Eruption disturbances such as impaction and ankylosis complicate orthodontic treatment because soft-tissue and hard-tissue considerations must be taken into account. Treatment is further complicated when such eruption disturbances occur in a growing patient. Extraction of impacted or ankylosed teeth can be an option that carries the weight of additional prostheses and bony defects, whereas exposure or luxation followed by orthodontic traction can preserve the patient’s teeth and bony structure with improved esthetics. Therefore, an accurate diagnosis is needed in establishing an efficient and effective force system to achieve the desired tooth movements with few unwanted sequelae. This case report describes the process of differential diagnosis with the aid of 3-dimensional imaging in constructing a force-driven system, using the centers of resistance as reference points, to successfully bring a pair of impacted maxillary canines into alignment and protract a mandibular molar to achieve an acceptable occlusion in an adolescent girl.
Eruption disturbances such as tooth impaction and ankylosis are relatively common but challenging because of the unpredictable biologic response of the alveolar bone and periodontal tissues. Maxillary canine impactions occur frequently, second only to third molar impactions, and could be associated with the long eruption path of the maxillary canines. In addition to some evident systemic factors such as genetic disorders and various local factors including supernumerary teeth, cysts, tumors, failure of resorption of the deciduous tooth roots, and reduced eruption space, spontaneous failure to erupt is a result of abnormal eruption paths and ankylosis. In particular, eruption failure without specific causes must be diagnosed, and intervention should occur as early as possible because the pathologic process will exacerbate the migration of neighboring teeth and lead to resorption of adjacent roots over time.
A wide range of treatment options for impacted canines has been reported, including extraction followed by prosthetic rehabilitation or canine substitution, and surgical exposure for orthodontic traction. Hyomoto et al proposed that mature roots and severe angulations are indicators for poor prognoses in dealing with cyst-related impacted teeth. Accordingly, extraction of impacted teeth is a readily selected treatment option in patients with excessive arch-length discrepancies or deeply located impacted teeth. On the other hand, in active growers without much space deficiency, the decision to extract the impacted tooth is not easy because prosthetic substitution is not possible until growth has stopped. Hence, a more progressive approach might be indicated for growing children even in challenging situations.
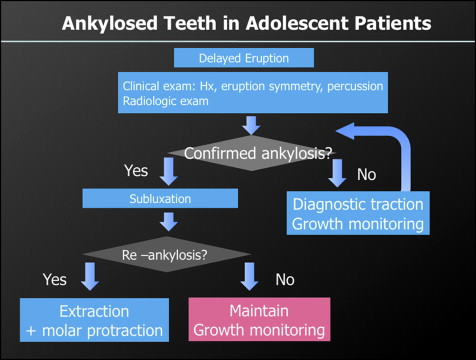
Ankylosis is defined as the fusion of cementum to alveolar bone. Patients with ankylosis are a concern to orthodontists because their malocclusions tend to worsen with time. Therefore, it is imperative to recognize ankylosis early and treat it accordingly. Ankylosis of molars often occurs from unknown causes and necessitates a strategic approach to avoid prosthetic restorations. There are several treatment options depending on the timing and severity of the ankylosis that can range from simple occlusal buildups to subluxation followed by orthodontic traction to extraction. As with impactions, the prognoses of ankylosed teeth are unpredictable, especially in active growers. Reankylosis of a successfully rescued ankylosed tooth can happen at any time during growth, only to lead to additional alveolar bone loss. Therefore, a timely decision as to whether to extract the tooth is important because a submerged ankylosed tooth can result in an alveolar bone defect.
The etiology of eruptive disturbances such as impactions and ankyloses is suggested to be multifactorial. Although the exact etiology has yet to be investigated, establishing a strategic diagnosis and constructing an efficient force system as well as a proper biologic assessment that considers all possible sequelae should precede any treatment. This case report presents the treatment and management of a patient with bilaterally impacted maxillary canines and an ankylosed mandibular first molar using a force-driven approach.
Diagnosis and etiology
A 10-year-old girl was referred to the Department of Orthodontics at Yonsei University Dental Hospital in Seoul, Korea, with the chief complaint of crooked teeth and impacted canines, which were previously diagnosed by a private dentist through a preliminary radiologic examination. Her medical and dental histories were not significant, and she had not yet reached menarche.
The initial extraoral views showed a relatively symmetrical face and straight profile ( Fig 1 ). Intraorally, the mandibular right permanent first molar and left deciduous second molar were in infraocclusion, and the upper midline was deviated 1 mm to the patient’s left. The maxillary arch showed moderate crowding with a tapered arch form, and the lateral incisors were in crossbite. The mandibular deciduous second molars were retained, and the permanent molars had an acceptable Class I relationship.

