Diagnosis of Temporomandibular Disorders
“THE MOST IMPORTANT THING YOU CAN DO FOR YOUR PATIENT IS TO MAKE THE CORRECT DIAGNOSIS. IT IS THE FOUNDATION FOR SUCCESS.”
—JPO
TO MANAGE MASTICATORY DISORDERS effectively one must understand the numerous types of problems that can exist and the variety of etiologies that cause them. Separating these disorders into common groups of symptoms and etiologies is a process called diagnosis. The clinician must keep in mind that for each diagnosis there is an appropriate treatment. No single treatment is appropriate for all temporomandibular disorders (TMDs). Therefore making a proper diagnosis becomes an extremely important part of managing a patient’s disorder. In many instances the success of the therapy depends not on how well the treatment is performed but instead on how appropriate the therapy is for the disorder. In other words, proper diagnosis is the key to successful treatment.
A diagnosis is achieved by careful evaluation of information derived through the history and examination procedures. This information should lead to the identification of a specific disorder. If a person has a single disorder, diagnosis becomes a relatively routine procedure. The clinician should remember, however, that there are no rules limiting an individual to just one disorder at a time. In fact, many persons who have suffered for more than several months are likely to present with more than one disorder. It is the clinician’s responsibility to identify each disorder and then (when possible) to prioritize them in order of their significance. This can be a complex task. For example, there are various possible relationships between just two general problems: a disc derangement disorder and a masticatory muscle disorder. If the patient reports with only joint pain or only muscle pain, diagnosis becomes very routine. However, many patients will have both joint and muscle pain; it then becomes important to identify the relationships of these, since treatment is quite different.
Suppose a person falls and sustains a blow to the chin and jaw. A disc derangement disorder can develop. After several days of joint pain, the muscles become secondarily involved as a mechanism of restricting jaw movement (protective co-contraction). When the patient reports to the clinician’s office, both joint pain (i.e., pain in the intracapsular tissues) and muscle pain are present. The information received during the history and examination should assist in determining that the patient has a primary problem with the joint and a secondary problem with the muscles. Once proper treatment is extended to the joint, the joint symptoms will resolve and so will the secondary muscle pain. If, in this instance, the muscle pain is treated but not the joint pain, the treatment will likely fail, since the primary disorder has not been managed.
The same problem can occur in reverse with a masticatory muscle disorder that increases the clinical symptom of clicking in the joint. The patient reports with muscle pain and joint clicking. If the clicking alone is treated, the painful muscle will remain. Treatment should be directed toward the primary diagnosis, not the secondary. The history and examination must assist the clinician in determining this order. The clinician should also realize that the patient may be suffering from both a muscle disorder and a joint disorder that are unrelated to each other. Generally in this instance, the chief complaint should be addressed first.
Diagnosing Pain Disorders
In disorders where pain is the primary symptom, it is imperative that the source of the pain be identified. If it is primary pain, this will not be difficult, since the source and the site are in the same location (Chapter 2). With primary pain the patient will point directly to the source of pain. However, if the pain is heterotopic, the patient will direct attention to the site of pain, which may be quite remote from the actual source of the pain. Treatment will be effective only if it is directed at the source and not at the site of the pain.
One key to locating the source of pain is that local provocation should accentuate it. But this rule does not always apply. When local provocation does not increase the pain, one should be very suspicious that the pain may be heterotopic. In other words, if a patient is complaining of pain in the TMJ area, he or she should also complain that it hurts to open and chew (local provocation). If the patient does not report any functional problem with jaw movement, the TMJ may be merely the site of pain without being involved pathologically. It is the clinician’s job in this instance to continue to examine the patient for the source of the pain.
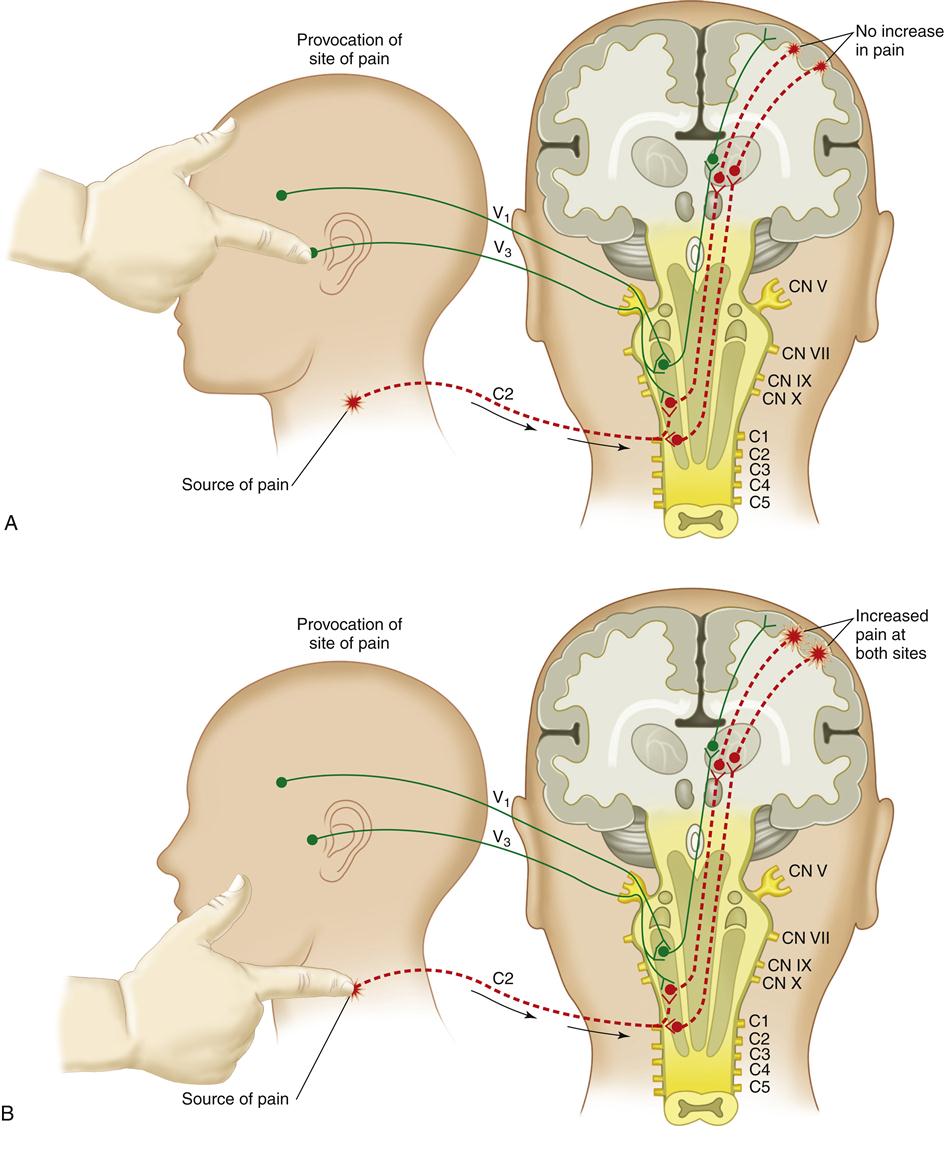
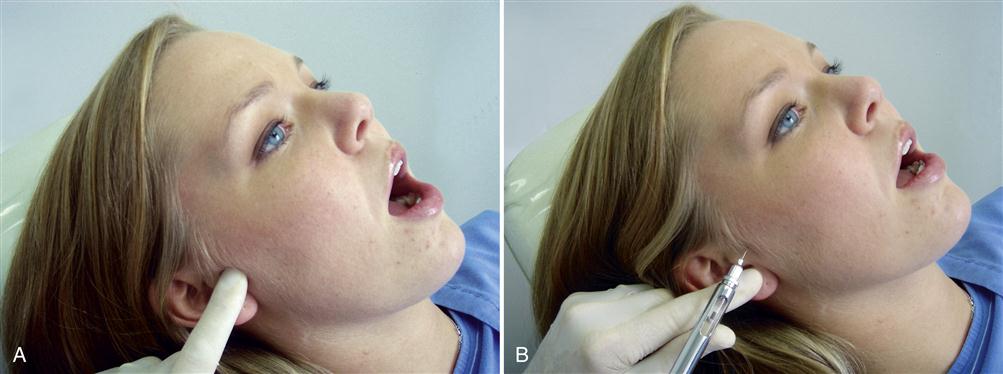
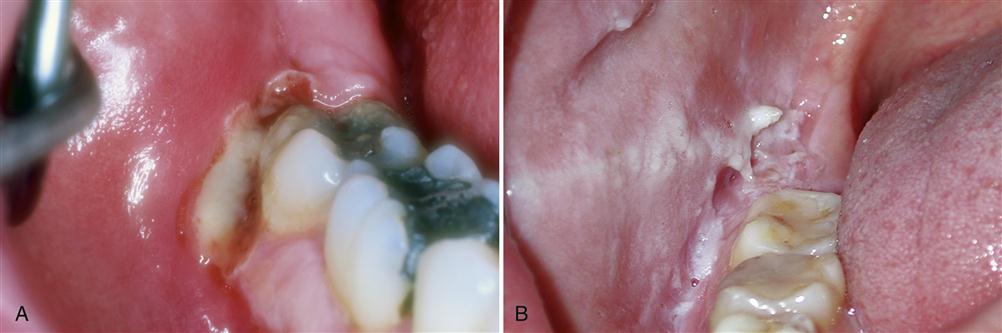
