Introduction
The aim of this community-based trial was to compare the effectiveness of the quad-helix appliance and removable plates for treating posterior crossbite.
Methods
Ninety-nine patients were randomly divided into 3 groups: quad-helix, expansion plate, and untreated. All subjects were in the mixed dentition, had posterior crosssbite, no sucking habits, no previous orthodontic treatment, and no Class III malocclusion. The following aspects were evaluated: posterior crossbite correction, maxillary and mandibular intermolar and intercanine expansions, length of treatment, cost-benefit analysis, success rate, and number of complications.
Results
The length of treatment and the costs were higher in the expansion plate group than in the quad-helix group. The success rates were similar for the quad-helix and the expansion plate groups, and the number of complications was higher in the quad-helix group. No self-correction was observed in the untreated group, and relapses occurred in both experimental groups.
Conclusions
The average treatment time was significantly shorter and 11% less expensive than in the quad-helix group, making it the more cost-effective choice for treatment.
Posterior crossbite is a malocclusion seen frequently in the deciduous and mixed dentitions (8% and 22%, respectively). It can be unilateral or bilateral and might develop during the mixed dentition. The etiology of this malocclusion can be dental, skeletal, or functional alone, or in combination. The most common form of posterior crossbite is unilateral with functional shift of the mandible toward the crossbite side.
Unilateral posterior crossbite might be associated with mandibular displacement. Some reports suggest that posterior crossbite might increase the risk of later temporomandibular joint dysfunction; however, other studies found this association weak and inconsistent.
Early treatment of posterior crossbites by means of maxillary expansion is currently advocated to redirect the erupting teeth into their normal positions and to eliminate premature occlusal contacts, thereby favoring beneficial dentoskeletal changes during growth periods.
For treatment of children with posterior crossbite, various methods have been suggested: rapid maxillary expansion, quad-helix appliance (QDH), removable plates, and grinding. However, the choice of treatment during the mixed dentition is focused on the transversal expansion of the maxillary teeth.
Earlier studies showed equal effectiveness for the QDH and removable plates in the treatment of posterior crossbite. On the other hand, 2 systematic reviews indicated that more scientific evidence from well-designed randomized controlled trials is needed to determine the most effective treatment for early correction of unilateral posterior crossbite and effective cost analysis.
We conducted a community-based trial to compare the effectiveness of the QDH and removable plates for treating unilateral dental and functional posterior crossbite. Our hypothesis was that the QDH and the removable plate would have equal effectiveness, equal costs, and equal numbers of complications, whereas the untreated group (control) would not show self-correction.
Material and methods
This was a community-based trial designed to produce more evidence of the efficacy of the 2 most popular techniques available to treat posterior crossbite in the mixed dentition. We also focused on access to treatment by evaluating the cost effectiveness of these orthodontic appliances. The subjects in this study were from public schools and the Santo Amaro Social Project, conducted by the University of Pernambuco, Recife, Pernambuco, Brazil. The Santo Amaro Social project enrolls about 700 children aged between 7 and 17 years. It is a social program aimed at supporting sports activities for a large underprivileged community located in a poor area of Recife known as the Santo Amaro favela. This community project also provides primary health care for the participants, including oral hygiene.
The trial was conducted in the small dental clinic of the Santo Amaro area, a basic dental unit in the center of the favela.
The sample comprised 99 children from that community, a sample large enough to produce statistically significant results.
The treatments were funded by the University of Pernambuco and a research grant from the Ministry of Education of Brazil (CAPES); the treatment was free for the patients. The target children had both unilateral posterior dental and functional crossbites in the mixed dentition (all incisors and permanent first molars were already present).
To meet the inclusion criteria, the patients had no sucking habits, previous orthodontic treatment, or Class III malocclusion; they all had skeletal posterior crossbite. The skeletal posterior crossbite was diagnosed by examining the casts models and anteroposterior cephalometric radiographs.
The study was approved by the ethics committee of the University of Pernambuco. The parents or guardians were informed of the purpose of the study and signed the informed consent document allowing their children to be treated.
The 99 children were randomly divided into 3 groups: QDH, expansion plate (EP), and untreated controls. For randomization, numbers were randomly drawn from a plastic bag. Each child received a number from 1 to 99.
One specialist orthodontist in practice for over 10 years (F.G.) diagnosed, took impressions (made the molds), placed the appliances, and followed the treatment plan.
Since both the QDH and the EP are recommended for treating functional and dental posterior crossbites, we chose these 2 appliances to be used in our trial.
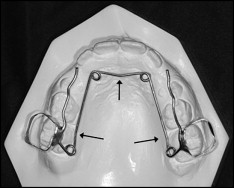
The QDH appliances were made of 0.9-mm stainless steel wire with stainless steel bands attached with glass ionomer cement to the maxillary first molars ( Fig 1 ). The degree of activation of the appliance was adjusted to allow for the retention of the band on 1 side to pass from the central fossa of the first permanent molar when the other band was placed on the molar. To try to prevent or compensate for rotation and buccal tipping, the arms of the QDH were held parallel to each other when activated, and a crown torque was incorporated into the appliance so that the molar bands were kept parallel ( Fig 2 ). The QDH was activated once a month until the posterior crossbite was corrected.
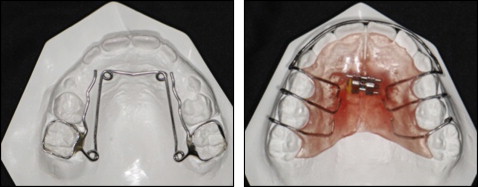
The EP had a midline 10-mm screw, 4 stainless steel clasps on the deciduous and permanent first molars, and an acrylic covering ( Fig 1 ). It was recommended that the screw be opened a quarter rotation every week until the posterior crossbite was corrected. The patient and parents or guardians were instructed to use the EP day and night except for tooth brushing.
The patients and parents received both oral and written information on the treatment, oral hygiene, and maintenance of the appliance.
In this study, we evaluated the following: correction of posterior crossbite, amounts of maxillary and mandibular intermolar and intercanine expansion, length of treatment, cost-benefit (treatment time, number of appliances used, and number of appointments) success rate, and number of complications. Palatal expansion and crossbite correction were measured on the study casts by 1 masked investigator (J.G.) using a sliding caliper (model I 395 24989 MFGIN, Rocky Mountain Orthodontics, Denver, Colo) to the nearest 0.1 mm. The investigator was unaware of the type of appliance used by the patient and the length of treatment (pretreatment, after expansion, after 6 months of retention, or 6 months after removal of the retention plate).
The following measurements were made on the study casts: (1) maxillary and mandibular intermolar widths: the width between the central fossae of the right and left maxillary and mandibular first permanent molars; and (2) maxillary and mandibular intercanine widths: the width between the crown tips of the right and left deciduous or permanent maxillary and mandibular canines (Fig 3). The mandibular arch was measured to verify the spontaneous expansion achieved after the maxillary expansion.
However, as expected in the mixed dentition, some children did not yet have their permanent canines after exfoliation of the deciduous teeth; as a result, those children could not have this measurement taken.
Dropouts and treatments not completed within 12 months were classified as unsuccessful.
For both techniques, the patients were evaluated every 4 weeks; no overcorrection was produced, and each child with the desired crossbite correction had a plate placed for retention of the treatment to be used 24 hours a day for 3 months and, after the first 3 months, for 3 more months just at night.
The untreated group received no orthodontic treatment during the trial period. According to the ethics committee’s guidelines, for all children in the untreated group who had no self-correction, the treatment would be provided at no cost as part of another trial.
Statistical analysis
The sample size calculation established an error of 5% and a power of 95%. To detect any differences in length of treatment between the 2 methods, the means and standard deviations were calculated based on the data from the study of Hermanson et al (8.00 ± 3.00 for the QDH; 12.00 ± 5.00 for the EP). The sample should include 27 patients per group to show a statistically significant difference. To make up for possible dropouts, we decided to add 20% to the number of children, so we ended up with a total of 99 children, 33 in each group.
To test the examiner’s internal reproducibility, after examining 45 sets of study casts, we randomly selected 20 to be reexamined after 1 week to ensure internal agreement. The results of the paired t test for the repeated measurements of intermolar and intercanine maxillary widths performed on 20 sets of study casts showed high agreement of the correlation coefficients of 0.98 (0.97-0.99) for the maxillary molars and 0.95 (0.88-0.98) for the maxillary canines.
