14
The paedodontic–orthodontic interface
T.J. Gillgrass
Chapter contents
14.2 Recognition of malocclusion
14.2.2 Need and demand for orthodontic treatment
14.2.3 Referral for orthodontic advice
14.3 Primary to mixed dentition
14.4 Extraction of children’s teeth
14.4.1 Extraction of primary teeth
14.4.3 Enforced extraction of primary teeth
14.4.4 Enforced extraction of first permanent molars
14.5 Correction of cross-bites
14.5.2 Posterior cross-bite with displacement
14.5.6 Incisor spacing—midline diastema
14.6 Anomalies of eruption—the ectopic maxillary canine
14.6.1 Prevalence of impacted maxillary canines
14.6.3 Radiographic assessment
14.6.6 Other anomalies of eruption
14.7 Anomalies of tooth size and number
14.7.3 Anomalies of tooth size
14.8 Orthodontics and dental trauma
14.8.1 Orthodontic movement of traumatized teeth and non-vital teeth
14.9 Complications of orthodontic treatment
14.9.2 Treatment failure and relapse
14.9.3 Predisposition to dental-related disorders
14.10.1 Dental care for patients with cleft lip and palate
14.10.2 Orthodontist within the cleft team
14.10.3 Paediatric dentist within the cleft team
14.1 Introduction
The long-term management of a child’s developing occlusion often benefits greatly from a good working relationship between the paediatric dentist and the orthodontist. Typical problems range from minimizing damage to the occlusion caused by enforced extraction of poor-quality teeth, through the management of specific local abnormalities such as impacted teeth, to referral for comprehensive treatment of all aspects of the malocclusion. This chapter discusses the principles of when to refer to a specialist colleague, and looks at some common clinical situations where collaboration is often needed.
14.2 Recognition of malocclusion
14.2.1 Orthodontic assessment
From the age of 8 years all children should be screened for the presence of malocclusion when they attend for a routine dental examination. Although orthodontic treatment is usually carried out in the late mixed and early permanent dentition, some conditions benefit from treatment at an earlier stage. The screening need only be a brief clinical assessment, but it should be carried out systematically to ensure that no important findings are overlooked.
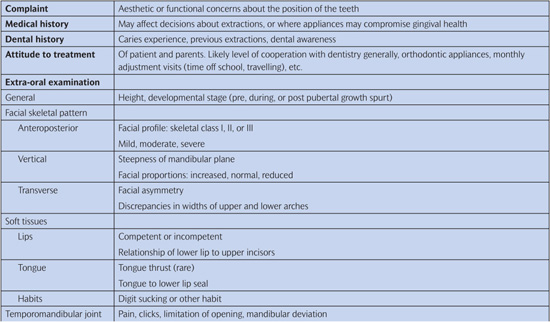
An outline of a basic orthodontic assessment is given in Table 14.1. With practice this can be carried out quite quickly to give an overall impression of the nature and severity of a malocclusion. In essence, it comprises assessments of the following elements:
• the patient’s awareness of their malocclusion (the complaint, if any);
• their general level of dental awareness;
• an extra-oral examination of facial form (skeletal pattern and soft tissues);
• general oral condition—oral hygiene and tooth quality;
• the presence or absence of all teeth;
• the alignment and form of each arch;
• the teeth in occlusion.
Table 14.1 Orthodontic assessment
Good-quality study models are often helpful when planning orthodontic treatment, and full orthodontic records comprising study models, relevant radiographs, and photographs should be obtained before any active treatment is started. Full-face and profile photographs are a record of facial form, including lip morphology. Intra-oral photographs are a further record of the malocclusion, give some indication of the standard of oral hygiene, and are valuable where enamel defects are present before treatment.
