Introduction
We investigated how young patients’ motivation for orthognathic surgery affected their satisfaction with treatment outcomes. The objective was to explore whether patients’ “possible selves” (ie, their ideas of what they might become in the future) and their parents’ proxy assessments of the patients’ possible selves were significantly correlated with the patients’ treatment satisfaction.
Methods
Questionnaire data were collected from 115 former patients (ages, 13-21 at time of surgery) and 117 parents (response rates, 41% and 42%, respectively), with responses from 95 patient-parent pairs. The patients’ motivations before surgery were assessed by determining how energized they were by thoughts about themselves after the surgery, and how much they had focused on the outcomes. The parents completed a parallel measure of their children’s motivation. Patient satisfaction was determined with the postsurgical patient satisfaction questionnaire.
Results
The more emotionally energized the patients had been before the surgery, the more satisfied they were with the outcomes (Spearman rho = .54, P <0.001). Similarly, the more these patients had focused on esthetic changes and improved functioning, the more satisfied they were with the outcomes (Spearman rho = .46, P <0.001; rho = .41, P <0.001, respectively). Parents’ recalls of their children’s motivation before the surgery were consistent with the children’s self-reports (all P <0.001) and correlated with the children’s satisfaction ( P <0.001 in the energized domain; P <0.01 for the esthetic changes domain).
Conclusions
Young patients’ recalls of their possible self-based motivation for orthognathic surgery were highly correlated with their treatment satisfaction. Oral surgeons and orthodontists should discuss with young patients and their parents the patient’s motivation during the consultation phase before treatment to assess how energized and focused they are on future treatment outcomes.
Based on the most recent data on occlusal characteristics and assuming that the most severe malocclusions are associated with an underlying skeletal discrepancy, Bailey et al estimated that 1.8 million people in the United States need surgery to correct a severe malocclusion. Advances in orthognathic surgery over the past 25 years—eg, computer imaging, rigid internal fixation, and shorter hospital stays —made surgery a viable option for many patients. In addition, the social acceptance of orthognathic surgery has increased over the years. Many patients become aware of their dentofacial deformity in early adolescence, and it is not surprising that the demographic profile of orthognathic patients is becoming increasingly younger. Because of these changes in the patient population, it seems important to understand how satisfied they are with the outcomes of their orthognathic surgeries and which factors can predict their level of treatment satisfaction.
Patients generally reported high satisfaction with the outcome of orthognathic surgery. For example, between 71% and 86.3% of patients reported that they would reelect surgical correction, 87% to 89% would recommend surgery to others, and between 80% and 100% of patients reported satisfaction with the surgery. Considering the increase in younger orthognathic surgery patients, it is interesting to explore whether satisfaction with surgery outcomes differs depending on the patients’ age. Although some authors found no differences in satisfaction levels between age groups, 2 studies showed clear evidence that the youngest patients were the least satisfied with the outcomes of orthognathic surgery. In a long-term assessment, Lazaridou-Terzoudi et al found that the youngest age group (14-20 years at the surgery) was most critical of their current appearance and less satisfied after the surgery than patients in the 2 other age groups (20-26 years and >26 years). In addition, Scott et al reported that older patients were more satisfied than younger patients at all postoperative times.
Because orthognathic surgery causes significant improvement in general well-being, self-esteem, self-concept, social interactions, overall body image, facial body image, and profile body image, it is worthwhile to consider why younger patients are not more satisfied. It is important to explore how orthodontists and oral surgeons can predict—before the surgery—which patients will most likely be dissatisfied with the outcomes of their treatment. This study suggests that young patients’ treatment motivation before surgery affects their satisfaction with the treatment outcome.
What do we know about patients’ motivation and the factors that influence their decisions to have surgery? Some studies analyzed the role of significant others on the patients’ surgical decision-making process. They showed that the opinions of others were an important decision-making factor for some patients. Flanary et al found that 31.1% of the patients reported that what others thought they should do was important for their own decision-making process. Garvill et al, in a longitudinal study with 27 patients, found that 52% had reached the decision on their own, but 48% were influenced by family members or professionals. Jacobson found that 22% of patients were urged by family members or friends. It seems important to consider that these influences might be even stronger for younger patients.
