Chapter 1
Oral Structures and Tissues
Arthur R. Hand1 and Marion E. Frank2
1 Department of Craniofacial Sciences and Cell Biology, School of Dental Medicine, University of Connecticut
2 Department of Oral Health and Diagnostic Sciences, University of Connecticut
The oral cavity and its component cells, tissues, and structures constitute a unique and complex organ system and environment. Of necessity, we study its various parts individually, but the health and function of the components of the oral cavity depend upon and influence one another. Importantly, the oral cavity relies on as well as influences the health and function of the entire body.
The oral cavity is the gateway to the body, and most of the substances that enter our bodies do so through the oral cavity. It is exposed to the physical insults of mastication, hard objects and various food substances, and extremes of temperature. A variety of chemicals, including those present in foods and drinks and produced by commensal and pathogenic organisms, affect the oral cavity. It functions in alimentation, respiration, innate and immune defense, special and general sensation, speech, and human interactions. The tissues and structures of the oral cavity are subject to unique as well as general disease processes. Diseases originating in the oral cavity can have systemic effects; likewise, systemic diseases can affect the oral cavity and the first signs and symptoms of many diseases may appear in the mouth.
The oral cavity
The readily visible components of the oral cavity include the lips (labia), the inside of the cheeks (bucca), the teeth and gums (gingivae), the hard and soft palates, the floor of the mouth, and the tongue (Fig. 1.1). Not visible, but clearly important, are the muscles, nerves, blood vessels, glands, joints, and especially the bones of the upper (maxilla) and lower (mandible) jaws that provide support for and function with the visible components. The oral cavity begins at the junction of the vermilion border of the lips and the mucosa lining the inside of the lips, and extends posteriorly to the palatoglossal folds or arch. Beyond the palatoglossal folds are the palatopharyngeal folds and the beginning of the oropharynx, where the digestive and respiratory tracts come together. The palatine tonsils are located in the tonsillar fauces between the palatoglossal and palatopharyngeal folds. The lymphoid tissue of the palatine tonsils, along with that of the pharyngeal tonsil (adenoids) and the lingual tonsils, guards the entrance to the oropharynx. Anteriorly, the respiratory tract (nasal cavity) is separated from the oral cavity by the hard palate, and posteriorly by the soft palate. The hard palate has an arch-like shape that varies in width and height among individuals. It also plays an important role in manipulation and mastication of food, and in speech. The soft palate functions to seal the oropharynx from the nasopharynx during swallowing and speech. However, during exhalation, receptor cells that detect odors in the olfactory mucosa are activated by oral vapors moving from the posterior oral to posterior nasal cavity through the nasopharynx, effectively expanding the mouth. It is this retronasal route that gives food and drink the odors that contribute much to flavor perception.
Figure 1.1 Diagram illustrating the anatomy and main structures of the oral cavity.
(Modified from Tortora, G.J. & Grabowski, S.R. 2000. Principles of Anatomy and Physiology, 9th edition, Wiley, New York. Reproduced by permission of John Wiley & Sons.)
The lips and cheeks are separated from the alveolar processes of the maxilla and mandible that support and hold the teeth by a space called the vestibule. The vestibule is limited posteriorly by the ramus of the mandible, and superiorly and inferiorly by the mucolabial and mucobuccal folds. The mucosal lining of the vestibule is continuous with the mucosa of the lips and cheeks, and with the mucosa covering the alveolar processes (Fig. 1.2). Folds (frena [singular, frenum]) of the mucosa, located at the midline and in the canine regions, extend across the vestibule to anchor the lips and cheek to the maxilla and mandible. The secretions of the parotid salivary gland enter the vestibule through its main duct, which opens at the parotid papilla on the buccal mucosa opposite the maxillary second molar tooth.
