14 Odontogenic Cysts
The tooth develops from ingrowth of the lining of the primitive stomodeum called the dental lamina. The dental lamina forms tooth buds for the primary and the permanent dentition (Fig. 14-1), and after odontogenesis, remnant epithelium are left behind as rests. The epithelium of odontogenic cysts is thought to arise from stimulation of such residual odontogenic rests (e.g., rests of Serres in the gingiva or rests of Malassez around the tooth roots in the jawbones) (Fig. 14-2).

FIGURE 14-2 Rest of Malassez (arrow) in the periodontal ligament (fibrous tissue that attaches the tooth to bone).
Odontogenic Cysts
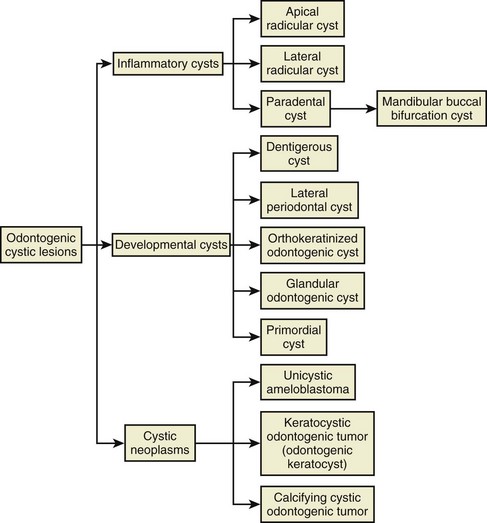
Cystic lesions in the jawbones are either odontogenic or nonodontogenic in their derivation. All odontogenic cysts are inflammatory, developmental, or, less commonly, neoplastic in nature, and the putative epithelium from which they derive may be rests of Malassez, dental lamina rests, reduced enamel epithelium, degenerated enamel organ, or, in rare cases, the epithelium of the surface mucosa (Fig. 14-3). In general, inflammatory odontogenic cysts have proliferative epithelium, and developmental odontogenic cysts have uniformly thin epithelium, although inflammation may lead to epithelial proliferation. The most common cyst is the radicular cyst (>50%), followed by the dentigerous cyst and keratocystic odontogenic tumor (odontogenic keratocyst).
Inflammatory Cysts
Apical and Lateral Radicular Cyst and Periapical Granuloma
Clinical Findings
• A cyst may or may not manifest as a swelling, depending on the size; the tooth may or may not be painful; a well-circumscribed radiolucency is present at the apex (apical radicular) or on the side (lateral radicular) of a nonvital tooth; there may have been prior root canal (endodontic) therapy (Fig. 14-4, A and B).
• Residual cyst refers to any odontogenic cyst in the alveolar bone where a tooth had been extracted and is most often a residual apical radicular cyst (see Fig. 14-4, C)
Etiopathogenesis and Histopathologic Features
• A radicular cyst is lined by nonkeratinized stratified squamous epithelium that usually proliferates in a plexiform or retiform pattern and exhibits spongiosis and neutrophilic exocytosis; the wall is composed of edematous granulation tissue and often scar tissue, many plasma cells, Russell bodies, lymphocytes, foamy macrophages, and sometimes abscesses are present (Fig. 14-5); curetted specimens may show only granulation tissue with focal lining epithelium (Fig. 14-6).
• Hyaline lamellar or globular structures of odontogenic origin (Rushton bodies) may be present within the epithelium (Fig. 14-7); epithelial loss is often associated with cholesterol granulomas.
• Foreign material from root canal filling is often seen: gutta percha is yellowish or brownish green, granular, and slightly refractile (Fig. 14-8); cements, in particular epoxy resin (such as AH Plus [Dentsply International, York, Pa], which contains zirconium and iron oxides and calcium tungstate), is usually refractile and crystalline in an eosinophilic background (Fig. 14-9); amalgam tattoo may be present from previous root apex excision (apicoectomy).
• Hyaline ring (pulse) granuloma (likely a foreign body reaction to exogenous material) consists of hyalinized rings with central and/or surrounding giant cells; foreign material is sometimes identified (Figs. 14-10 and 14-11).
• Radicular cysts from the apices of maxillary molars may be lined by respiratory epithelium (Fig. 14-12); fragments of sinus mucosa, however, signify an oroantral communication and must be reported; fragments of sinus inflammatory polyps may be present—exhibiting few to no mucous glands, eosinophilic coagulum, and eosinophils (Fig. 14-13).

FIGURE 14-11 Giant cell hyaline rings showing center of rings composed of granulation tissue with giant cells at the periphery.
Differential Diagnosis
• Any inflamed intraosseous, odontogenic, or other cyst may appear similar.
• If epithelium is not present, the diagnosis is periapical granuloma (Fig. 14-14); sheets of plasma cells are common in periapical granulomas, and they should not be overdiagnosed as plasmacytomas (Fig. 14-15).
• Periapical scar shows only fibrosis, sometimes with inflammation (Fig. 14-16).
• Chronic active periodontal disease appears similar histologically, but clinically, the tooth is surrounded by a periradicular radiolucency; disease starts either from an apical radicular cyst that grows very large and combines with an overlying periodontal bone defect or from periodontal disease starting from the surface of the bone and extending downwards to encompass the entire tooth.
Gadbail AR, Chaudhary M, Patil S, Gawande M. Actual Proliferating Index and p53 protein expression as prognostic marker in odontogenic cysts. Oral Dis. 2009;15:490-498.
Jones AV, Craig GT, Franklin CD. Range and demographics of odontogenic cysts diagnosed in a UK population over a 30-year period. J Oral Pathol Med. 2006;35:500-507.
Neville BW, Damm DD, Allen CM, Bouquot J. Oral and Maxillofacial Pathology, 5th ed. Philadelphia: Saunders; 2009.
Philippou S, Ruhl GH, Mandelartz E. Scanning electron microscopic studies and x-ray microanalysis of hyaline bodies in odontogenic cysts. J Oral Pathol Med. 1990;19:447-452.
Philipsen HP, Reichart PA. Pulse or hyaline ring granuloma. Review of the literature on etiopathogenesis of oral and extraoral lesions. Clin Oral Investig. 2010;14:121-128.
Schulz M, von Arx T, Altermatt HJ, Bosshardt D. Histology of periapical lesions obtained during apical surgery. J Endod. 2009;35:634-642.
Tripi TR, Bonaccorso A, Rapisarda E, Bartoloni G. Proliferative activity in periapical lesions. Aust Endod J. 2003;29:31-33.
Mandibular Buccal Bifurcation Cyst
Clinical Findings
• Children in the first decade (mean age of 7 years); 38% bilateral
• Swelling and pain in the area of the first permanent molar; radiolucency around a vital first molar that extends from the furcation (where roots diverge) to the apex of the tooth causing tilting of the roots lingually (best seen on occlusal radiograph); periosteal reaction usually present (Fig. 14-17)
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses