Introduction
Our objective was to report a patient treated with 3-dimensional virtual-surgery simulation-assisted asymmetric bilateral mandibular distraction osteogenesis.
Methods
A boy (age, 9.5 years) had mandibular hypoplasia and facial asymmetry, induced by bilateral condylar fractures at 4 years of age. The asymmetric bilateral mandibular distraction osteogenesis was planned to correct facial asymmetry and mandibular hypoplasia. The 3-dimensional virtual-surgery simulation results were 11 mm of horizontal distraction on the right side and 4.5 mm of horizontal and 18 mm of vertical distraction on the left side of the mandible. Bilateral ramus osteotomies were performed, and intraoral unidirectional distraction devices were inserted. After a 6-day latency period, distraction was performed at 1 mm per day, followed by a 5-month consolidation period. Transarch and interarch elastics and an acrylic plate were used during distraction and consolidation. Total treatment time was 30 months.
Results
Satisfactory outcomes were obtained (achievement ratios between postconsolidation results and simulated results: gonial angle, 106% and 103.9%; mandibular body length, 94.2% and 89.9%; ramus height, 104.1% and 94.5% [values of the right and left sides, respectively]). The chin-point deviation and the transverse cant of the maxillary occlusal plane were significantly improved (10.1 mm to 3.3 mm; −6.8° to −4.4°). At 53 months of follow-up, the Class I molar relationship was well maintained. The transverse cant of the maxillary occlusal plane was slightly improved to −3.7° during pubertal growth.
Conclusions
Three-dimensional virtual-surgery simulation can help clinicians to determine the optimal vector and amount of distraction with high accuracy in complex cases requiring simultaneous correction of a hypoplastic mandible and facial asymmetry.
Highlights
- •
A growing boy had mandibular hypoplasia and facial asymmetry caused by previous trauma.
- •
3D virtual-surgery simulation was used to plan treatment.
- •
Treatment included asymmetric bilateral mandibular distraction osteogenesis.
- •
Class I molar relationship maxillary occlusal plane cant was maintained during growth.
- •
3D simulation helped plan complex treatment.
Condylar fracture in early childhood usually produces several complications including mandibular hypoplasia, facial asymmetry, transverse cant of the occlusal plane, temporomandibular disorder, temporomandibular joint ankylosis, mouth opening limitation, or anterior open bite. If the fracture occurs on both mandibular condyles, more severe complications can develop, especially in terms of mandibular hypoplasia, facial asymmetry, and transverse cant of the occlusal plane.
Mandibular distraction osteogenesis (MDO) has had successful outcomes in the management of patients with micrognathia since its introduction by McCarthy et al in 1992. MDO has the following advantages over traditional mandibular osteotomies. (1) In MDO, the need for a bone graft and its associated donor site morbidity diminish. (2) MDO can be performed in patients who are not candidates for mandibular osteotomy because of the developing tooth buds and inadequate bone quality and quantity. (3) Three-dimensional (3D) repositioning of the mandible is feasible with MDO.
In patients with bilateral condylar fractures, asymmetric bilateral MDO (ABMDO) can be applied to correct mandibular hypoplasia and facial asymmetry at the same time, and to alleviate the impairment of the maxillary dentoalveolar growth, which is the consequence of a deficit in mandibular vertical growth. However, precise control of the vector and the amount of ABMDO has been a challenging task for both orthodontists and surgeons. If the accuracy of prediction in ABMDO cannot be guaranteed in the 3D coordinates, every effort to restore skeletal imbalance may end in failure. Precise treatment planning using 3D virtual-surgery (3D-VS) simulation is fundamental for a successful outcome.
The purpose of this article was to report a patient with mandibular hypoplasia and facial asymmetry induced by bilateral condylar fractures in early childhood and treated with 3D-VS simulation-assisted ABMDO.
Diagnosis and etiology
A boy (age, 9.5 years) complained about the undergrowth of his face on the left side ( Fig 1 ). He had a history of fractures in both condyles and left ramus of the mandible at 4 years of age. Closed and open reductions with internal semirigid fixation were conducted for his fractured right and left condyles, respectively. However, a condylectomy had to be done on his left condyle because of osteomyelitis. During subsequent growth, there was worsening of the transverse cant of the maxillary occlusal plane and the chin-point deviation to the left side where the condyle was removed. When the patient visited the clinic, he had a retrognathic mandible, facial asymmetry, a transverse cant of the lip and maxillary occlusal plane, and dental midline discrepancies between the maxilla and the mandible.

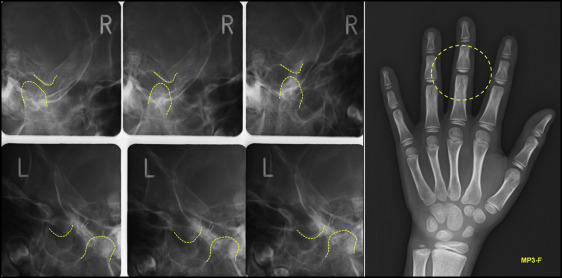
The panoramic radiograph showed a malformed condylar head and a short ascending ramus on his left side ( Fig 2 ). Compensatory growth of the left mandibular body had caused the mandibular dental midline to shift to the right side. The dentoalveolar growth of the maxilla was confined by the impeded vertical growth of the mandible, and this feature was more apparent on the left side compared with the right side. Although the amount of maximum mouth opening was within normal limits, condylar movements were significantly restricted on both sides during mouth opening ( Fig 3 ). The hand-wrist maturation stage of the patient was before the pubertal growth peak ( Fig 3 ).

Treatment objectives
The treatment objectives were (1) to improve the facial harmony by correcting the mandibular hypoplasia, facial asymmetry, and the transverse cant of the maxillary occlusal plane; (2) to resolve the confined vertical growth of the maxilla; (3) to guide the distal segment of the mandible into the planned position and stabilize the occlusion; and (4) to obtain normal overjet and overbite, along with a Class I molar relationship.
The treatment regimen consisted of preoperative orthodontic treatment, ABMDO, and active postoperative orthodontic and orthopedic treatment.
Treatment objectives
The treatment objectives were (1) to improve the facial harmony by correcting the mandibular hypoplasia, facial asymmetry, and the transverse cant of the maxillary occlusal plane; (2) to resolve the confined vertical growth of the maxilla; (3) to guide the distal segment of the mandible into the planned position and stabilize the occlusion; and (4) to obtain normal overjet and overbite, along with a Class I molar relationship.
The treatment regimen consisted of preoperative orthodontic treatment, ABMDO, and active postoperative orthodontic and orthopedic treatment.
Treatment alternatives
A unilateral functional appliance could be considered. However, this approach was not adequate for a patient with severe skeletal discrepancies, as in this case. That appliance, even with its best performance, would not fully restore his facial harmony.
Wait and see until the completion of the growth when orthognathic surgery could be performed was a possible option, but the psychosocial impairment would remain ignored until the surgical intervention.
Another alternative was the combination of an immediate LeFort l osteotomy and fixation of the maxilla for cant correction of the maxillary occlusal plane and bilateral distraction osteogenesis of the mandible for correction of the mandibular hypoplasia and the chin-point deviation. However, developing tooth buds of the maxillary posterior teeth made this treatment regimen unrealistic.
After all treatment options were discussed, the patient and his parents decided to have ABMDO.
Treatment progress
For the preoperative orthodontic treatment, fixed appliance therapy was initiated for dental decompensation, establishment of adequate transverse arch coordination, and elimination of probable interferences during the ABMDO. After 19 months of preoperative orthodontic treatment, the transpalatal arch and the lingual arch were cemented in the maxillary and mandibular dental arches, respectively ( Figs 4 and 5 ). The roles of these appliances were to maintain the transverse arch coordination and to prevent an excessive lateral shift of the distal segment of the mandible during the transarch and interarch elastics.
Surgical treatment planning for the ABMDO was as follows: (1) evaluation of the preoperative diagnostic records, (2) 3D evaluation of mandibular morphology, (3) 3D-VS simulation of distraction, (4) determination of the optimal vector and amount of distraction, and (5) trial application of distraction devices to a rapid prototyping model.
Three-dimensional computed tomogram data were used to measure ramus height, mandibular body length, and gonial angle on the right and left sides ( Figs 6-8 ; Table I ). The mandibular body length was deficient on both sides, and the ramus height was noticeably decreased on the left side compared with ethnic norm values.
| Variable | Ethnic norm (Hellman, lllB) |
Before distraction | After 3D-VS simulation | After consolidation | Achievement ratio (%) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Right side | Left side | Right side | Left side | Right side | Left side | Right side | Left side | ||
| Gonial angle (°) | 127.4 | 129.8 | 135.8 | 130.0 | 129.7 | 137.8 | 134.7 | 106 | 103.9 |
| Mandibular body length (Go-Me, mm) | 69.5 | 65.7 | 63.6 | 75.9 | 75.1 | 71.5 | 67.5 | 94.2 | 89.9 |
| Ramus height (Co-Go, mm) | 41.6 | 50.3 | 31.1 | 50.8 | 49.1 | 52.9 | 46.4 | 104.1 | 94.5 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


