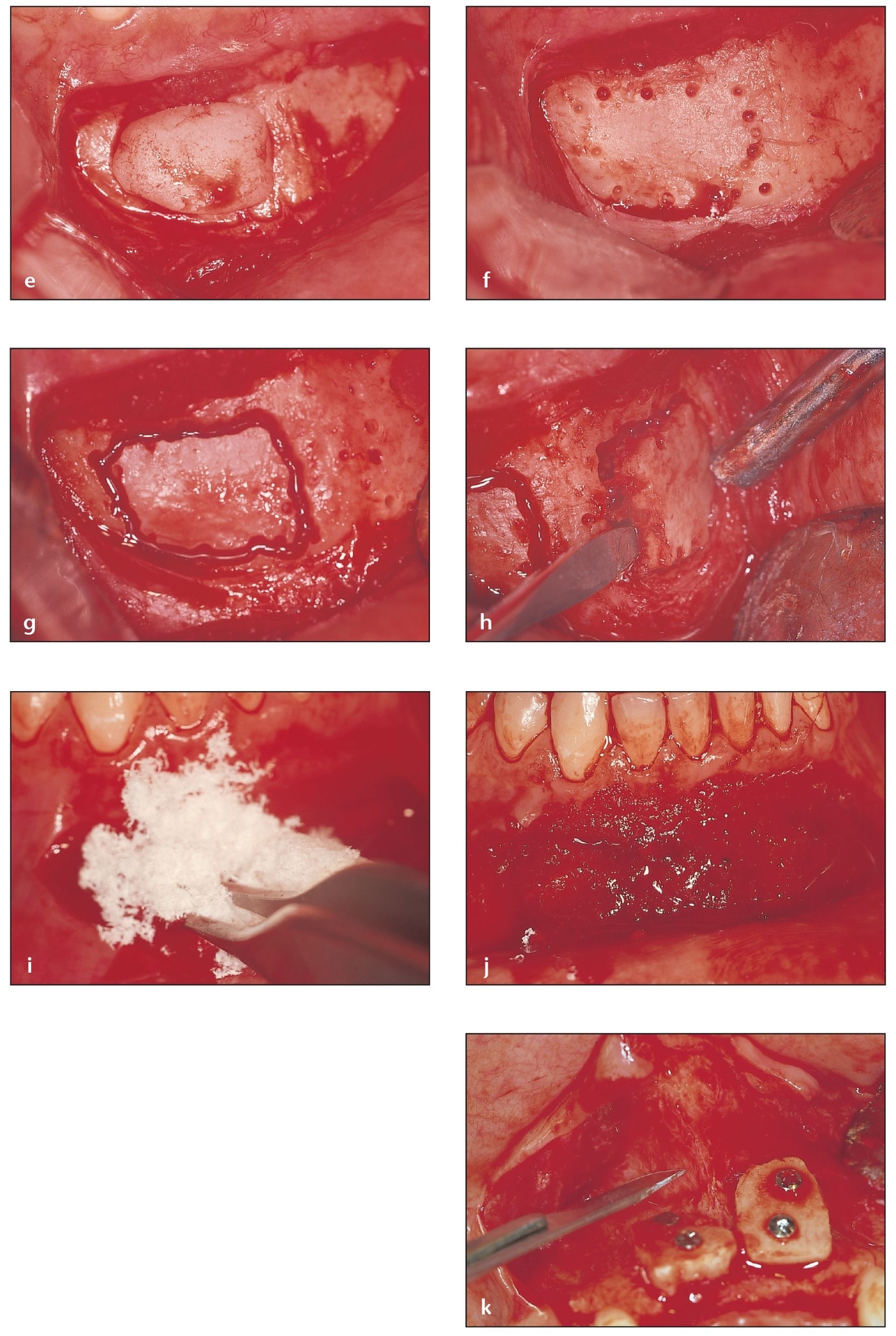
Fig 6-4 The vestibular method is indicated when there is marginal inflammation or existing alveolar bone loss around the incisors.
(a) Two maxillary central incisors and part of the alveolar ridge have been lost as a result of trauma. There is insufficient bone to accommodate dental implants.
(b) A midcrestal incision is made at the edentulous area; vertical incisions to release the flap are made distal to the lateral incisors.
(c) Bone wax, available in sterile packages, is ideal to mold over the bone defect and for hemostasis.
(d) Bone wax can be shaped over the deficient anterior maxilla to help assess the amount of bone volume needed. The bone wax mold can then be used at the donor site as the template for harvesting a bone graft of the correct size and shape.
Vestibular Method
The vestibular method is indicated when there is marginal inflammation or existing alveolar bone loss around the incisors. A vestibular incision is made in the alveolar mucosa 5 mm or more apical to the mucogingival junction between the premolars. Avoiding the mental nerve bundles is crucial to the success of this method; a blunt dissection can be used to uncover the bundles if needed. Limiting the distal extent of the vestibular incision to the canine area can also reduce the incidence of temporary mental nerve paresthesia.13 Reflection of a full-thickness flap exposes the donor site after the clinician makes an incision apicolingually in the direction of the bone and through the mentalis muscle.44
The advantages of this incision method include no interference with the gingiva surrounding the anterior mandibular teeth, no mentalis muscle detachment (thus facilitating accuracy when repositioning it), reduced risk of facial ptosis, closer proximity of the intact part of the periosteum to the donor site, better lateral access, and ability to use a two-step suturing approach (first the muscle, then the mucosal tissues). Disadvantages include greater challenges associated with the initial shallow incision site and the need for subsequent blade redirection,19 more bleeding and edema, and invisible scarring (Fig 6-4).