In attempting to locate the true source of pain, the clinician should palpate the area seen by the patient as the location of the pain. If this is the preauricular area, the clinician should palpate this area to see if pain is provoked. If this is a true source of pain, the pain will be increased with this palpation and/or by joint movement. If the pain is not increased, this area is not likely the source of pain but only a site (Figure 10-1, A). When this occurs, the clinician is obliged to continue to search for the source of pain in order to establish the proper diagnosis.
The next task is to explore the adjacent areas for sources of pain. In some instances the clinician may find a trigger point in the trapezius muscle that is painful and could be the source of the preauricular pain. Heterotopic pains can result from central excitatory effects in the brainstem produced by a distant source of nociception (Chapter 2). Palpation of this area will increase the pain not only in the trapezius but also in the preauricular area, to which it is referred (Figure 10-1, B). When this occurs, the clinician is verifying that the true source of pain felt in the TMJ is really not coming from the joint but that, in fact, the pain in the trapezius muscle is being referred to the preauricular area.
Sometimes it can be difficult to differentiate the site of pain from the source of pain. It may then be necessary to use selective local anesthetic blockade of tissues. This idea is based on the concept that local anesthetic blockade of a source of pain will temporarily eliminate the pain, since it blocks the nociceptive input originating from the true source of the pain. Following this concept, local anesthetic blockade of a site of pain will produce anesthesia in the area but have no effect on reducing the pain, since there is no nociceptive input coming from that site. Anesthetic blocking can be a very useful tool for the clinician treating orofacial pain disorders.
Continuing with the clinical case described above, the patient is complaining of TMJ area pain but the pain is not increased by palpation or joint movement. If an auriculotemporal nerve block were performed the TMJ area would become anesthetized (numb), but there would be no reduction in the pain (Figure 10-1, C). This is because the true source of the pain is not the TMJ but rather the trapezius muscle.
Once the source of pain is suspected to be in the trapezius muscle, this can be confirmed by locally anesthetizing the trigger point in this muscle. Once this is accomplished, the pain will resolve not only in the trapezius but also in the preauricular area (Figure 10-1, D). These diagnostic procedures are very important for the clinician since they are essential in establishing the correct diagnosis, the most critical aspect of successful pain management.
The manner in which secondary hyperalgesia (Chapter 2) clinically responds to local anesthetic blockade is somewhat different than is the case with referred pain. When the original source of pain is blocked, referred pain resolves immediately, but secondary hyperalgesia may remain for several hours. This probably occurs because of the nociceptive neurotransmitters that remain in the local tissues until they are metabolized (by neurogenic inflammation). Therefore the effect of a local anesthetic injection on secondary hyperalgesia should not be evaluated until the following day.
The following four rules summarize the examination techniques used to differentiate primary pain from referred pain. These rules are also graphically depicted in Figure 10-1, A-D:
Diagnostic Analgesic Blocking
Indications for Analgesic Blocking
The value of local anesthetic injections as well as the application of topical anesthetics to identify and localize pain cannot be overemphasized. It is essential in differentiating primary from secondary pains. It is equally useful to identify the pathways that mediate peripheral pain and to localize pain sources. Very often when the source of pain is difficult to identify, local anesthetic blocking of related tissues is the key to making the proper diagnosis. The examiner should therefore become skilled in the use of this valuable diagnostic tool. Muscle injections can also be useful for diagnostic purposes as well as for therapy. Local anesthetic blocking not only provides valuable diagnostic information but in some pain disorders can also provide therapeutic value. This is especially true for myofascial pain and myospasm.
Another indication for analgesic blocking is to help educate the patient as to the source of his or her pain problem. Often patients do not appreciate the concept of pain referral and it can be quite convincing to the patient when blocking a remote site reduces or even eliminates the chief complaint. This can be a very valuable educational tool.
The Armamentarium
The armamentarium needed to provided anesthetic blocks is already present in almost all dental offices. It begins with an aspirating syringe and both short and long 27-gauge needles. The length needed depends on the structure targeted. Alcohol and/or povidone-iodine (Betadine) swipes are also need to clean the site to be injected. Sterile 2-by-2 gauze pads should be available to apply to the injection site to control bleeding. Clean disposable gloves are also needed.