We used SPSS software (version 15, Statistical Package for the Social Sciences, Chicago, Ill) to analyze the data. The Pearson chi-square test and the Fisher exact test were used for analysis of differences between the variables. The t test was used for continuous variables with equal or different variances. Analysis of variance (ANOVA) with the Tukey test were used to compare independent groups, the effects of the treatment, the length of the treatment, the amount of expansion, and the costs between groups.
Results
The numbers, sexes, and ages of the patients are shown in Table I .
| Group | |||||
|---|---|---|---|---|---|
| QDH | EP | Control | Total group | ||
| Variable | (n = 33) | (n = 33) | (n = 33) | (n = 99) | P value |
| Age: mean ± SD | 8.00 ± 0.79 | 7.82 ± 0.85 | 8.09 ± 0.81 | 7.97 ± 0.81 | P † = 0.387 |
| Sex: n (%) | |||||
| Male | 7 (21.2) | 15 (45.5) | 19 (56.6) | 41 (41.4) | P ‡ = 0.009 ∗ |
| Female | 26 (78.8) | 18 (54.5) | 14 (42.2) | 58 (58.6) | |
All children treated in this trial with both appliances had their crossbite corrected. However, 3 patients in the EP group showed crossbite correction only after the 12 months of treatment ( Table II ); no self-correction was observed in the untreated group (control). Relapses occurred in 9.1% of the 2 experimental groups after 1 year of follow-up ( Table III ).
| Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| QDH | EP | Total | ||||||
| Variable | n | % | n | % | n | % | P value | Prevalence ratio (CI at 95%) |
| Length of treatment until posterior crossbite correction | ||||||||
| Up to 3 months | 18 | 54.5 | 6 | 18.2 | 24 | 36.4 | P † = 0.009 ∗ | 2.00 (1.02-3.92) |
| 4 to 6 months | 9 | 27.3 | 17 | 51.5 | 26 | 39.4 | 0.92 (0.41-2.12) | |
| 7 or more | 6 | 18.2 | 10 | 30.3 | 16 | 24.2 | 1.00 | |
| Number of visits | ||||||||
| ≤10 | 18 | 54.5 | 16 | 48.5 | 34 | 51.5 | P † = 0.622 | 1.13 (0.69-1.84) |
| >10 | 15 | 45.5 | 17 | 51.5 | 32 | 48.5 | 1.00 | |
| Number of appliances | ||||||||
| One | 28 | 84.8 | 24 | 72.7 | 52 | 78.8 | P † = 0.228 | 1.51 (0.72-3.18) |
| Two | 5 | 15.2 | 9 | 27.3 | 14 | 21.2 | 1.00 | |
| Final result | ||||||||
| Success | 33 | 100.0 | 30 | 90.9 | 63 | 95.5 | P † = 0.238 | ‡ |
| Failure | – | – | 3 | 9.1 | 3 | 4.5 | ||
| Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| QDH | EP | Total group | ||||||
| Relapse | n | % | n | % | n | % | P value | RR (CI at 95%) |
| Yes | 3 | 9.1 | 3 | 9.1 | 6 | 9.1 | P ∗ = 1.000 | 1.00 |
| No | 30 | 90.9 | 30 | 90.9 | 60 | 90.9 | 1.00 (0.43-2.32) | |
| TOTAL | 33 | 100.0 | 33 | 100.0 | 66 | 100.0 | ||
The average treatment length to correct the unilateral posterior crossbite was higher with the EP (6.12 months ± 3.25) than with the QDH (4.24 months ± 2.05) ( Table IV ).