14.2.2 Need and demand for orthodontic treatment
The Index of Orthodontic Treatment Need (IOTN) is based upon the severity of the malocclusion, and has been developed to try to establish a consensus within the profession as to which malocclusions will gain a worthwhile benefit from orthodontic treatment (Brook and Shaw 1989). It is important to emphasize that IOTN does not indicate the difficulty or complexity of treatment, as mild malocclusions often need extensive and sophisticated treatment if any improvement is to be made at all. Other indices have been developed to assess the complexity (Index of Complexity, Outcome, and Need (ICON)) and success of treatment (Peer Assessment Rating (PAR)). The IOTN has two components.
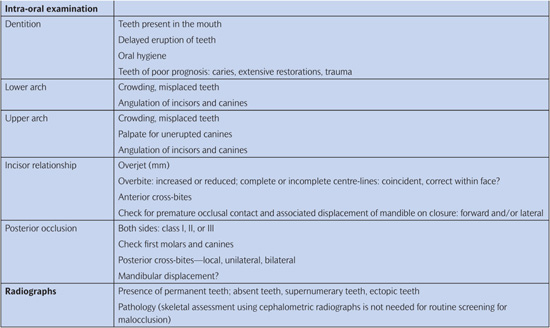
1. The Dental Health Component categorizes malocclusion into five grades (Table 14.2) according to severity, based upon current evidence at its inception for the detrimental effects of various occlusal features. It is based on an index from the Dental Board of Sweden. A malocclusion is graded according to its worst feature, i.e. it is not cumulative. Therefore once mastered, it is quick to apply.
Grade 1 no need
Grade 2 little need
Grade 3 borderline need
Grade 4 need
Grade 5 great need
To assess the malocclusion a ruler has been developed although this is not essential for scoring. The acronym MOCDO is used to systematically analyse each feature of the malocclusion (M issing, O verjet, Crossbite, D isplacement of contacts, O verbite). Each occlusion can be numerically graded with an indication for treatment and an associated alphabetical descriptor describing the feature for which it has been scored.
Table 14.2 Dental Health Component of the Index of Orthodontic Treatment Need
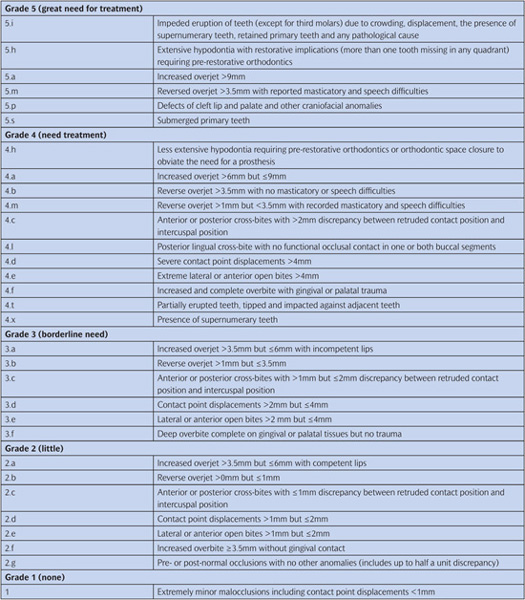
2. The Aesthetic Component uses a scale of 10 photographs showing different levels of dental attractiveness (Fig. 14.1). The appearance of the dentition is rated using the photographs as a guideline. Grades 1–4 indicate little or no need for treatment on aesthetic grounds, grades 5–7 are borderline, and patients in grades 8–10 would clearly benefit from orthodontic treatment. However, it is difficult to be truly objective when making judgements of this kind about an individual’s appearance, although when scoring the aesthetics the operator should assess the aesthetic component score. Particular difficulty is found when analysing class III malocclusion and anterior open bite as this type of malocclusion does not appear within the aesthetic component. It should be emphasized that the scoring of the aesthetics using the component is based on equivalence rather than matching the malocclusion to one that is within the component.