The type of local anesthetic used may vary according to the type and purpose of the particular injection. When only diagnostic information is needed, the use of a short-acting drug is most desirable. Usually a solution without a vasoconstricting agent is best. Good anesthesia for skeletal muscle requires a nonvasoconstricting solution owing to the vasodilating effect of epinephrine-like substances on such tissue. This reverse effect on muscle tissue is sometimes forgotten and may account for the poor-quality transient anesthesia that is sometimes obtained when muscles are injected for diagnostic purposes.
It has been demonstrated that local anesthetics have a measure of myotoxicity. Procaine appears to be the least myotoxic of the local anesthetics in common use.1 Mild inflammatory reactions follow the injection of 1% and 2% procaine hydrochloride as well as isotonic sodium chloride.2 Single injections of either procaine or isotonic saline cause no muscle necrosis.3 The longer-acting and stronger anesthetics induce more severe inflammation and occasional coagulation necrosis of muscle tissue.4 Regeneration takes place in about 7 days. Solutions containing epinephrine cause greater muscle damage.5 To minimize the danger of muscle damage in analgesic blocking for both diagnostic and therapeutic purposes, low concentrations of procaine are advisable, and such injections should be spaced at least 7 days apart. Since procaine is not available in dental carpules, the dentist may select 2% lidocaine (Xylocaine) or 3% mepivacaine (Carbocaine)6 without a vasoconstrictor. When a longer-acting anesthetic is indicated, 0.5% bupivacaine (Marcaine) may be used.7 Although bupivacaine is sometimes indicated for joint pain (auriculotemporal nerve block), it should not be routinely used with muscle injections because of its myotoxicity.8
The diagnostic use of local anesthetics in muscles should be limited to actual need. It should be noted that, despite some myotoxicity, the diagnostic and therapeutic use of local anesthesia in the management of myogenous pain disorders is clinically justified. Many diagnostic procedures and therapeutic modalities are attended by some risk, such as, for example, the destructive effects of radiation in radiography. All anesthetics and most medications are toxic to some degree. The inherent risks, therefore, must be weighed against the benefits derived. Reasonable judgment should be exercised in the application of all procedures that entail a measure of risk to the patient.
General Rules to Follow
Whenever an injection is to be performed, the following fundamental rules should be observed:
Types of Injections
Diagnostic and therapeutic anesthetic blocks are divided into three types according to the structures targeted: muscle injections, nerve block injections, and intracapsular injections. Each of these is discussed separately, since the indications and techniques vary.
Muscle injections
Injecting a muscle can be very valuable in determining the source of a pain disorder. In some instances muscle injections can provide therapeutic value. For example, the injection of local anesthetic into a myofascial trigger point can result in significant pain reduction long after the anesthetic has been metabolized.9–14 In myofascial pain, the patient presents with a firm taut band of muscle tissue that is quite painful to palpate. This is known as a trigger point and is often responsible for producing a pattern of pain referral9 (Chapter 8). When this is suspected, the trigger point can be injected with local anesthetic; thus the resulting pattern of pain referral is shut down. The precise mechanisms of trigger-point pain and the indications for treatment are reviewed in Chapter 12. When it has been determined that injection of the trigger point is indicated, the following sequence should be followed:
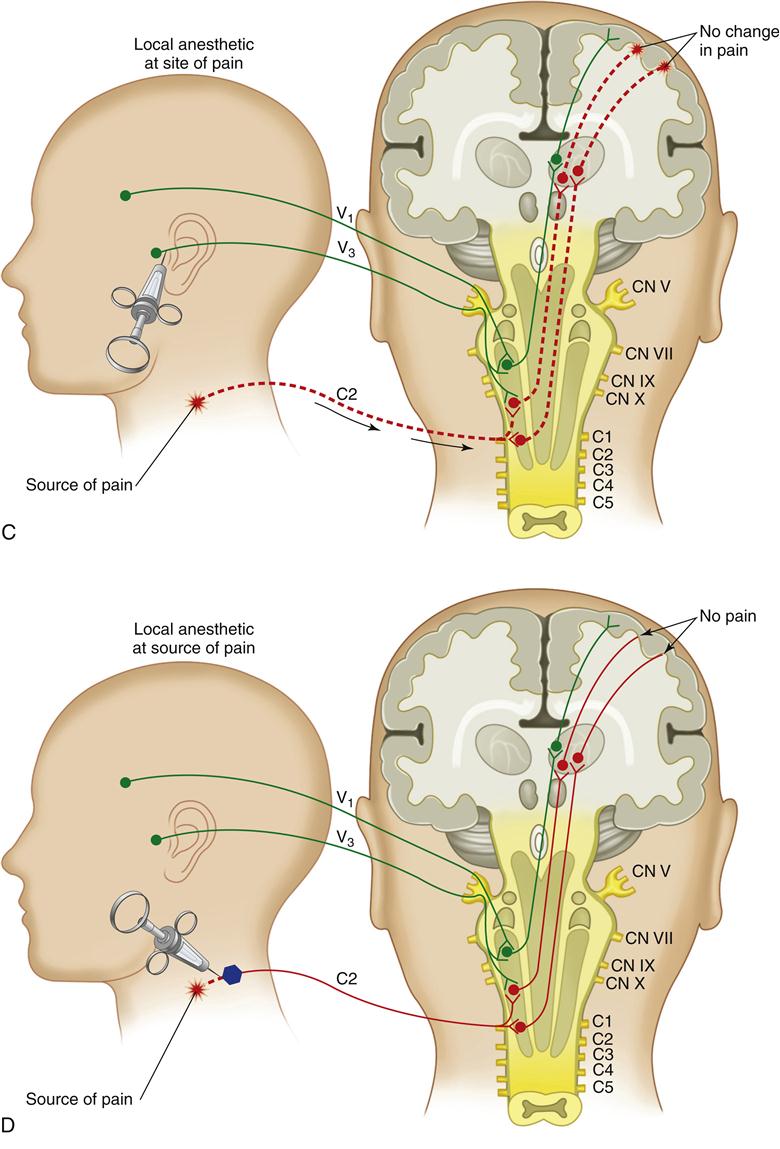
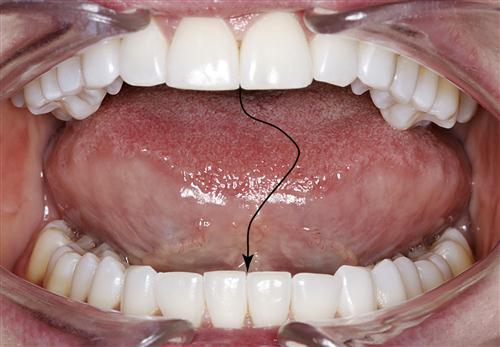
1. The trigger point is located by placing the finger over the muscle and firm pressure is applied to locate the tight band. The finger is moved across the band so that it can be felt to “snap” under the pressure of the finger. Once the band has been identified, the finger is moved up and down the band until the most painful area is located (Figure 10-2, A).