| Group | ||||
|---|---|---|---|---|
| Variable | Statistics | QDH | EP | P value |
| Length of treatment until crossbite correction (mo) | Mean | 4.24 | 6.12 | P † = 0.007 ∗ |
| Median | 3.00 | 5.00 | ||
| SD | 2.05 | 3.25 | ||
| Minimum | 2 | 2 | ||
| Maximum | 9 | 15 | ||
| Number of complications | Mean | 2.15 | 1.67 | P † = 0.122 |
| Median | 2.00 | 2.00 | ||
| SD | 0.80 | 0.50 | ||
| Minimum | 1 | 1 | ||
| Maximum | 3 | 2 | ||
| Number of appliances used (cost) | Mean | 17.27 | 19.09 | P ‡ = 0.235 |
| Median | 15.00 | 15.00 | ||
| SD | 5.46 | 6.78 | ||
| Minimum | 15 | 15 | ||
| Maximum | 30 | 30 | ||
| Number of visits | Mean | 11.48 | 11.61 | P † = 0.869 |
| Median | 10.00 | 11.00 | ||
| SD | 3.01 | 2.93 | ||
| Minimum | 8 | 8 | ||
| Maximum | 20 | 18 | ||
Our study design was a prospective cohort, and our patients were followed for approximately 20 months after correction, since our mean correction time was 4.5 months, depending on the choice of appliance.
The average numbers for loss of appliance, displacement of appliance, breakage of appliance, and missed appointments in the QDH group were 12.1% higher than in the EP group (39.4% for the QDH group, 27.3% for the EP group).
No appliances were lost in the QDH group, but 24.2% were lost in the EP group; failure occurred in one third of the QDH patients during the treatment, but there were no failures in the EP group. Breakage of appliances occurred in 18.2% of the QDH patients and in none of the EP patients. For both experimental groups, the average number of clinical visits and the number of teeth involved in the crossbite were about the same.
Because the patients in the EP group could activate the appliance at home, loss of appointments did not interfere with the treatment, whereas those in the QDH group could not miss appointments because it would represent a delay in treatment. The number of missed appointments was 12.1% higher in the QDH group than in the EP group (33.3% × 21.2%). The results of all complications can be seen in Table V .
| Group | ||||||||
|---|---|---|---|---|---|---|---|---|
| QDH | EP | Total group | ||||||
| Variable | n | % | n | % | n | % | P value | PR (CI at 95%) ǁ |
| Complication | ||||||||
| Yes | 13 | 39.4 | 9 | 27.3 | 22 | 33.3 | P ‡ = 0.296 | 1.30 (0.81-2.09) |
| No | 20 | 60.6 | 24 | 72.7 | 44 | 66.7 | 1.00 | |
| Loss of appliance | ||||||||
| Yes | – | – | 8 | 24.2 | 8 | 12.1 | P § = 0.005 ∗ | † |
| No | 33 | 100.0 | 25 | 75.8 | 58 | 87.9 | ||
| Displacement of appliance | ||||||||
| Yes | 11 | 33.3 | – | – | 11 | 16.7 | P ‡ <0.001 ∗ | † |
| No | 22 | 66.7 | 33 | 100.0 | 55 | 83.3 | ||
| Breakage of appliance | ||||||||
| Yes | 6 | 18.2 | – | – | 6 | 9.1 | P § = 0.024 ∗ | † |
| No | 27 | 81.8 | 33 | 100.0 | 60 | 90.9 | ||
| Missed appointments | ||||||||
| Yes | 11 | 33.3 | 7 | 21.2 | 18 | 27.3 | P ‡ = 0.269 | 1.00 |
| No | 22 | 66.7 | 26 | 78.8 | 48 | 72.7 | 1.33 (0.83-2.16) | |
| Total | 33 | 100.0 | 33 | 100.0 | 66 | 100.0 | ||
∗ Significant difference at 5.0%
† Not possible to determine due to null occurrence
ǁ Prevalence ratios of the QDH group in relation to the EP group.
For the cost-benefit analysis, the average number of appliances used was 1.82 higher in the EP group than in the QDH group, and the length of treatment was also longer in the EP group ( Tables II and IV ). The laboratory costs were the same for both appliances. Comparing the total treatment costs, the number of clinical visits, the length of treatment, and the number of appliances needed, the EP group cost 10.53% more than QDH group ( Table IV ).
There were no significant differences between the groups in regard to the initial intercanine and intermolar distances ( Tables VI and VII ). We can see significantly larger amounts of expansion in maxillary intermolar and intercanine distances in the QDH and EP groups than in the control group. No significant differences were found between the 2 experimental groups. In the mandibular arch, however, the QDH group had greater intermolar expansion than did the EP group and the control group ( Table VII ).