Demand for orthodontic treatment is affected by many factors and not necessarily by need. Females, those in higher socio-economic groups, and those in areas with a plentiful supply of orthodontic provision appear the most likely to seek treatment. Patients vary enormously in how they perceive their own dental appearance, with some apparently being unaware of obvious malocclusions while others express dissatisfaction about very minor irregularities. Thus demand for treatment depends in part upon the severity of the malocclusion as perceived by patients, and particularly by the parents, rather than by the dentist. This is backed up by studies suggesting that malocclusion has an effect on the quality of life of the patients and the parents.
Long-term studies have questioned the long-term health and psychological benefit of orthodontic treatment, but this must be weighed against the relatively short-term psychological boost that orthodontics brings to a patient during what is, in the case of adolescents, an emotional rollercoaster.
There is little doubt that demand continues to increase, particularly in the adult population. This continues to create increasing strain where state-funded treatment is still available and inevitably leads to the use of indices (IOTN) to decide who is eligible for the treatment.
Figure 14.1 The Aesthetic Component of the Index of Orthodontic Treatment Need. (R. Evans and W. Shaw 1987. Reproduced with kind permission of the Editor of the European Journal of Orthodontics.)
14.2.3 Referral for orthodontic advice
Before referring a patient for orthodontic advice it is important to ensure that his/her dental health is under control and that the referring practitioner has made some assessment as to the severity of the orthodontic need. The referring dentist can give the orthodontist a lot of invaluable information.
Timing of referral
The right time for orthodontic intervention will vary according to the condition, but if specialist advice is needed it is better to refer too early than too late. Often, a good time is as the first premolar teeth are erupting. The majority of orthodontic treatments are carried out in the late mixed and early permanent dentition, but some conditions can be treated earlier (see Section 14.4) and some treatments, such as functional appliances, depend on active facial growth and should not be delayed too long before starting. It is important that prior to referral the patient’s oral hygiene has reached an adequate standard for treatment and caries is under control. There may be some instances where referral is sought for extraction decisions on carious teeth where an assessment of long-term prognosis is helpful to the decision-making process. Important information to include on your referral is the patient’s name, address with postcode, date of birth, and telephone number. The patient’s medical practitioner should be included, particularly for hospital-based referral, and any previous correspondence reference. Key information regarding the clinical condition includes:
• past medical and dental history;
• reason for referral;
• patient’s/parents’ attitude to treatment in general and likelihood of cooperation with future orthodontic treatment if required;
• radiographs where taken.
(See Key Points 14.1.)
14.3 Primary to mixed dentition
The dentist is responsible for noticing deviations from normal in the development of the occlusion. To do this, the practitioner must have a thorough knowledge of ‘normal development’ (see Chapter 1).
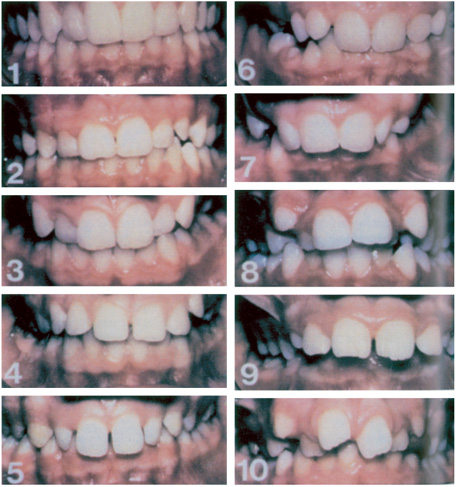
The primary dentition usually erupts between the ages of 6 months and 2½ years. The classic sequence of eruption is given in Chapter 1, with lower teeth erupting before uppers. However, deviation from this ‘normal’ sequence is not unusual (Fig. 14.2).
14.3.1 Primary dentition
The permanent teeth erupt from the age of about 6 years, usually in two stages. The first stage, with eruption of the first molars and incisors, takes place up to the age of 9 years and the second stage, including premolars and canines, occurs between the ages of 10½ and 12 years. The key for the practitioner is to ensure sequence and symmetry of eruption, as a change in either may represent abnormal development and warrant radiological investigation.