2. Once the trigger point is located, the tissue over the trigger point is cleaned with alcohol. The trigger point is then trapped between two fingers so that when the needle is placed into the area, the tight band will not move away (Figure 10-2, B).
3. The needle tip is then inserted into the tissue superficial to the trigger point and advanced to the depth of the tight band (Figure 10-2, C). It is often helpful to receive feedback from the patient regarding the accuracy of the needle placement. Usually the patient can tell immediately when the trigger point has been entered. Once the needle tip is at the proper depth, the syringe is aspirated to make sure that it is not located in a vessel. Then a small amount of anesthetic is deposited in the area (one quarter of a carpule).
4. Once the initial anesthetic has been deposited, it is useful to “fan” the needle tip slightly. This is done by withdrawing the needle halfway, changing the needle’s direction slightly, and reentering the firm band to the same depth (Figure 10-2, D). The needle tip should not be completely removed from the tissue. This manipulation of the needle tip should be repeated several times, especially if the patient has not confirmed that the needle tip has reached the area of exquisite tenderness. At each site the syringe is aspirated and a small amount of anesthetic is deposited. In some instances, the muscle will be felt to contract quickly. This is known as the twitch response and usually helps confirm that the needle is properly placed.15 Although the presence of a twitch response is favorable, not all muscles demonstrate this, and successful pain reduction can often be achieved without it.
5. Once the injection has been completed, the needle is fully withdrawn and a sterile gauze is held over the injection site with slight pressure for 5 to 10 s to assure good hemostasis (Figure 10-2, E).
This general technique is used for most muscle injections; however the unique anatomy of each muscle may demand slight variations. It is extremely important that the clinician be familiar with the anatomy of the muscle to be injected so as to avoid disturbing any neighboring structures. A review of the anatomy of all the muscles that may require injection is beyond the scope of this text; it is therefore recommended that the clinician consult appropriate texts on gross anatomy before proceeding with an injection. Muscles that can be injected easily are the masseter (Figure 10-3), temporalis (Figure 10-4), sternocleidomastoid (Figure 10-5), splenius capitis (Figure 10-6), posterior occipital muscles (Figure 10-7), and trapezius muscle (Figure 10-8). The orofacial pain specialist should become familiar with the anatomic features of these muscles and surrounding structures so that safe and predictable injections can be routinely preformed.



Nerve block injections
Diagnostic nerve blocks can be very useful in identifying whether a painful structure is actually a site or source of pain. When diagnosis is the primary purpose of the injection, a short-acting local anesthetic should be used without a vasoconstrictor. In some instances long-term pain relief maybe therapeutically indicated. This may be appropriate for certain chronic pain conditions when prolonged relief of pain can be used to interrupt pain cycling and hopefully reduce central sensitization. When long-term anesthesia is indicated, a long-term local anesthetic, such a bupivacaine with a vasoconstrictor, may be a better choice.
Some of the important nerve blocks that should be considered are dental blocks, the auriculotemporal nerve block, and the infraorbital nerve block.
Dental blocks
The practicing dentist uses nerve blocks routinely in dental treatments. It should be remembered that these same injections can provide valuable diagnostic information. The common nerve blocks used are the inferior alveolar nerve block, the posterior superior nerve block, the mental nerve block, and infiltration blocks often administered in various areas of the maxillary arch. The techniques used for these blocks are not reviewed here since they are routinely used in the dental office. Although these blocks are mostly used for anesthesia during dental procedures, their diagnostic value should not be overlooked. For example, an inferior alveolar nerve block will completely eliminate any source of pain coming from the mandibular teeth on the side of the injection. This block is useful in separating dental pain from muscle or joint pain since it blocks only the dental structures. This is very important diagnostic information, especially when a patient’s chief complaint is toothache. If a mandibular toothache is truly of dental origin, an inferior alveolar nerve block will eliminate the pain. If, however, the toothache is actually a referred pain, the block will not change the pain.
In attempting to localize a particular tooth as a source of pain, it is important to consider local infiltration of the anesthetic first before a total nerve block (i.e., mandibular block) is undertaken. Isolating a single tooth with local anesthetic is far more specific than blocking an entire quadrant of teeth. Once the entire nerve has been blocked, it may be very difficult to identify the specific tooth until the anesthesia has been metabolized. As a general rule for diagnosing tooth pain, it is best to begin by utilizing very localized areas of anesthesia and then moving to broader areas as needed. Starting with a total nerve block can be confusing, especially if one tooth is referring to another and both are blocked at the same time.
In identifying pain sources, it is important that the clinician ask the patient the proper questions. If the patient has a nonodontogenic toothache and an inferior alveolar nerve block is administered, the pain will not be resolved even though the tissues become anesthetized. If the clinician asks whether the area is numb, the patient will respond positively. This may lead the clinician to assume that the pain has resolved, which is not the case. After giving the patient local anesthesia, the clinician must phrase the question carefully. The clinician should ask the question in this manner: “Now I realize that your jaw is numb, but does it still hurt?” The patient’s jaw will certainly feel numb, but the important question is “Does it still hurt?” This is a critical concept to appreciate in differentiating the odontogenic toothache from the nonodontogenic toothache.
Auriculotemporal nerve block
A very important nerve block with which all orofacial pain clinicians should become very familiar is the auriculotemporal nerve block. This nerve block has very significant diagnostic value. The primary innervation of the TMJ is from the auriculotemporal nerve, with secondary innervation coming from the masseter and posterior deep temporal nerves.16 Therefore if the TMJ is a source of pain, this nerve block will quickly eliminate the pain. Since the TMJ area is a frequent site of pain referral, this block is very valuable and indicated to help determine when the joint is actually a source of pain. In fact, anytime that an irreversible treatment is planned for the TMJ, such as surgery, this block can help to confirm the need for such treatment. If an auriculotemporal nerve block does not resolve the pain, aggressive therapies should not be considered until the true source of the pain is identified.