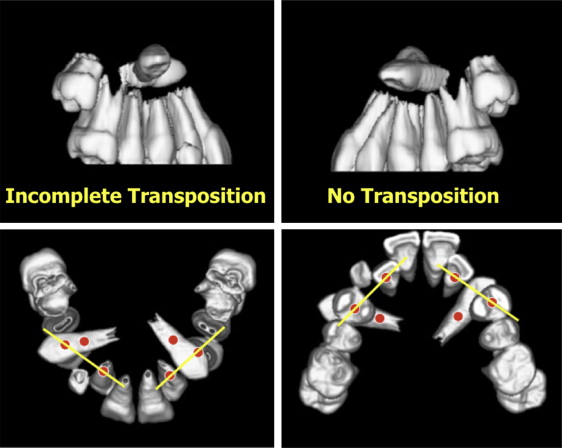
The panoramic radiograph showed bilateral horizontally impacted maxillary canines in the subapical area ( Fig 2 ). Incomplete eruption of the mandibular right first molar was also confirmed in the radiograph, and the initial periotest value was negative, which raised the suspicion of ankylosis. Developing mandibular third molar buds were evident as well. Computed tomography imaging followed by 3-dimensional (3D) rendering was performed to precisely locate the impacted maxillary canines and allowed for visualization of both canines positioned horizontally above the root apices of the adjacent premolars ( Fig 3 ).

The pretreatment lateral cephalogram showed a Class I skeletal relationship with a slightly hyperdivergent facial pattern ( Table ). The maxillary incisors were mildly labially inclined, and the mandibular incisors were slightly lingually inclined.
| Measurement | Norm | Initial | Final |
|---|---|---|---|
| SNA (°) | 81.1 | 82.8 | 82.9 |
| SNB (°) | 77.0 | 79.5 | 79.8 |
| ANB (°) | 3.0 | 3.3 | 3.1 |
| Wits appraisal (mm) | −2.8 | −1.3 | −3.1 |
| SN to Go-Me (°) | 35.6 | 39.6 | 39.2 |
| U1 to SN (°) | 105.4 | 110.4 | 107.8 |
| L1 to Go-Gn (°) | 94.6 | 85.6 | 88.9 |
| Upper lip to E-line (mm) | 1.7 | −0.9 | −1.2 |
| Lower lip to E-line (mm) | −2.8 | 1.4 | 1.8 |
Treatment objectives
The treatment objectives were to (1) relieve the crowding in the maxillary and mandibular arches and coordinate both arches by expansion of the maxillary arch, (2) relocate the impacted maxillary canines and bring them into alignment, (3) allow the mandibular premolars to erupt to the occlusal level, (4) perform adequate actions on the mandibular right first molar to establish a proper occlusion on the right side, (5) make the midlines coincident, and (6) maintain a desirable lateral profile.
Treatment objectives
The treatment objectives were to (1) relieve the crowding in the maxillary and mandibular arches and coordinate both arches by expansion of the maxillary arch, (2) relocate the impacted maxillary canines and bring them into alignment, (3) allow the mandibular premolars to erupt to the occlusal level, (4) perform adequate actions on the mandibular right first molar to establish a proper occlusion on the right side, (5) make the midlines coincident, and (6) maintain a desirable lateral profile.
Treatment alternatives
The most important things to consider while treating this patient were the impacted maxillary canines and the potentially ankylosed mandibular right first molar. According to Kuftinec and Shapira, horizontally impacted canines have a poor prognosis because of difficulties in both orthodontic traction and the unpredictable response of the periodontium. Moreover, this patient was in an actively growing phase, further complicating treatment. The best treatment option, therefore, had to be selected among several possibilities according to growth change.
First, extraction of the deciduous canine and observation for spontaneous eruption of the impacted canines were considered. Apparently, this treatment option is reported to be effective 80% of the time in 10- to 13-year-olds. Furthermore, Bedoya and Park reported that if the canine has not crossed the midline of the lateral incisor, there is a 91% chance that the canine will erupt on its own once the deciduous canine has been removed. However, in this patient, both canines were horizontally impacted; this led us to believe that spontaneous eruption without intervention would be highly unlikely, and that further delay in eruption would worsen the situation by allowing inclination of the adjacent teeth to occur.
A secondary option was to extract and then transplant the impacted canines to ease the relocation. However, autotransplantation of teeth carries the risk of ankylosis and can lead to failure of the development of surrounding alveolar bone. Progressive root resorption is another risk related to autotransplantation. In particular, the autotransplantation of canines is subject to other risks. For instance, the inaccessibility of horizontally impacted canines increases the chances for damage to the root and periodontal ligament during removal for autotransplantation. Impacted canines also tend to have thinner periodontal ligaments than normally functioning teeth. Furthermore, relocation into the desired canine position requires surgical shaping of the alveolus, with removal of alveolar bone.
Yet another option was to extract the impacted canines followed by prosthodontic rehabilitation or orthodontic closure of the remaining spaces. In this patient, because of her young age, the space for the canines would have to be maintained until the cessation of growth and maturation of the periodontium. In addition to the economic burden for additional prosthetic work, possible alveolar bone shrinkage could make the later implant work difficult. Space closure after extraction was not a readily acceptable option either because of the uncertainty of growth changes to the profile and possible narrowing of the tapered maxilla, which could in turn lead to poor arch coordination.
With regard to the ankylosed mandibular right first molar, several options were considered ( Fig 4 ). Subluxation of the tooth followed by inclusion into the arch with fixed appliances was the primary option, and this option also has the advantage of induction of alveolar bone development. However, subluxation nearly always carries the risk of reankylosis, which can further stunt alveolar bone growth. The other option available was to extract the ankylosed tooth, which can effectively deter further alveolar bone defect in active growers. After extraction, however, massive tooth movement would have to follow to prevent a serious bone defect, necessitating second molar protraction. Hence, a strategic and stepwise plan was crucial for this patient.