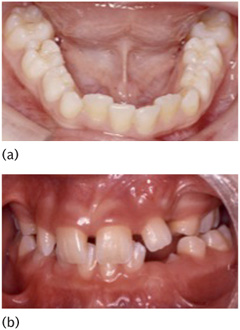
As the incisors erupt it is not unusual for the lower to appear slightly crowded (Fig. 14.4) and upper to appear slightly spaced. Crowding in the lower labial segment is usually relieved through transverse expansion and when the lower deciduous canines are lost. The upper arch spacing is frequently associated with fanning of the incisor crowns and is described as the ugly duckling stage of development. This incisor spacing will usually close spontaneously as the upper permanent canines erupt.
14.3.2 Early mixed dentition
The primary dentition classically presents as spaced and the molars often present with a ½ class II molar relationship or ‘flush terminal plane’ (Chapter 1, Fig. 1.18). It is essential for this spacing to be present, as without it crowding in the permanent dentition is likely. Malocclusion at this stage is merely noted, although it is unlikely to improve particularly in the case of a significant class III incisor relationship (Fig. 14.3), although intervention would not be considered at this stage. Habits are common and depending upon the extent of the habit, be it dummies or digits, malocclusion may exist because of it.
A supernumerary tooth may occur in the primary dentition and usually erupts. The likelihood of its being followed by a permanent successor is up to 50%, and it should be identified to parents and noted for future assessment.
It is important for the dentist to recognize these signs of normal development so that he/she can give some reassurance to the patient and parents if they are concerned. The spacing and diastema between the central incisors should not be mistaken for that due to other causes (see later). The early mixed dentition is a useful time for orthodontic assessment, as once the incisors have erupted there is a break in the eruption period until the upper premolars and lower canines start to appear at the age of 10½ years and this period allows simple interceptive measures. Interceptive measures are often designed at this stage to reduce the severity/complexity of a malocclusion rather than eliminate it completely, and are frequently the first part of a more complex orthodontic plan.
Figure 14.2 An unusual sequence of eruption in the primary dentition.
Figure 14.3 Class III incisor relationship in primary dentition.
Figure 14.4 (a) Mild lower labial segment crowding and (b) fanned upper incisors on first eruption of the incisors.
Things to consider and possible interceptive measures include the following:
• Monitor eruption of incisors and first molars, paying attention to sequence and symmetry.
• Extract primary teeth displacing permanent successors.
• Possible balancing extractions of primary teeth to prevent centre-line deviation.
• Check long-term prognosis of first permanent molars and extract if necessary.
• Correct cross-bites (anterior or posterior) with associated mandibular displacement.
• Remove supernumeraries causing displacement or impeded eruption (central incisors and median diastema).
• Severe jaw discrepancies requiring early specialist referral (class III, class II, and bilateral cross-bites).
• Habit deterrents.
• Space maintenance.
Some or all of these may require specialist referral.
14.4 Extraction of children’s teeth
The extraction of teeth in children may be needed as part of orthodontic treatment, or may be necessary because of caries, trauma, or developmental anomalies. The extraction of teeth in the mixed dentition for purely orthodontic reasons, usually crowding, can sometimes be helpful, but managing the enforced extraction of carious or poor-quality teeth is a matter of trying to minimize disruption of the developing dentition.
14.4.1 Extraction of primary teeth
In general, where a child has crowding, the extraction of primary teeth will worsen this as adjacent teeth will be able to drift into the resultant space (Fig. 14.5). Normally the resultant space loss is greater in the maxilla than the mandible. Usually, it is the teeth distal to the extraction that migrate forwards as a result of mesial drift. This drifting is generally unhelpful where the extraction is enforced, but in some rare situations it can be harnessed to help with the management of dental crowding.
As there is an increase in the size of the arches during the mixed dentition stage, decisions about the treatment of crowding should be deferred until the permanent incisors have erupted for at least a year, usually at about 8½–9 years of age. Historically where severe crowding existed, the extraction of primary teeth might have been considered at this point as part of a programme of serial extractions. However, this is unusual with modern orthodontic techniques other than for children where cooperation with orthodontic treatment is unlikely. Where the crowding is mild or moderate, the decision should be delayed until the permanent canines and premolars are erupting.