Several studies analyzed the relationships between these motivational factors and satisfaction with treatment outcomes. In a review based on other types of cosmetic surgery, Peterson and Topazian stressed that patients who had surgery to please parents or significant others, and who had vague, nonspecific expectations were more likely to be dissatisfied with the surgical results. Other studies focusing on orthognathic surgery showed that lack of support from significant others, unrealistic expectations, emotional unpreparedness, and pressure from others to undergo surgery led to dissatisfaction. In addition, Rispoli et al found that patients with more esthetic and functional concerns before surgery were more likely to be satisfied with the results. Considering this rather eclectic set of findings, the question arises whether a unifying explanation can be found for the relationship between patients’ motivations before surgery and their treatment satisfaction after surgery.
We suggest that considering patients’ “possible selves” as a unifying concept could provide a connection between patient motivation and satisfaction with the outcome of orthognathic surgery. “Possible selves” are the patients’ ideas of what they might become in the future. Possible selves can be positive and expressed as hopes or dreams about positive future identities. They can also be negative and take on the form of fears of whom the person might become in the future. Research on the use of possible selves in connection with psychological phenomena is extensive and covers many topics. Research based on this possible-self theory in health-related areas also addressed diverse phenomena. For example, some studies used the concept of possible selves to explore lifestyle-related behaviors such as alcohol abuse, smoking, and exercising. Other studies applied the concept of possible selves to chronic pain, depression, borderline personality disorder, and Alzheimer’s disease. However, this is the first study that applies this widely used concept to orthognathic surgery patients.
When considering the relationship between possible selves and orthognathic-surgery patients’ satisfaction with treatment outcomes, it is important to understand that these possible selves affect a person in 2 ways. First, the possible-selves concept energizes the person to work toward making positive possible selves become a reality or to prevent negative possible selves from becoming real. In this sense, possible selves affect the intensity or the strength of a patient’s motivation. Second, possible selves also provide a structure to a person’s motivations by affecting how clearly he or she focuses on a specific positive or negative possible self. This second motivational component can be understood as affecting the direction of the motivation.
Patients who consider undergoing combined orthodontic and orthognathic treatment are likely to differ in how they engage in possible self-images of themselves after the treatment. Some patients are excited to have surgery; they might be looking forward to positive changes in appearance or function. These patients are energized. On the other hand, some might not be excited about change and might suppress even thinking about the outcomes. Some patients might also be focused regarding their future possible selves. For example, they might imagine how they will look after the surgery and specifically how esthetic their profile will be or how their smile will change. Focused patients develop vivid images about their future possible selves, whereas nonfocused patients do not have a clear picture of the surgical outcomes. These differences clearly shape a patient’s motivation to undergo orthognathic surgery and, according to the theory of possible selves of Markus and Nurius, will determine their satisfaction when the possible selves are realized in the future. An application of this theory to the situation of orthognathic surgery patients therefore leads to the concrete hypotheses that (1) the more energized and enthusiastic patients are when thinking about a future, postoperative possible self, and (2) the more patients are clearly focused on their future, postoperative possible self, the more satisfied they will be with the outcomes of their surgery.
Material and methods
This study was approved by the Institutional Review Board for the Medical Sciences at the University of Michigan, Ann Arbor.
A total of 318 patients who had undergone orthognathic surgery at the Oral and Maxillofacial Surgery Department of the University of Michigan or in a private group practice of 3 oral surgeons in Ann Arbor, Mich, between January 1, 1996, and December 31, 2005, were contacted by their surgeons and informed about the study. These recruitment letters were accompanied by a survey for the patients and a survey for their parents with stamped return envelopes. The inclusion criteria for receiving this mailing were (1) patient age (13-21 years at the surgery), (2) a developmental dentofacial deformity that was corrected by the surgery, and (3) the ability to independently complete the questionnaire. Patients were excluded from the study if they were not in this age group, had surgery to correct secondary deformities resulting from trauma or tumors, or had surgery not involving the tooth-bearing part of the jaws (eg, genioplasty alone).
