The diagnosis of an impacted incisor with dilaceration refers to a dental deformity characterized by an angulation between the crown and the root, causing noneruption of the incisor. In the past, surgical extraction was the first choice in treating severely dilacerated incisors. The purpose of this case report was to present the correction of a horizontally impacted and dilacerated central incisor through 2-stage crown exposure surgery combined with continuous-force orthodontic traction. The tooth was successfully moved into its proper position. The treatment is discussed, and the orthodontic implications are considered, with a review of the current literature on this topic.
The abnormality of root dilaceration, which presents itself as the deformed development of a tooth, has been long recognized. The term refers to an angulation, which can occur anywhere along the length of the tooth—ie, its crown, cementoenamel junction, along the root, or only involving the apex of the root—resulting in disruption of the normal axial relationship of the tooth. The malformation occurs by displacement of the crown, usually during early tooth development, in a vestibular or, less frequently, palatal direction, while root growth is still progressing in a cranial direction. In the literature, a distinction is also made between vestibular and lateral root bending. With continued tooth development, later tooth eruption becomes unlikely, and the tooth remains unerupted.
Most frequently, this deformation occurs unilaterally in the maxillary permanent central incisors. It has as also been reported in the maxillary deciduous incisors, the mandibular permanent incisors, and the maxillary permanent canines and premolars. There are also few reports of patients having 2 affected dilacerated teeth (in 1 patient, 11 and 21 were involved; in 2 others, 21 and 22 were simultaneously affected ).
Dilacerations are estimated to occur in 3% of all permanent dentitions. However, the etiology of dilaceration is not yet fully understood. Traumatic injury to the deciduous predecessors and ectopic development of the tooth germ are the 2 commonly cited causes of this anomaly, so that the entity has continued to present something of a clinical puzzle.
The treatment of a dilacerated anterior tooth is challenging for the clinician, because of its difficult position and the abnormality of the root. Treatment often involves surgical removal with subsequent orthodontic methods to either close the space or keep it open until the patient reaches an age when implants or prosthetic treatment can be performed. Both methods have associated problems. Alternatively, surgical exposure followed by orthodontic traction is suggested to save an impacted dilacerated incisor.
This article presents a patient with a horizontally impacted and dilacerated maxillary left central incisor. With the help of 2 stages of surgical crown exposure combined with continuous orthodontic traction, the dilacerated incisor was successfully moved into its proper position.
Diagnosis and etiology
A 10-year-old white girl was referred by her general dentist to the orthodontic department of the University of Bonn in Germany for consultation. The chief concern was the noneruption of the maxillary left central incisor; this had resulted in an unesthetic appearance and a psychologic compromise ( Figs 1 and 2 ). The child was physically healthy, and there was no evident history of a traumatic injury in the frontal oral region. However, because of the severely displaced position of 22, with an incisal cant, dental trauma could not be excluded. Examination of the oral cavity showed dental caries in the deciduous teeth and a deep insertion of the maxillary labial frenulum.

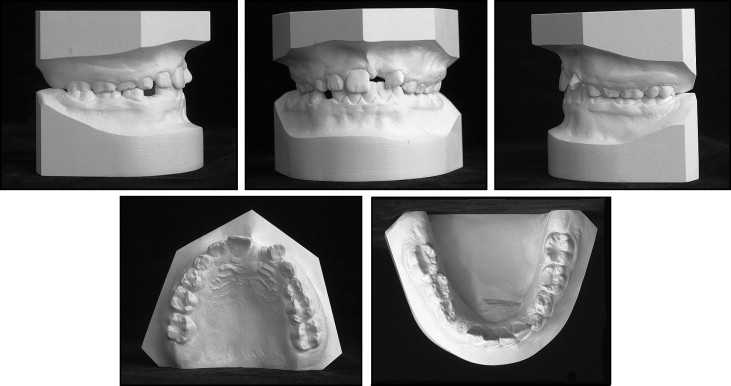
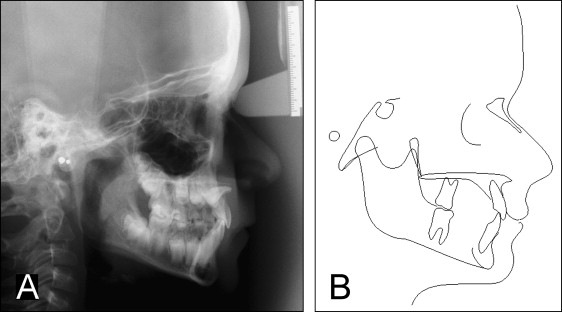
The patient had a skeletal Class I occlusion with a balanced facial pattern. The analysis of the lateral cephalometric radiograph disclosed normal cephalometric values. Intraoral examination showed an early mixed dentition and an Angle Class I molar relationship. The impaction of the maxillary left central incisor had resulted in drifting of the adjacent teeth with a resultant midline deviation and a 45° mesial rotation of the left lateral incisor. The impacted incisor’s crown was palpable high in the labial sulcus. There were minor arch length discrepancies in both arches and a crossbite of the first molar on the right side.