(e) The bone wax mold (surgical template) is placed at the ideal position for harvesting bone. It can be moved before perforations are made to mark the size of the bone block needed. Note that a vestibular incision is used in this case.
(f) The initial perforations to guide the final cuts are made with a no. 1701 cylindrical bur (Brasseler, Savannah, GA). Corrections to the size and shape of the block can still be made at this crucial step.
(g) With the same no. 1 701 bur, the final perforations in the bone are connected to outline the block. All of the cuts are made with the bur placed perpendicular to the bone, except the anterior vertical one, which should be made with the bur at a 45-degree angle to facilitate the process of sliding in the chisel and lifting up the block.
(h) The bone block is carefully chiseled out and easily extracted if the osteotomy is deep enough (the complete active part of the bur) and the entire outline, even the corners, is cut completely.
(i) Avitene, a hemostatic agent that consists of easily handled collagen fibers, is used to control bleeding.
(j) Once hemostasis has been achieved, the donor site can be sutured.
(k) Bone blocks are placed at the recipient site and fixed with titanium screws. The flap should be properly dissected to separate the mucosa from the periosteum and thus permit tension-free coverage of the grafted area.
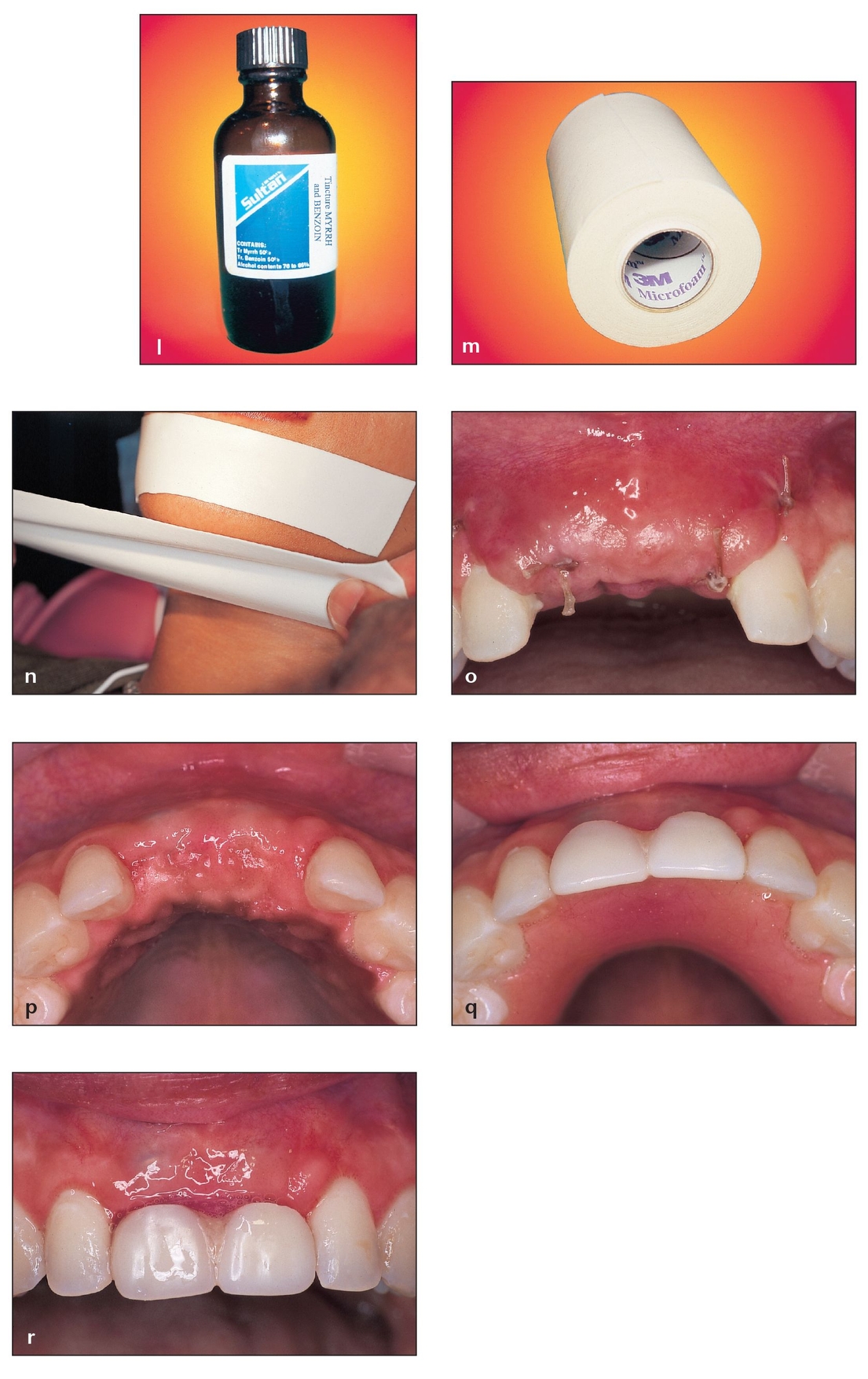
(l) To aid adhesion and minimize irritation from the adhesive, the skin of the mental area is painted with tincture of myrrh and benzoin prior to applying the adhesive surgical dressing.
(m, n) A stretchable microfoam tape is ideal to help keep the soft tissues of the mental area together. The stretchable dressing is placed with one strip pulled back underneath the lower lip and another pulled upward from below the chin.
(o) A 1-week postsurgical view of the grafted site shows that the sutures have not yet been removed and that some swe/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