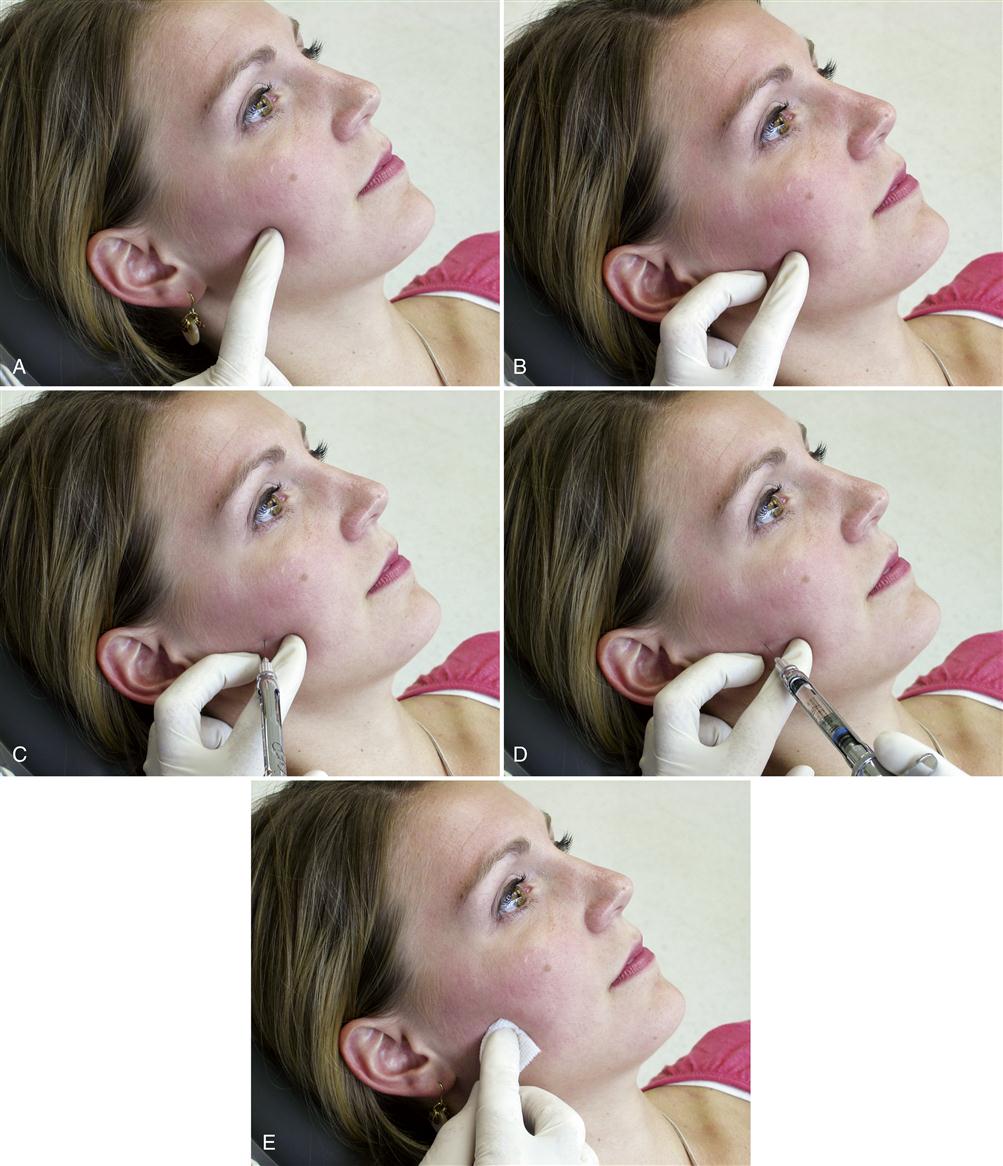
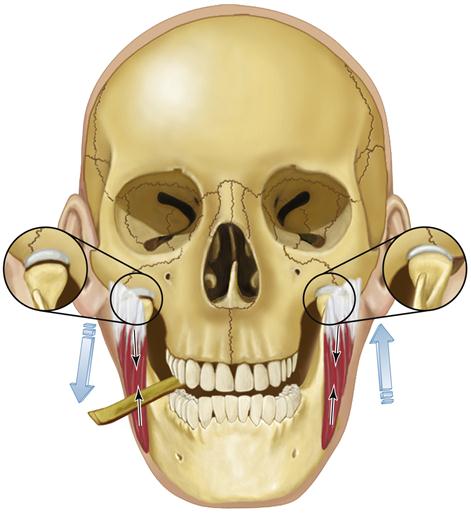
Some clinicians anesthetize the TMJ by injecting directly into the joint or into the retrodiscal structures. Although this may be effective, it can also traumatize delicate joint structures. A less traumatic method is to anesthetize the joint structures by blocking the auriculotemporal nerve before its fibers reach the joint. The auriculotemporal nerve can be blocked by first cleaning the tissue (Figure 10-9, A) and then passing a 27-gauge needle through the skin just anterior and slightly above the junction of the tragus and the earlobe (Figure 10-9, C). The needle is then advanced until it touches the posterior neck of the condyle. The needle is then repositioned in a more posterior direction until its tip is able to pass behind the posterior neck of the condyle (Figure 10-9, D). Once the neck of the condyle is felt, the tip of the needle is carefully moved slightly behind the posterior aspect of the condyle in an anteromedial direction to a depth of 1 cm (Figure 10-9, E). The syringe is then aspirated and, if no blood is seen, the solution is deposited.17 If the true source of pain is the joint, the pain should be eliminated or certainly significantly decreased in 4 to 5 min.
Intracapsular injections
On occasion it is indicated to inject directly into the temporomandibular joint (TMJ). This type of injection would be indicated for therapeutic and not diagnostic reasons. Diagnostic information is derived from performing the auriculotemporal nerve block. A therapeutic injection would be indicated when it is appropriate to introduce some medication to the joint structures. The types of medications that may be considered are discussed in Chapter 11.