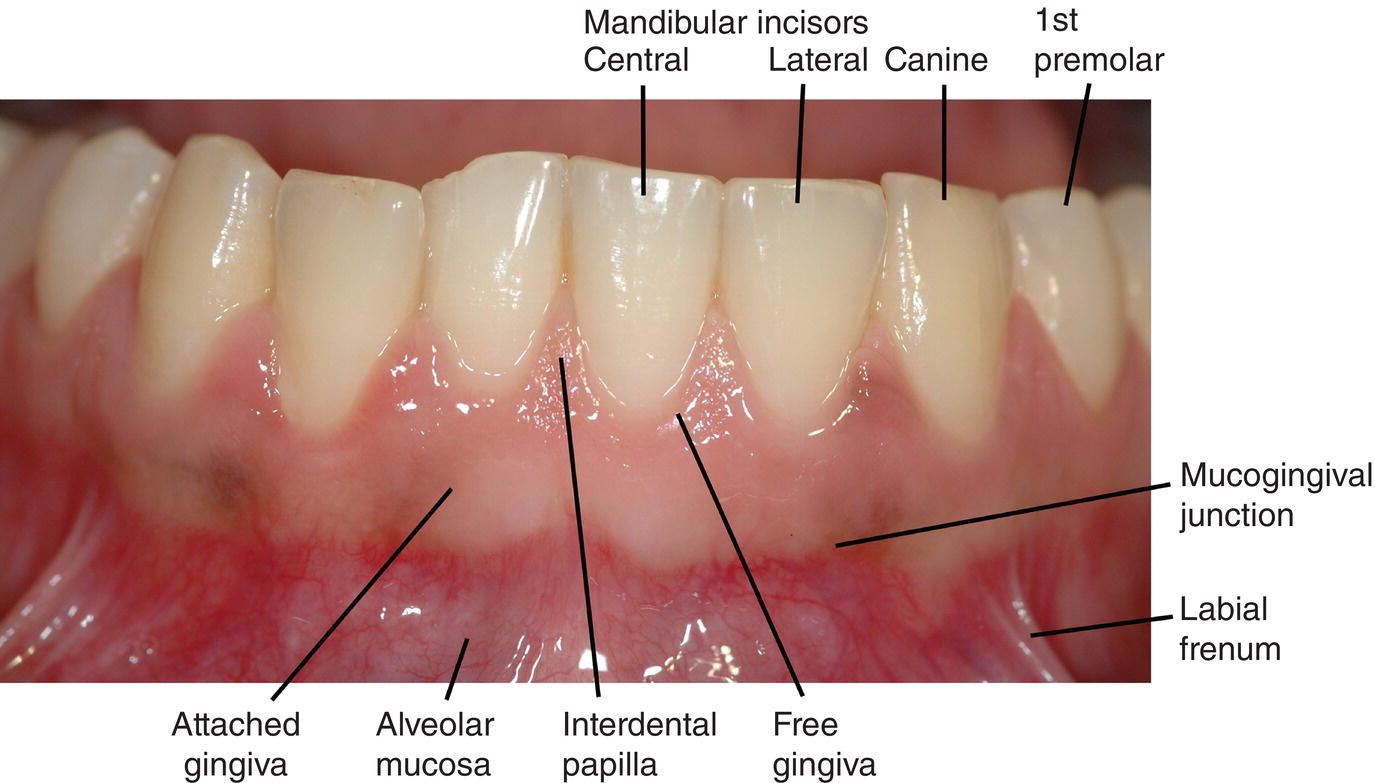
Figure 1.2 Oral mucosa, gingivae and mandibular teeth. Blood vessels visible through the thin non-keratinized epithelium of the alveolar mucosa give it a redder color than the gingivae with their thicker keratinized epithelium.
The mucosa surrounding the necks, or cervical regions of the teeth, is called the gingivae. The attached gingiva is clearly demarcated from the alveolar mucosa at the mucogingival junction. The attached gingiva is firmly bound to the bone of the alveolar process, and through the junctional epithelium is bound to and creates a seal around each tooth. The free gingiva is separated from the tooth by the gingival sulcus or crevice, and forms the interdental papilla between adjacent teeth.
The tongue occupies the space within the maxillary and mandibular arches, from the floor of the mouth to the hard and soft palates. The mucosa of the dorsal surface of the tongue has several types of specialized structures called papillae that function in the manipulation of food and in taste. The tongue also is critical for forming proper speech sounds. The anterior portion of the tongue is anchored to the floor of the mouth by the lingual frenum. The ducts of the submandibular and sublingual salivary glands open on either side of the lingual frenum at the sublingual caruncle; smaller ducts of the sublingual gland open along the sublingual fold on each side of the floor of the mouth.
Oral mucosa
Mucosa is a wet, soft tissue membrane that lines an internal body space, e.g., the oral cavity, the gastrointestinal, urinary, and reproductive tracts. The oral mucosa consists of three layers: a surface epithelium; a supporting lamina propria consisting of a layer of loose connective tissue (papillary layer) just below the epithelium and a deeper layer of dense irregular connective tissue (reticular layer); and an underlying submucosa consisting of dense irregular connective tissue (Fig. 1.3). The submucosa frequently contains minor salivary glands, and in some locations may contain adipose tissue. In some regions of the oral cavity, the submucosa may be absent, and the mucosa is bound to either bone or muscle by the lamina propria.