Figure 14.5 Complete space loss in the upper arch after early extraction of carious upper first primary molars.
Figure 14.6 Retention of upper primary central incisors and deflection of the permanent successors.
The term balancing extraction refers to the contralateral tooth in the same arch. This is usually carried out to prevent centre-line shift. Compensating extraction refers to the equivalent tooth in the opposite arch. The rationale for this is based on the assumption that such an extraction will maintain the occlusal relationship.
Extraction of retained primary teeth
Suspicions should be raised where the difference between the exfoliation of contralateral teeth is greater than 6 months. Primary teeth should also be removed where they are partially exfoliated but causing deflection of a permanent successor (Fig. 14.6). If this is done early it will lead to normalization of the permanent tooth position.
14.4.2 Serial extraction
Serial extraction is a form of interceptive orthodontic treatment which aims to relieve crowding at an early stage so that the permanent teeth can erupt into good alignment, thus reducing or avoiding the need for later appliance therapy. It consists of a planned sequence of extractions.
1. Primary canines—extracted as the permanent lateral incisors erupt to allow them space to align.
2. First primary molars—about 1 year later, or when the roots of the first primary molars are at least half resorbed, to encourage eruption of the first premolars. In the lower arch these often tend to erupt after the canines.
3. First premolars—on eruption to make space for the eruption of the permanent canines into alignment.
In effect, the extraction of primary canines transfers the crowding from the incisors to the canine regions where it is more easily treated by extracting the first premolars. It is essential to carry out a full orthodontic assessment before embarking on a course of serial extractions. The intended advantage of serial extraction is to minimize or eliminate the need for appliances to align the arches after the permanent teeth have erupted. Sometimes this is very successful (Fig. 14.7), but the results can be disappointing. The great disadvantage of serial extraction is the multiple episodes of extractions, starting when the child is quite young. The primary canine extractions should usually be balanced by removing the contralateral canine to prevent a centre-line shift, but it is not necessary to compensate by extracting the canines in the opposite arch. (See Key Points 14.2.)
14.4.3 Enforced extraction of primary teeth
The main complication of the enforced extraction of poor-quality primary teeth is mesial drift of the teeth distal to the extraction space, causing crowding of the permanent successors. The extent to which this occurs is determined by:
• the tooth that is extracted
• the age of the patient
• the arch from which it is extracted
• the amount of pre-existing crowding present at the time of extraction.
In general terms the younger the patient the greater the pre-existing crowding, and the more distal the tooth the greater the space loss by mesial migration. Space loss also tends to be greater in the maxilla than the mandible where unerupted posterior teeth have a distal inclination and tend to tip and rotate mesially. In this section we shall use the terminology balancing and compensating. It should be borne in mind that many of the original ‘rules’ for balancing and compensating are from an era where correction of centre-lines and molar–canine relationships was challenging because of the limitation of appliances and provision of orthodontic care. Well-managed modern orthodontic techniques make such corrections possible, although not necessarily straightforward. As such, any decision as to whether to extract a sound deciduous tooth for balancing and compensating reasons should be weighed against the trauma of such a procedure to the child.
Figure 14.7 (a) Before extraction of primary canines. (b) Aged 10½: 6 months before extraction of first premolars. Upper canines palpable in buccal sulcus, lower canines crowded buccally. (c) Aged 13: excess space in lower arch. (d) Aged 15: upper spaces closed and lower spaces reducing. (Courtesy of Mr T.G. Bennett.)
1. Primary incisors Premature loss usually causes virtually no drifting of other teeth, but if done very early may delay the eruption of the permanent incisors. Loss of a permanent incisor is a very different matter.