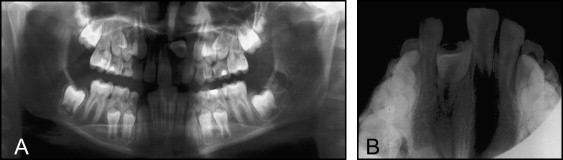
The panoramic and maxillary occlusal radiographs demonstrated an impacted maxillary left central incisor ( Fig 3 ). The tooth’s morphology and position were easily visible in the lateral cephalometric radiograph ( Fig 4 ), showing a horizontally displaced tooth, with its crown rotated more than 100° from normal, and its incisal tip just below the floor of the nose. The palatal surface of the crown was facing forward “like the hand of a traffic policeman,” and the root was shortened. It was not possible to exactly define the root apex on the conventional radiographs.
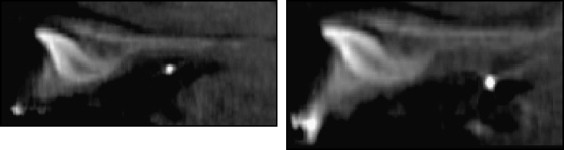
Thus, a TC-Dentascan (NewTom, Newtom Deutschland AG, Marburg, Germany) was performed, and evaluation confirmed the presence of the impacted tooth localized in the body of the premaxilla with a bend at the root’s apical third ( Fig 5 ). The dilacerated tooth showed complete apex formation. In addition, the tooth had a marked labiopalatal curvature adjacent to the cortical plate of the bone of the palatal vault, and the crown-root angle was judged to be about 45°. The use of TC-Dentascan was essential to show the root dilaceration and to focus on potential problems associated with the orthodontic movement of the tooth.
Treatment alternatives and objectives
The following treatment options were considered.
- 1.
Surgical extraction of the impacted incisor and restoration with a prothesis or an implant after orthodontic space opening when growth had ceased.
- 2.
Surgical extraction of the impacted incisor, orthodontic space closure, and prosthodontic restoration of the left lateral incisor as the central incisor at a later stage.
- 3.
Orthodontic space opening, uncovering the tooth by using the closed eruption technique and orthodontic traction of the tooth into proper alignment.
The treatment options were explained to the parents, and it was decided to attempt to bring the tooth into alignment.
Treatment alternatives and objectives
The following treatment options were considered.
- 1.
Surgical extraction of the impacted incisor and restoration with a prothesis or an implant after orthodontic space opening when growth had ceased.
- 2.
Surgical extraction of the impacted incisor, orthodontic space closure, and prosthodontic restoration of the left lateral incisor as the central incisor at a later stage.
- 3.
Orthodontic space opening, uncovering the tooth by using the closed eruption technique and orthodontic traction of the tooth into proper alignment.
The treatment options were explained to the parents, and it was decided to attempt to bring the tooth into alignment.
Treatment progress
The patient was referred to the general dentist for restoration of the carious deciduous teeth. Subsequently, a fixed appliance was placed on the maxillary teeth to create space for the impacted central incisor. Bands with lingual Burstone slots were placed on the maxillary first molars, and orthodontic brackets were bonded to the 3 anterior permanent teeth. Initially, the posterior crossbite was corrected with an asymmetrically activated transpalatal arch. Afterward, the rotated left lateral incisor was aligned by means of a cantilever, which was fully inserted to the lateral incisor’s slot and ligated to the left molar band. Leveling was then continued with a 0.0175-in multistrand wire, followed by a 0.016 × 0.016-in beta-titanium alloy wire and a 0.016 × 0.022-in stainless steel wire with an open-coil spring in the position of the unerupted central incisor ( Fig 6 ).