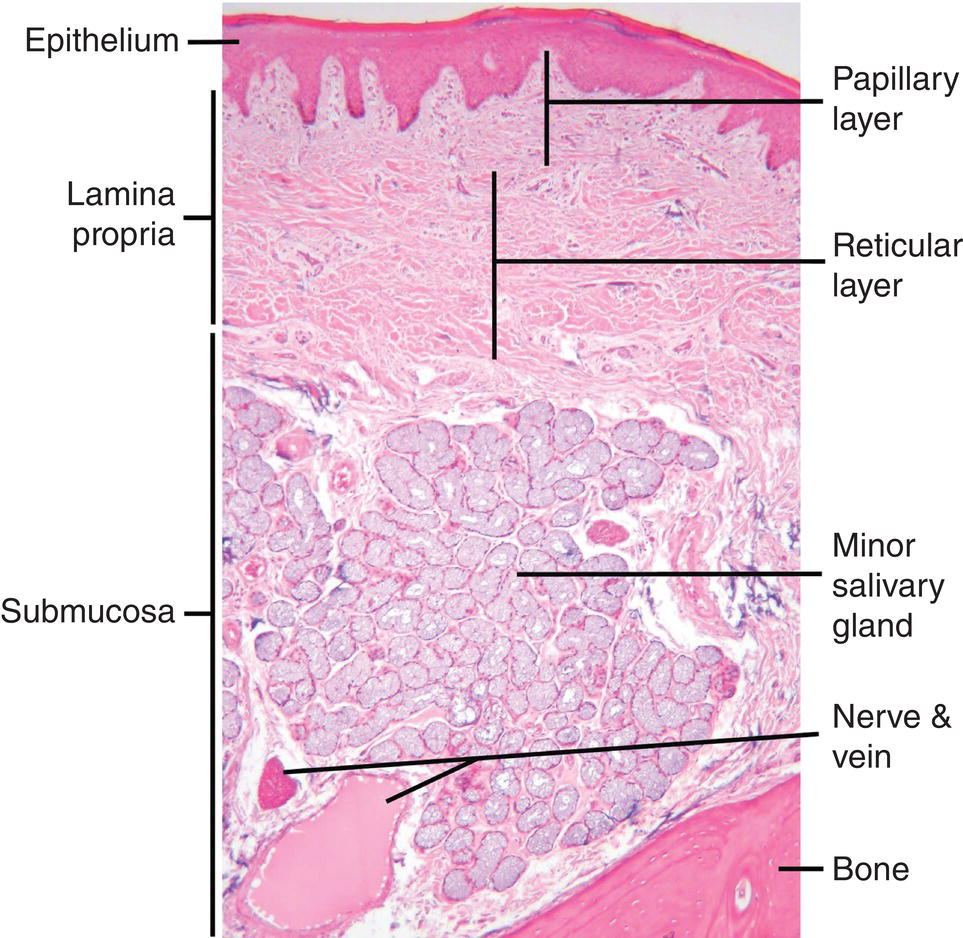
Figure 1.3 Light micrograph showing the layers and components of the oral mucosa. A submucosa is not present in all regions of the oral cavity.
Three subtypes of mucosa are found in the oral cavity. Lining or moveable mucosa has a stratified squamous non-keratinized epithelium, and is found on the inside of the lips and cheeks, in the vestibules and the floor of the mouth, and on the alveolar processes, the ventral surface of the tongue, and the soft palate. Masticatory mucosa has a stratified squamous keratinized or parakeratinized epithelium, and is found on surfaces subjected to the stresses induced by chewing our food (mastication), the hard palate and the gingivae. Specialized mucosa is found on the dorsal surface of the tongue. This mucosa is considered specialized because it forms four different types of papillae, three of which have taste buds through which taste sensations are received. Multiple fungiform papillae dot the dorsal anterior lingual surface, whereas two series of papillae with associated trenches or troughs, the medial circumvallate and lateral foliate papillae, are found far posterior near the base of the tongue (Fig. 1.4). The walls of the trenches are lined with specialized mucosa containing taste buds. The ducts of minor salivary glands (von Ebner’s glands) open into the trenches, and substances present in the trenches are flushed out by their secretions. Because the mucosa of the tongue has a stratified squamous keratinized epithelium, and because it plays an important role in mastication of food, this mucosa also may be classified as masticatory mucosa.
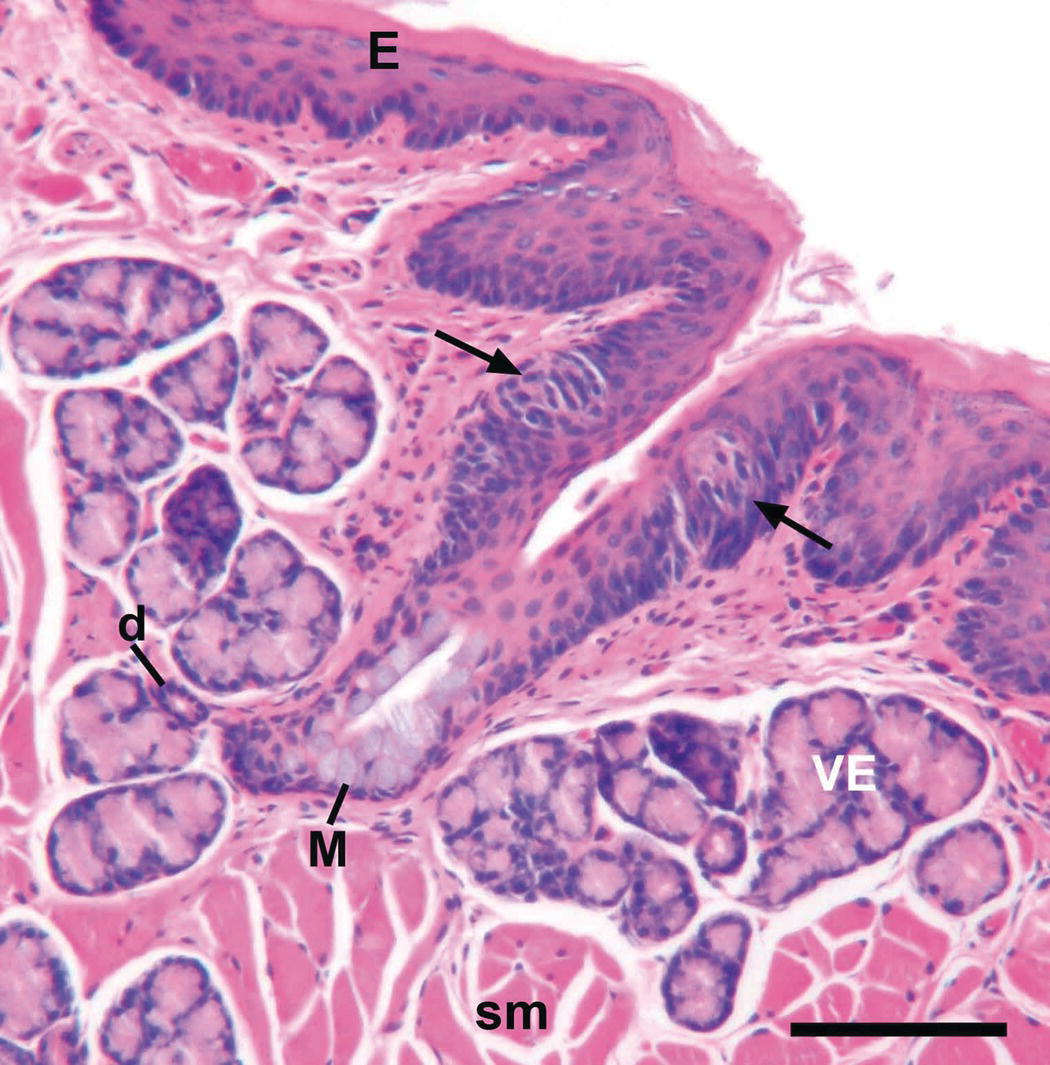
Figure 1.4 Light micrograph of a section through a foliate papillary trench of the tongue of a hamster. Arrows point to taste buds in the epithelial lining of the trench. Mucous cells (M) are present in the excretory duct of von Ebner’s gland (VE) as it opens into the trench. Small duct from a VE lobule (d); skeletal muscle (sm); stratified squamous keratinized epithelium (E). Scale bar = 100 μm.
The oral mucosa has several functions. These include providing protection from physical and chemical insults through its multilayered and keratinized epithelial surface; serving as a permeability barrier to prevent passage of microorganisms and toxic materials; detecting and responding to pathogenic microorganisms and foreign antigens through its immunological components; lubricating and moistening the oral surfaces through secretion of fluid and mucins; and general and special sensation through free and encapsulated nerve endings and taste buds.
Teeth
The teeth are among the most unique and complex structures of the body. Although they are designed to last a lifetime, teeth can be destroyed or lost in a relatively short time if we fail to take care of them. They consist of three different hard, or mineralized, tissues – dentin, cementum, and enamel – and are supported by a fourth hard tissue – bone (Fig. 1.5). The interface between the teeth and the gingivae is the only place in the body where a structure composed of hard tissues breaches a soft tissue covering. This unique anatomic arrangement is the site of significant pathology that can lead to the destruction of the supporting tissues of the tooth (periodontium) and its eventual loss.
Figure 1.5 Diagram illustrating the structure of a tooth and its supporting tissues.
(Modified from Ross, M.H. & Pawlina, W. 2011. Histology: A Text and Atlas, 6th edition, Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia. Reproduced by permission of Wolters Kluwer Health.)
Humans have two sets of teeth, the primary, or deciduous, teeth and the permanent teeth. The primary teeth are the first set to form and erupt into the oral cavity, beginning at about 6 months of age. There are a total of 20 primary teeth, 10 in the maxilla and 10 in the mandible, arranged in the form of an arch. On each side (quadrant) of the arch of each jaw, there is a central incisor, lateral incisor, canine (or cuspid), and first and second molars. The permanent teeth, also called succedaneous or successional teeth, which replace the primary teeth beginning at 6 to 7 years of age, develop in relation to the primary teeth. The permanent molars, or accessional teeth, have no primary precursors and develop posterior to the second primary molars. There are a total of 32 permanent teeth, eight in each quadrant; these include the central and lateral incisors, canine, first and second premolars (or bicuspids), and first, second, and third molars (Fig. 1.1).
A tooth consists of a crown, containing the pulp chamber and one or more roots, which contain the pulp canals (Fig. 1.5). The anatomic crown is covered by enamel, the hardest biological substance known; the clinical crown is the portion of the crown exposed in the oral cavity. One or more cusps and ridges separated by grooves and sulci are present on the occlusal surface (upper or grinding surface) of premolars and molars. The incisal surface of incisors is flatter and thinner and that of canines is more pointed; these teeth function in biting and tearing. The surfaces of the crowns of premolars and molars that face the cheeks are the buccal or facial surfaces (Fig. 1.6). The surfaces of the crowns of incisors and canines that face the lips are the labial or facial surfaces. The surfaces of the maxillary teeth that face the palate are the palatal surfaces; the surfaces of the mandibular teeth adjacent to the tongue are the lingual surfaces. The surfaces of the teeth in each arch that face the adjacent teeth are the proximal surfaces. The proximal surface of premolars and molars facing the posterior part of the oral cavity is the distal surface; that facing the anterior part of the oral cavity is the mesial (toward the midline) surface. This convention is maintained for the incisors and canines: distal, toward the adjacent tooth in the arch closer to the posterior teeth; mesial, toward the midline.
Figure 1.6 Tooth surfaces and directions in the oral cavity.
(Modified from Tortora, G.J. 1995. Principles of Human Anatomy, 7th edition, Wiley, New York. Reproduced by permission of John Wiley & Sons.)
The main tissue of the tooth is dentin. Dentin supports the enamel, which covers the crown, and it forms the root of the tooth. Dentin encloses the pulp, which through its blood and nerve supply and immunologic and regenerative functions maintains the vitality of the dentin and the cells that produce it, odontoblasts. Odontoblasts line the periphery of the pulp and secrete and mineralize the matrix components of dentin, predominantly collagen. Each odontoblast has a long apical or distal cytoplasmic process, the odontoblast process, that extends partway through the dentin in a dentinal tubule. The dentinal tubules are created as the dentin is deposited around the odontoblast processes and the odontoblasts gradually move deeper into the pulp. Some of the dentinal tubules also contain nerve endings, which in conjunction with the odontoblasts and other nerve endings associated with the odontoblasts are responsible for the sensation of pain in dentin. Odontoblasts respond to challenges to the integrity of t/>
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