2. Primary canine Loss causes some mesial drift of the buccal segment, depending upon the degree of crowding. There is also drift of the incisors into the space, which causes a centre-line shift towards the extraction site (Fig. 14.8). Ideally this should be prevented by balancing the extraction with loss of the contralateral canine, particularly as this is to be completed under general anaesthetic.
3. Primary first molar Loss of a primary first molar allows more mesial drift of the teeth distal to it than with the loss of a canine. There may also be some effect on the centre-line (Fig. 14.9), although this is likely to be less pronounced than that with loss of a canine. Balancing of a sound first primary molar would not necessarily be indicated unless general anaesthetic is considered. Where the distribution of caries indicates loss of a primary canine on one side and a primary first molar on the other, these extractions can be regarded as balancing each other reasonably well and the contralateral teeth can be retained.
Figure 14.8 Early mixed dentition where early loss of the lower right primary canine has resulted in mesial drift of the buccal segment and loss of space. There also appears to be a centre-line shift to the right.
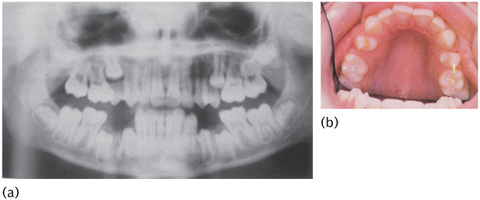
4. Primary second molar Loss allows significant mesial migration of the first permanent molar in that quadrant, causing potentially severe local crowding with displacement or impaction of the second premolar, especially in the upper arch where mesial drift is greatest (Fig. 14.10). In principle, however, the loss of a primary second molar should be avoided if at all possible, especially in the upper arch. A space maintainer, either removable or fixed, can be considered unless the patient’s caries rate is high or the oral hygiene is poor, which is frequently the case in patients requiring early extraction of primary second molars. Primary second molar extractions should never be balanced on the contralateral side as there is very little effect on the centre-line and the potential crowding becomes even more complicated.
In general, there is no need to compensate primary tooth extractions with extractions in the opposing arch. (See Key Points 14.3.)
Figure 14.9 The lower left first molar has been extracted in the mixed dentition. There has been some space loss but the effect on the centre-line has been minimal.
Figure 14.10 Localized crowding of upper second premolars on (a) OPG and (b) clinically due to the early loss of primary upper second molars. (Courtesy of Professor J.H. Nunn.)
14.4.4 Enforced extraction of first permanent molars
First permanent molars are very rarely the teeth of choice for extraction for orthodontic reasons—in practice, their removal often makes treatment more difficult.
• The space they provide is remote from the labial segments and is poorly placed for either the relief of anterior crowding or overjet reduction.
• Depending on the timing of the extractions, much of the space is lost to mesial migration of the second molars, especially in the upper arch.
• The behaviour of the lower second molars following loss of the lower first permanent molars is fairly unpredictable and is greatly influenced by the timing of the extractions.
In general, therefore, first permanent molars are only extracted if their long-term prognosis is felt to be poor because of caries or increasingly hypoplasia. In an ideal world where the loss of one or more first molars is necessary in the mixed dentition, the management of the extractions would depend on whether or not the patient is likely to have active treatment with orthodontic appliances in the future—often a difficult judgement to make. However, owing to caries and the nature of compliance in patients who present with extensive caries, the decision is frequently enforced (Fig. 14.11).
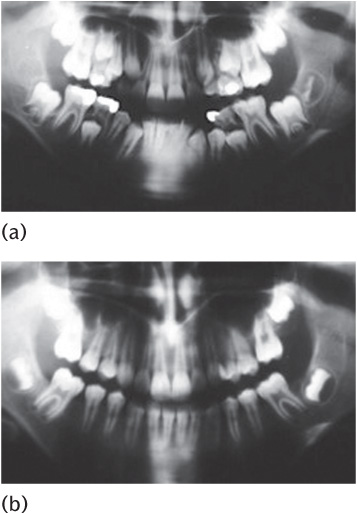
A panoramic radiograph must be taken to confirm the presence of all permanent teeth (except third molars) before finalizing the extractions. Where optimal space closure (Fig. 14.12) is the goal, particularly in the lower arch, the radiographic examination should show:
• a 15–30° angle between the long axes of the first and second molars;
• overlap between the crypt of the second molar and the mesial root of the first molar;
• formation of the bifurcation of the second molars.