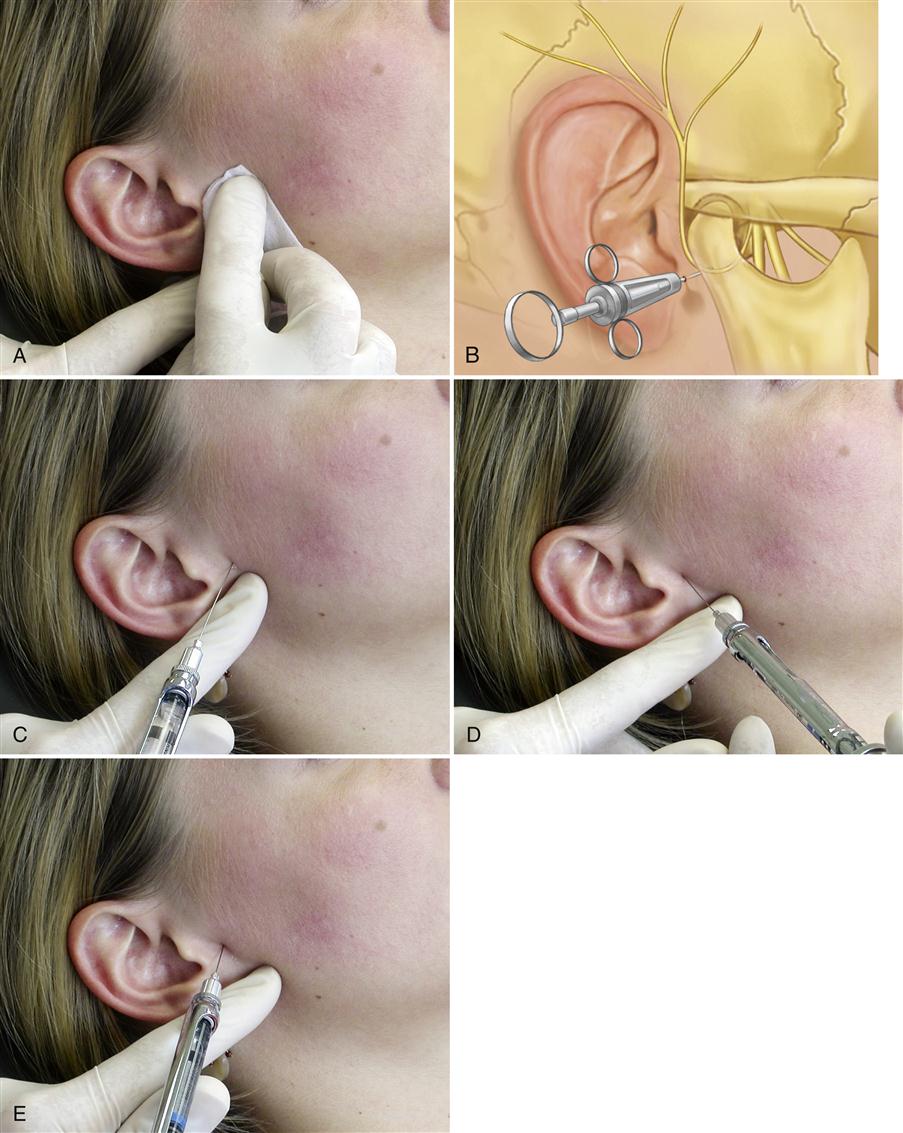
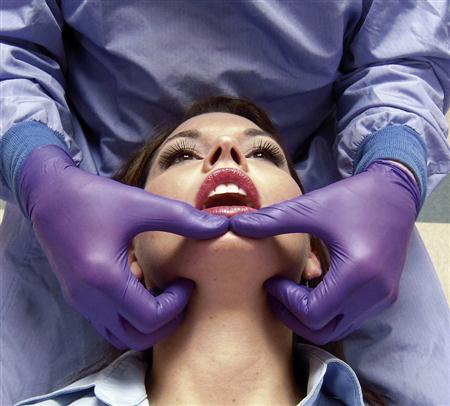
Normally the superior joint space is the target for an intracapsular (intra-articular) injection because it is the largest joint space and is the simplest to locate consistently. The joint can be entered by first locating the lateral pole of the condyle. This can be assisted by asking the patient to open and close the mouth (Figure 10-10, A). Once the pole is located, the patient is asked to open slightly and the clinician palpates directly above to locate the zygomatic arch. The tissue is cleaned and the tip of the needle is placed just below the zygomatic arch and slightly behind the posterior and superior aspect of the condyle. The needle is angulated slightly anterosuperiorly to avoid the retrodiscal tissues and ear structures (Figure 10-10, B). Once the capsule is penetrated, the tip of the needle will be in the superior joint space. The solution is then deposited and the needle removed. A sterile gauze is held over the injection site for a few seconds to ensure hemostasis. The patient is then asked to open and close the mouth a few times to distribute the solution throughout the joint space.
Often a successful intra-articular injection will leave the patient with an immediate acute malocclusion on the ipsilateral side. Since there is very little area in the superior joint space, the introduction of additional fluid will temporarily cause an increase in the joint space, which leads to the separation of the posterior teeth on the same side of the injection. This will resolve in a few hours. The patient should be made aware of this condition so that it does not lead to any unnecessary concern or emotional stress.
Infraorbital nerve block
The infraorbital nerve traverses below the eye to exit from the infraorbital foramen located in the inferior border of the orbit. This nerve goes on to innervate the facial structures below the eye and some of the lateral aspects of the nose. In cases of trauma to the face, this nerve can be injured resulting in a continuous neuropathic pain. Blockage of this nerve may have some therapeutic value. The nerve can be blocked by either an extra- or intraoral approach. When the extraoral approached is used, the foramen is identified by palpation of the inferior border of the orbit, feeling for a slight notch. The notch represents the exit of the infraorbital nerve. Once the notch is located, the tissue is cleaned and the needle is placed to the depth of the notch and into the foramen when possible (Figure 10-11, A). When the intraoral approach is used, the notch is found in the same manner as previously described. The middle finger is used to maintain the position of the notch while the index finger and thumb are used to retract the lip. The needle is placed into the mouth and the tip is inserted into the vestibule and directed upward to the notch (Figure 10-11, B). In some instances a long 27-gauge needle may be needed to reach the foramen with this technique.
Keys to Making a Differential Diagnosis
As stated in previous chapters, the two most common masticatory problems (other than odontalgia) that present in a dental office are masticatory muscle disorders and intracapsular joint disorders. It is extremely important that they be differentiated, since their treatments are quite different. The clinician who cannot routinely separate them is likely to have relatively poor success in managing TMDs.
Although muscle and joint disorders have some clinical findings in common, there are seven areas of information acquired during the history and examination that will assist in separating them. These keys to diagnosis are the following: history, mandibular restriction, mandibular interference, acute malocclusion, loading of the joint, functional manipulation, and diagnostic anesthetic blockade.
1. History. The history is always helpful in distinguishing joint from muscle disorders.18,19 In the patient’s report, one must listen for an event that might have initiated the disorder. When a joint is traumatized, the symptoms are likely to begin in association with the trauma and to be relatively constant or to worsen from that time forward. Muscle disorders, on the other hand, appear to fluctuate and cycle from severe to mild with no apparent initiating event. Muscle problems are more closely related to changes in levels of emotional stress; therefore periods of total remission are not uncommon when stress is low.
2. Mandibular restriction. Restriction of mouth opening and eccentric movements are common findings with both joint and muscle disorders. The character of the restrictions, however, can be quite different. Restriction in mouth opening because of intracapsular problems (e.g., a dislocated disc without reduction) usually occurs at 25 to 30 mm. At that point the mouth cannot be opened wider, even with mild passive force. This hard “end feel”’ is commonly associated with a dislocated disc blocking translation of the condyle. Restricted mouth opening as a result of a muscle disorder can occur anywhere during the opening movement. For example, a restricted opening of 8 to 10 mm is most certainly of muscle origin. When the mouth opening is restricted by muscles, mild passive force will usually lengthen the muscles slightly and result in a small increase in opening. This represents a soft end feel and is typical of muscle restriction. Combining these clinical findings with the onset of the limited mouth opening obtained in the history is very helpful in understanding the reason for the restriction.
Mandibular restriction should also be evaluated by observing the patient move in left and right eccentric positions. In patients with an intracapsular restriction (i.e., disc dislocation without reduction), a contralateral eccentric movement will be limited but an ipsilateral movement will be normal. However, with muscle disorders, the elevators (temporalis, masseter, medial pterygoid) are responsible for the limited mouth opening and, because eccentric movements do not generally lengthen these muscles, a normal range of eccentric movement exists.