Thirty-seven questionnaires were not deliverable because of invalid addresses. One hundred fifteen patients (response rate, 41%) and 117 parents (response rate, 42%) returned the questionnaires. Of these surveys, 95 in each group came from a patient-parent pair. The patients’ average age at the time of surgery was 16.89 years (SD, 1.920; range, 13-21 years), and the average age when responding to the survey was 21.84 years (SD, 3.054; range, 15-31 years). Sixty-nine percent of the responding patients were female, and 31% were male. Of the 105 patients who identified their ethnicity, 97 were white, 4 were black, 3 were Hispanic, and 1 was Asian. Thirty-two patients (23%) had maxillary surgery, 62 (45%) had mandibular surgery, and 43 (31%) had surgery in both arches. Fourteen (12%) of the parent respondents were fathers, and 103 (88%) were mothers.
A comparison of the respondents and nonrespondents showed no significant differences between the 2 groups concerning providers. These analyses showed that female patients were more likely to respond than male patients (45.9% vs 33%; P = 0.02). The responding patients did not differ significantly from the nonrespondents in age at surgery (16.96 vs 16.90 years) or current age (21.80 vs 22.28 years). However, the respondents had a tendency to have had their surgery more recently than the nonrespondents (4.84 vs 5.39 years ago; P = 0.09).
The researchers gave the prepared mailings to the 4 oral surgeons, who then attached address labels and mailed the surveys to the parents of the former patients. A second mailing was sent 6 weeks later to patients and parents who had not responded to the first mailing. Six weeks after the second mailing, the nonresponding patients from the University of Michigan clinic received a third mailing.
The recruitment cover letters for the parents and the patients were written and signed by the patients’ providers. Because the parents received the survey and had to give it to their children, this ensured that the parents consented to have their children respond if they were under 18 years of age. No written consent and assent were required by the Institutional Review Board because the signatures on these forms would have revealed the respondents’ names.
Because the measurements of possible selves is domain specific and no prior research explored the role of possible selves for orthognathic surgery patients, it was necessary to develop the questions used to assess these concepts in this study. The reliability and validity of these questions will therefore be reported. In the patient survey, 12 questions concerning possible self and motivational issues were included ( Fig ). As can be seen from the wording of these questions, they have intuitive face validity. Four questions were designed to measure the energizing component of the patients’ possible selves. Eight items measured how much the patients had focused on the postoperative possible self.
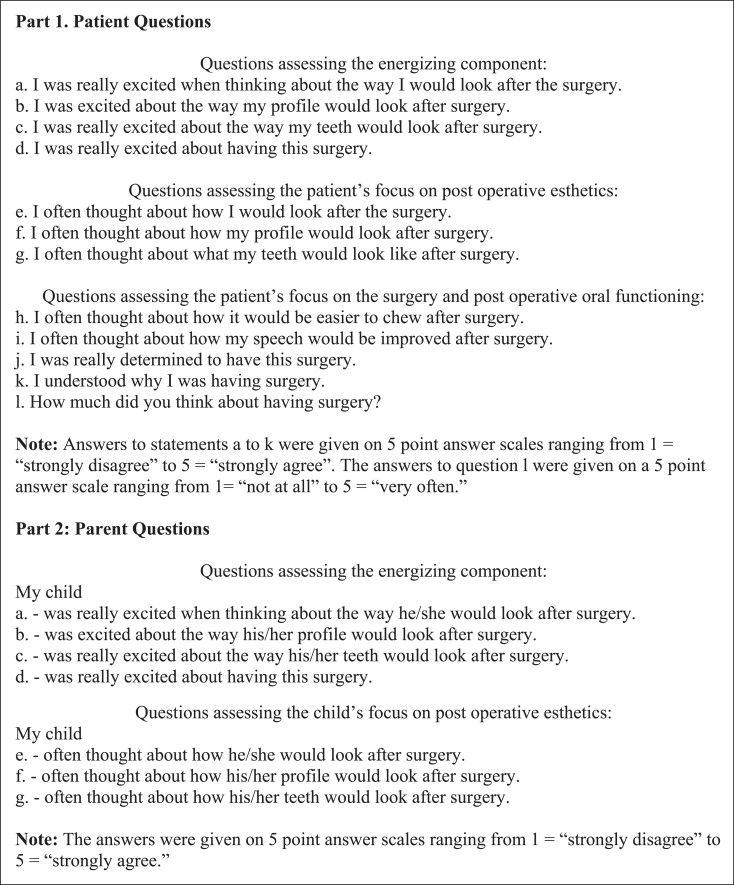