In the following discussion the presence of all permanent teeth is assumed—if a premolar is congenitally absent, the first molar in that quadrant should be saved if possible.
Extractions where no orthodontics is planned
The objective is to minimize disruption of the occlusion. Following the extraction of a first molar, the paths of eruption of adjacent unerupted teeth alter, and erupted adjacent and opposing teeth also start to drift. Many of these changes are unhelpful, but some can be used to advantage with careful planning.
1. Lower arch In general, the most obvious change is mesial drift of the second molar. However, some distal movement of premolars and canines may also be expected in the lower arch. The extraction of first molars can be a convenient way of relieving premolar crowding, especially in the lower arch. In the lower arch the timing of the extraction is important. If it is carried out very early the unerupted lower second premolar migrates distally, sometimes leaving a space between the first and second premolars if the arch is uncrowded (Fig. 14.11). If it is carried out late, as or after the lower second molars erupt, that tooth tilts mesially under occlusal forces and can cause an occlusal interference, especially if the opposing upper first molar over-erupts into the lower extraction space (Fig. 14.13). There is often residual space mesial to the tilted second molar and this poor relationship with the second premolar may cause a stagnation area. These unwanted effects can be minimized in two ways:
Figure 14.11 Spaces between the lower first and second premolars resulting from very early extraction of the lower first molars.
Figure 14.12 (a) Pre-extraction and (b) good space closure following loss of all four first permanent molars.
(i) extraction of the upper first molar—this eliminates the problem of over-eruption of the opposing first molar and removes the occlusal contact which exaggerates mesial tilting of the lower second molar (Fig. 14.14);
(ii) optimal timing of the extractions—usually at about 8½–9½ years of age (Fig. 14.15).
2. Upper arch The behaviour of the second molar is more predictable in the upper arch, although timing is still important. The tendency to mesial drift is much greater than in the lower arch, and there is almost no distal drift of the upper premolars. If the upper first molar is extracted early, the unerupted second molar migrates mesially so that it erupts into the position of the first molar (Fig. 14.10). If the second molar has erupted before the extraction, it still migrates forward, taking up most or all of the space depending on the degree of crowding, and it usually tilts mesially and rotates mesiopalatally about the palatal root. However, compensating extraction of the lower first molar is not indicated (Fig. 14.16).
Balancing extractions of the contralateral first permanent molars are not routinely necessary unless they are also in poor condition. Where the arch is crowded, an extraction on the opposite side is usually needed to relieve crowding. If the first permanent molars are in good condition, extraction of first premolars may well be more appropriate. A balancing extraction may prevent any shift of the centre-line, although this is likely to be minimal and is not an indication for extraction by itself. (See Key Points 14.4.)
Extraction where orthodontic treatment is p/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


 Key Points 14.1
Key Points 14.1



 Key Points 14.2
Key Points 14.2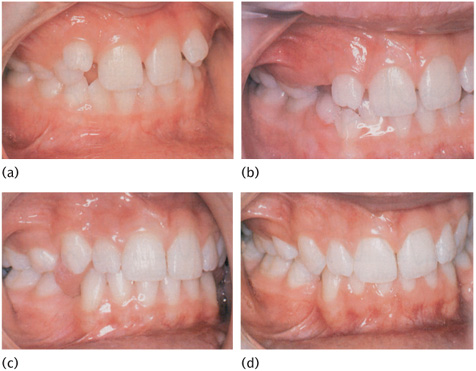

 Key Points 14.3
Key Points 14.3

 Key Points 14.4
Key Points 14.4