3. Mandibular interference. When the mouth is opened, the pathway of the mandible is observed for any deviations or deflections. If the deviation occurs during opening and the jaw then returns to midline before 30 to 35 mm of total opening, it is likely to be associated with a disc derangement disorder (Figure 10-12). If the speed of opening alters the location of the deviation, it is likely to be associated with discal movement, such as disc displacement with reduction. If the speed of opening does not alter the interincisal distance of the deviation and the location of the deviation is the same for opening and closing, a structural incompatibility is a likely diagnosis. Muscle disorders that cause deviation of mandibular opening pathways are commonly large, inconsistent, sweeping movements not associated with joint sounds. These deviations result from muscle engrams. Deviation can also occur because of subluxation at the wide-open position. This is an intracapsular disorder but not necessarily a pathologic condition.
Deflection of the mandibular opening pathway results when one condyle does not translate (Figure 10-13). This may be due to an intracapsular problem such as a disc dislocation without reduction or an adhesion problem. With these problems, the mandible will deflect to the ipsilateral side during the late stages of opening. Deflection during opening can also result if a unilateral elevator muscle, such as the masseter, becomes shortened (myospasm). This condition can be separated from intracapsular disorders by observing the protrusive and lateral eccentric movements. If the problem is intracapsular, the mandible will often deflect to the side of the involved joint during protrusion and be restricted during a contralateral movement (normal movement to the ipsilateral side). If the problem is extracapsular (i.e., stemming from muscle), there will be no deflection during the protrusive movement and no restrictions in lateral movements.
When deflection of the mandible is due to an intracapsular source, the mandible will move toward the involved joint. If the deflection is the result of a shortened muscle, the direction in which the mandible moves will depend on the position of the involved muscle with respect to the joint. If the muscle (i.e., masseter or temporalis) is lateral to the joint, the deflection will be toward the involved muscle. If the muscle (i.e., medial pterygoid) is medial to the joint, deflection will be away from the involved muscle (in a contralateral direction).
4. Acute malocclusion. As stated earlier, an acute malocclusion is a sudden alteration of the occlusal condition secondary to a disorder. An acute malocclusion caused by a muscle disorder will vary according to the muscles involved. If the inferior lateral pterygoid is in spasm and shortens, the condyle will be brought slightly forward in the fossa on the involved side. This will result in a disocclusion of the ipsilateral posterior teeth and heavy contact on the contralateral canines (Figure 10-14). If the spasms are in the elevator muscles, the patient is likely to report a feeling that the teeth “suddenly don’t fit right,” yet clinically it may be difficult to visualize any change. An acute malocclusion resulting from an intracapsular disorder is usually very closely related to the event that changed the joint function. If the disc is suddenly displaced, the thicker posterior border may be superimposed between the condyle and fossa and cause a sudden increase in the discal space. This appears clinically as a loss of ipsilateral posterior tooth contact. If the disc becomes suddenly dislocated, collapse of the discal space can occur as the condyle compresses the retrodiscal tissues. The patient notes this as a sudden change in the occlusion characterized as heavy posterior contact on the ipsilateral side. If this condition continues, retrodiscitis may result and cause tissue inflammation with swelling of the retrodiscal tissues. The resulting acute malocclusion may now change to one characterized by loss of posterior tooth contacts on the ipsilateral side.
5. Loading the joint. As mentioned in Chapter 9, positioning the condyles to their musculoskeletally stable position and loading the structures with manipulative force does not produce pain in a healthy joint. When pain is produced, one should be suspicious of an intracapsular source of pain (Figure 10-15).
6. Functional manipulation. As stated in Chapter 9, functional manipulation can be helpful in identifying the location of pain. Functional manipulation procedures that do not produce pain tend to rule out muscle disorders as the source of the problem.
If the clinician wants to differentiate intracapsular pain from muscle pain, having the patient bite on a tongue blade can be helpful. When a patient bites unilaterally on a hard substance, the interarticular pressure is quickly reduced in the ipsilateral TMJ (Figure 10-16). If the patient’s primary source of pain is the TMJ structures, this will reduce the pain. Conversely, if the patient bites on the contralateral side, the interarticular pressure on the opposite joint will be increased. Therefore this activity increases the preauricular pain. For example, if a patient has right-side TMJ pain (e.g., osteoarthritis), the right TMJ will be painful when the patient clenches the teeth. If a tongue blade is placed between the right-side molars and the patient is again asked to bite on the tongue blade, the right-side TMJ pain will be reduced or eliminated (Figure 10-17). This is due to reduced loading of the painful structures. If, however, the tongue blade is moved to the left molar area and the patient is asked to bite, the increased loading of the right TMJ will result in increased pain in the right preauricular area.
If the patient has primary muscle pain (e.g., right-side masseter pain), when he or she is asked to clench the teeth, the right masseter will produce pain. If a tongue blade is placed on the right molar and the patient is asked to bite on it, pain will also be increased. This is due to the increase activity of the painful masseter muscle. If, however, the tongue blade is moved to the left side and the patient is asked to bite on it, there will be a reduction in pain on the right. This occurs because the predominant muscle activity now comes from the left masseter muscle.
Biting on a unilateral tongue blade is a simple procedure that can be very helpful in differentiating muscle pain disorders from intracapsular pain disorders. As stated earlier, it is essential to differentiate these disorders in order to determine the most appropriate treatment.
Classification of Temporomandibular Disorders
For years the classification of TMDs has been a confusing issue. There have been almost as many classifications as there were texts on the subject. Then Welden Bell20 presented a classification that logically categorizes these disorders and the American Dental Association21 adopted it with few changes. It has, in fact, become a “road map” helping clinicians toward a precise and well-defined diagnosis.
This chapter presents the basic classification of TMDs developed by Bell but incorporates some additional modifications of my own. The American Academy of Orofacial Pain has also followed a similar classification for the last two editions of its guidelines.22,23 It begins by separating all TMDs into four broad categories having similar clinical characteristics: masticatory muscle disorders, TMDs, chronic mandibular hypomobility disorders, and growth disorders. Each of these categories is further divided according to dissimilarities that are clinically identifiable. The result is a relatively intricate classification system that initially might appear to be almost too complex. However, this classification is important, since treatment indicated for each subcategory varies greatly. In fact, treatment that is indicated for one may be contraindicated for another. It is therefore important that these subcategories be identified and clearly defined so that the proper treatment can be initiated.
Treatment failures are commonly attributed to the utilization of one mode for all patients in a major category. This, however, demonstrates improper diagnostic technique and almost always leads to treatment failure. It is virtually impossible to overemphasize the importance of proper diagnosis as the key to successful treatment. Dentistry is indebted to Dr. Bell for his major contribution to the diagnostic classification of TMDs.
Each broad category can be described according to the symptoms that are common to it while each subdivision is characterized by the clinical characteristics that differentiate it from the others. In this chapter each disorder is discussed according to the etiology, history, and examination findings leading to its diagnosis. Once a diagnosis has been established, appropriate treatment must be provided. Treatment for each disorder is discussed in Chapters 11 to 16. The classification used for diagnosing TMDs is summarized in Box 10-1.