A factor analysis (extraction method: principal component analysis; rotation method: Varimax) was conducted to determine whether the 4 items concerning the energizing component and the 8 items about the focusing component consistently assessed these concepts. The 4 energizing items all loaded highly on a first factor (Cronbach α = 0.89). A “possible-self energizing component” index was therefore computed by averaging the answers to these 4 questions. The 8 focus questions loaded on 2 factors, with 3 items focusing on postoperative esthetics ( Fig , patient questions e-g) loading on 1 factor and 5 items focusing on the surgery and postoperative oral function ( Fig , patient questions h-l) loading on a second factor. The reliability of these 2 scales (Cronbach α = 0.82 and 0.71, respectively) justified computing 2 separate indexes: “possible self—focus I” and “possible self—focus II.” The results of the factor analyses showed that these scales have construct validity. This fact allowed us to use the created possible-self indices in the presentations of the results in Tables I and II .
| Low motivation 1 to 2.5 ∗ |
Medium motivation >2.5 to 3.5 |
High motivation >3.5 to 5 |
Mean | |
|---|---|---|---|---|
| Patients’ self-assessments of possible selves | ||||
| Energizing component † | n = 28 24.3% |
n = 29 25.2% |
n = 58 50.4% |
3.50 |
| Focus on postoperative esthetics (focus I) ‡ | n = 21 18.3% |
n = 19 16.5% |
n = 75 65.2% |
3.80 |
| Focus on postoperative oral function (focus II) § | n = 15 13.4% |
n = 40 35.7% |
n = 57 50.9% |
3.42 |
| Parents’ assessments of the children’s possible selves | ||||
| Energizing component ‖ | n = 31 27.2% |
n = 28 24.6% |
n = 55 48.2% |
3.41 |
| Focus on postoperative esthetics (focus I) ¶ | n = 20 17.5% |
n = 24 21.1% |
n = 70 61.4% |
3.74 |
∗ The indexes were computed by averaging the responses to the items in each scale. Answers were given on 5-point answer scales, with low scores indicating a low degree of energizing and focusing motivation, and higher scores indicating a higher degree of energizing and focusing motivation.
† This index was computed by averaging items 1, a to d, of the Figure.
‡ This index was computed by averaging items 1, e to g, of the Figure.
§ This index was computed by averaging items 1, h to l, of the Figure.
‖ This index was computed by averaging items 2, a to d, of the Figure.
¶ This index was computed by averaging items 2, e to g, of the Figure.
| Patients’ self-assessments of possible selves | |||
|---|---|---|---|
| Patients’ self- assessments of possible selves | Energizing component | Focus on postoperative esthetics (focus I) | Focus on postoperative function (focus II) |
| Energizing component | 1 | .86 ( P <0.001) n = 115 |
.70 ( P <0.001) n = 112 |
| Focus on postoperative esthetics (focus I) | .86 ( P <0.001) n = 115 |
1 | .59 ( P <0.001) n = 112 |
| Focus on postoperative function (focus II) | .70 ( P <0.001) n = 112 |
.59 ( P <0.001) n = 112 |
1 |
| Parents’ assessments of the children’s possible selves | |||
| Energizing component | .60 ( P <0.001) n = 93 |
.52 ( P <0.001) n = 93 |
.48 ( P <0.001) n = 90 |
| Focus on postoperative esthetics (focus I) | .54 ( P <0.001) n = 93 |
.58 ( P <0.001) n = 93 |
.43 ( P <0.001) n = 91 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


