Delayed tooth eruption can affect the accuracy of orthodontic diagnosis and treatment planning and could delay overall treatment. A girl, aged 7 years 4 months, who had unilateral delayed eruption of several teeth was successfully treated. The evaluation of delayed tooth eruption should be considered by the orthodontist because the role of these teeth can affect the overall treatment of malocclusion. In patients with delayed tooth eruption, careful and accurate diagnosis and treatment planning will allow the orthodontist to start treatment at the proper stage and might reduce the overall orthodontic treatment time.
Tooth eruption is a complicated developmental process when a tooth moves from its intraosseous location through the alveolar process to its final position of occlusion in the oral cavity. Numerous theories have been proposed to explain the movement of the tooth during eruption. They have implicated almost every tissue in or near the erupting tooth as a mediator of the process : growth of root, establishment of the periodontal ligament, alveolar bone growth and remodeling, increased pressure from cellular proliferation, and increased vascular pressure in the periapical tissue or pulp.
When a tooth emerges into the oral cavity significantly later than the established norms according to sex and ethnic background, it is considered a delayed tooth eruption. Delayed eruption of permanent teeth is one of the more severe problems that can occur during the mixed dentition stage and cause a significant concern for children and their parents. A delay in the eruption of permanent teeth might affect an accurate orthodontic diagnosis and treatment planning and could prolong overall treatment time. As a result, delayed tooth eruption is an important clinical problem that can significantly affect a patient’s proper orthodontic care.
Delayed tooth eruption has been associated with local, systemic, and genetic factors. Clinically, delayed tooth eruption is any of the following conditions: the normal eruption time has been exceeded, a tooth is absent in the dental arch and shows no potential for eruption, an unerupted tooth has complete root formation, or a contralateral tooth has been erupted for at least 6 months.
This case report presents a girl, aged 7 years 4 months, with delayed eruption of a mandibular left canine and the maxillary left first and second molars, and their orthodontic management.
Case report
The patient was referred to an orthodontist (K.T.) at a private orthodontic practice in Okayama, Japan, and examined for possible orthodontic treatment. She had a convex profile, a protrusive upper lip, and a Class II skeletal pattern. Her facial form was mesocephalic with good symmetry. She was in good general health and had no history of major systemic diseases or dental trauma. Intraorally, her mandibular dental midline was deviated approximately 2 mm to the right side relative to her facial midline, and she had an anterior open bite. She had a Class II end-on molar relationship on the right side and a mesial-step molar relationship on the left side, along with a deep palatal vault. She was observed to have a tongue-thrust habit and mouth breathing.
The treatment objectives were to obtain normal overjet and overbite, establish a Class I molar relationship, provide space for the erupting permanent dentition, and improve facial esthetics by correcting the protrusive upper lip.
The patient started her phase 1 treatment when she was 8 years old. To flatten the deep palatal vault, improve inadequate nasal capacity, and provide space for the erupting permanent teeth, a W-arch fixed expander was delivered for the maxillary arch. It was banded on the maxillary second deciduous molars because the maxillary left first permanent molar had not emerged. Tongue spurs were soldered onto the W-arch fixed expander and delivered for the mandibular arch. The mandibular dental arch was also expanded by using a W-arch fixed expander to maintain the buccolingual relationships of occlusal contacts in the posterior teeth during expansion and to provide space for the erupting permanent teeth.
When the patient was 9 years 1 month old, her appliances were removed. At this point, her maxillary left first permanent molar was erupting slowly. The mandibular right permanent canine was emerging, but the left deciduous canine showed no mobility. It was recommended that the patient have the left deciduous canine extracted, but, since there was no mobility, the patient and her mother wanted to wait a bit to extract it. When the patient was 10 years old, she returned for her recall visit without having had the deciduous canine extracted yet ( Fig 1 ). By the time she started her phase 2 orthodontic treatment, full fixed 0.022-in straight edgewise brackets (3M Unitek, Monrovia, Calif) were bonded, and a cone-beam computed tomography (CBCT) image was taken to observe the status of her retained deciduous canine. There was almost no root resorption around the apex of the deciduous tooth, and the impacted canine had more root development than the root length expected for eruption (tooth eruption begins when three quarters of the final root length has been established) and remained unerupted ( Figs 2 and 3 ). It was recommended that she have the deciduous canine extracted at the same time as the impacted tooth was surgically exposed. Because of financial issues, the patient only had the deciduous canine extracted. After 3 months of observation, the tooth was considered to be delayed in eruption, and her family finally decided to surgically expose the impacted tooth ( Fig 4 ).




An open-coil spring was inserted between the adjacent teeth. The spring had sufficient pressure to just counterbalance the forces of the chain elastic. It was also necessary to use light forces (no more than 2 oz) with a stiff archwire (0.018 × 0.025-in stainless steel in a 0.022-in slot) and to maintain adequate space with a closed-coil spring on the archwire. The added stiffness minimized the undesirable “roller-coaster” effect caused by intrusion of the anchor teeth ( Fig 5 ). The impacted tooth finally erupted and was guided into occlusion. Once the mandibular canine had reached the desired position in the dental arch, detailing was done ( Fig 6 ). At this stage, the maxillary left second molar still had not emerged. A fixed retainer was placed from canine to canine in the mandible and from lateral incisor to lateral incisor in the maxilla before debonding. The total phase 2 treatment time for this patient was 23 months. She and her mother were pleased with the esthetic results.

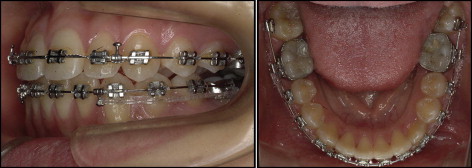
The posttreatment records indicate that the treatment objectives were achieved. Class I canine and molar relationships were established with a canine protected occlusion. The mandibular dental midline was almost coincident to the facial midline, and her overbite and overjet were improved.
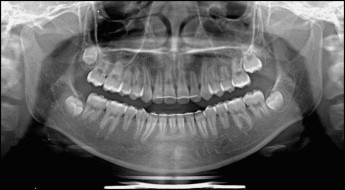
The posttreatment panoramic radiograph showed proper space closure and acceptable root parallelism. There were no significant signs of bone resorption. However, some areas showed signs of apical root resorption. The maxillary left second molar was developing and erupting slowly ( Fig 7 ).

Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