Masticatory Muscle Disorders
Certainly the most frequent complaint of patients with functional disturbances of the masticatory system is muscle pain (myalgia). Patients commonly report that the pain is associated with functional activities such as chewing, swallowing, and speaking. The pain is also aggravated by manual palpation or functional manipulation of the muscles. Restricted mandibular movement is common. Muscle pain is of extracapsular origin and may be primarily induced by the inhibitory effects of deep pain input. The restriction is most often not related to any structural change in the muscle itself. Sometimes accompanying these muscle symptoms is an acute malocclusion. Typically the patient will report that his or her bite has changed. As previously stated, muscle pain disorders can so alter the resting mandibular position that when the teeth are brought into contact, the patient perceives a change in the occlusion.
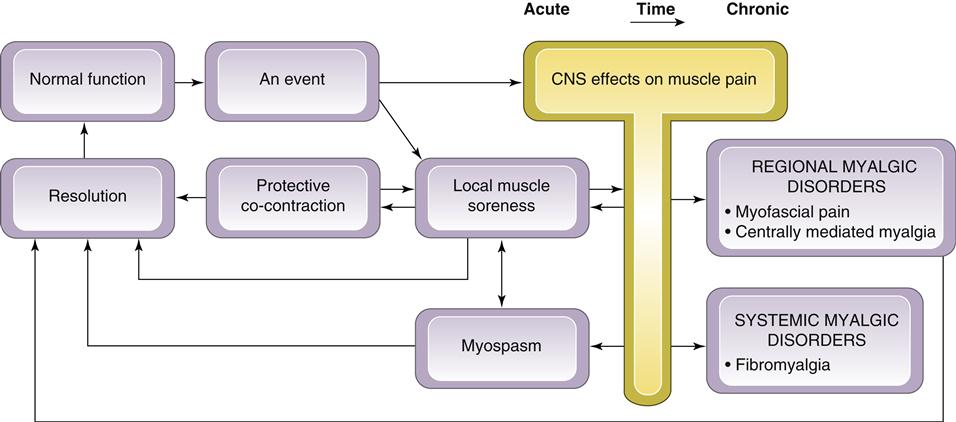
All masticatory muscle disorders are not clinically the same. At least five different types are known; being able to distinguish among them is important because the treatment of each is quite different. The five types are protective co-contraction (muscle splinting), local muscle soreness, myofascial (trigger point) pain, myospasm, and centrally mediated myalgia. A sixth condition known as fibromyalgia must also be discussed. The first three conditions (protective co-contraction, local muscle soreness, and myofascial pain) are commonly seen in the dental office. Myospasm and centrally mediated myalgia are less frequently seen. Since most of these masticatory muscle disorders occur and recover in a relatively short period of time, they are generally considered acute myalgic disorders. When these conditions are not resolved, more chronic pain disorders may result, which are often more complicated to manage. Centrally mediated myalgia and fibromyalgia are examples of chronic myalgic disorders. In some patients myofascial pain can also become chronic. Chronic myofascial pain and centrally mediated myalgia are regional pain disorders, whereas fibromyalgia is a chronic systemic myalgic disorder. Fibromyalgia is not primarily a masticatory problem; therefore the dentist must be able to recognize it for referral to the appropriate medical personnel.
In Chapter 8 a masticatory muscle model was described showing the relationship between the acute myalgic disorders and certain events that are experienced by the masticatory system. This model also depicts how a nonresolving acute myalgic disorder can become chronic when certain perpetuating conditions are present (Figure 10-18). Here that model is not reviewed; instead, the following discussion concentrates on a detailed description of each disorder so that a proper diagnosis can be established. For review of the model, the reader is referred to Chapter 8.
Protective co-contraction (muscle splinting)
The first response of the masticatory muscles to one of the previously described events is protective co-contraction. This is a central nervous system (CNS) response to injury or threat of injury. In the past this response was referred to as muscle splinting.20 In the presence of an event, the activity of appropriate muscles seem to be altered so as to protect the injured part from further injury.24–28 As has already been described (Chapter 2), all muscles are maintained in a mildly contracted state known as tonus. Tonus persists without fatigue by virtue of the alternating contractions and relaxations of the muscle fibers, which keep the overall muscle length unchanged and resist any sudden elongation.
When protective co-contraction occurs, the CNS increases the activity of the antagonist muscle during contraction of the agonist muscle. It is important to recognize that co-contraction29 is observed during many normal functional activities such as bracing the arm in attempting a task with the fingers. In the presence of altered sensory input or pain, however, antagonistic muscle groups seem to fire during movement in an attempt to protect the injured part. In the masticatory system, for example, a patient who is experiencing protective co-contraction will demonstrate slightly increased muscle activity in the elevator muscles during mouth opening.26,30 During closing of the mouth, an increase in activity is noted in the depressing muscles. This reflexlike activity is not a pathologic condition but a normal protective or guarding mechanism that must be identified and appreciated by the clinician. It is important to recognize that this increase in muscle activity is very slight and therefore not clinically identifiable with electromyography (EMG) except under stringent experimental conditions. Such increased EMG activity is much less than the clinical error encountered from patient variability as well as from variability in electrode placement (Chapter 9).
Etiology
Three conditions can lead to protective co-contraction:
2. Constant deep pain input. As already discussed, the presence of deep pain input felt in local structures can produce protective co-contraction of associated muscles (Figure 10-19). This phenomenon occurs by way of the central excitatory effects described in Chapter 2. It is important to note that the source of the deep pain need not be muscle tissue itself but any associated structures such as tendons, ligaments, joints, or even the teeth.
3. Increased emotional stress. Clinical observations strongly demonstrate that emotional stress can greatly influence masticatory muscle activity31–35 (Chapter 7). When an individual experiences increased levels of emotional stress, a common response is for the gamma efferent system to alter the sensitivity of the muscle spindle. This increases the sensitivity of the muscle to lengthening, resulting in increased tonicity of the muscle. The clinical response of the muscle is seen as protective co-contraction. Increased emotional stress also has the ability to initiate parafunctional activities such as nocturnal bruxism and clenching. As previously discussed, these activities can lead to muscle symptoms.
History
The history reported by the patient reveals a recent event associated with one of the etiologies discussed above. The patient may report an increase in emotional stress or the presence of a source of deep pain. The key to the history is that the event occurred very recently, usually within a day or two.
Clinical characteristics
Myalgia, although often present, is not usually the major complaint associated with protective co-contraction. The following four clinical characteristics identify this clinical condition:
2. No pain at rest. Individuals who experience protective co-contraction have little to no pain when the muscle is allowed to rest. Co-contraction may represent a very slight increase in tonicity of the muscle; but an increase in tonicity, especially for a short period of time, does not produce myalgia. As already mentioned, it is unlikely that this slight increase in activity would be measurable by EMG output, especially considering the great variability of resting activity between patients.36–39
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses