The vitamins
Publisher Summary
Evidence for the existence of accessory food factors, later to be known as vitamins was obtained from the study of deficiency diseases such as scurvy, beriberi, pellagra, and rickets, which were suspected to be of dietary origin, and also from experiments in which highly purified diets were fed to rats and mice. From these two independent lines of investigation, the idea emerged that natural foodstuffs contain small quantities of substances, other than proteins, carbohydrates, fats, and minerals that are essential for normal growth and health. This chapter describes vitamin as an organic substance present in natural foodstuffs that the body requires in very small amounts but is not able to make for itself in sufficient quantity. This rather clumsy definition is necessary to cover what is now known about this very varied collection of nutrients. From the dietary point of view, the vitamins may be divided into major and minor vitamins. Lack of any of the major vitamins, which include vitamins A, D, and C and three or four members of the vitamin B complex, leads to a recognizable deficiency disease. The requirement for the remaining vitamins is much less; they are very widely distributed, and many of them are synthesized by microorganisms that inhabit the gut so that deficiency rarely occurs. A vitamin may be an essential dietary constituent for one animal species but unnecessary for another. In certain instances, the body may have a limited ability to synthesize a particular vitamin but be unable to meet its requirements in all circumstances.
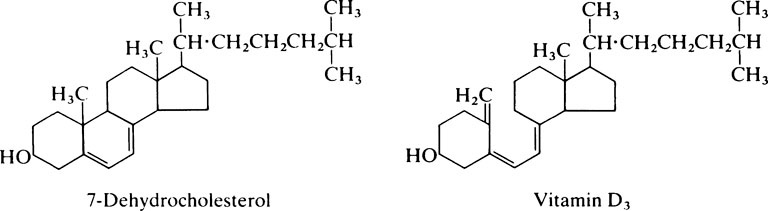
Evidence for the existence of ‘accessory food factors’, later to be known as ‘vitamins’, was obtained from the study of deficiency diseases such as scurvy, beriberi, pellagra and rickets, which were suspected to be of dietary origin, and also from experiments in which highly purified diets were fed to rats and mice. From these two independent lines of investigation the idea emerged that natural foodstuffs contain small quantities of substances, other than proteins, carbohydrates, fats and minerals, that are essential for normal growth and health. The nature of these substances was unknown, but that there was more than one was soon recognized because both fat-soluble and water-soluble factors were required. Initially the vitamins were designated by letters of the alphabet but as their structure and functions were determined most of them were given specific names. However, since in various instances several closely related compounds have similar biological effects, it is convenient to use a generic term for a group of substances, e.g. vitamin D to include both cholecalciferol and ergocalciferol (page 156).
The fat-soluble vitamins
Vitamin A – retinol
Vitamin A deficiency
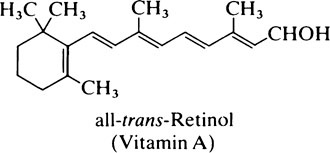
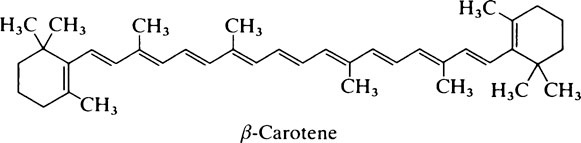
Apart from its specific function in the visual process (page 155), vitamin A is needed for growth, reproduction and the maintenance of the integrity of epithelial cells. Since retinol is stored in the liver, signs of its deficiency develop very slowly. In Man the earliest noticeable effect is night-blindness, i.e. the inability to see in dim light, and this is readily cured by administration of the vitamin. Later, xerophthalmia develops, the eyes become dry and susceptible to infection and the conjunctiva and cornea become keratinized. This is followed by keratomalacia or softening of the cornea which leads to permanent blindness. Even today vitamin A deficiency is the commonest cause of blindness in Africa, India and the Far East in spite of the fact that carotene can be obtained from green leaves, maize and other vegetables. Carotene is poorly absorbed even in normal subjects and, where nutrition is inadequate, not only may the diet be deficient in fat but the gastrointestinal tract may be abnormal so that the fat-soluble vitamins are very poorly absorbed.
Cellular effects
From the effects of its deficiency it appears that vitamin A is required for the controlled division and differentiation of cells. Retinol is delivered to specific sites on the cell surface that recognize the RBP and cause it to release the retinol. Once inside the cell the retinol combines with the cellular retinol-binding protein and retinoic acid with cellular retinoic acid-binding protein and each is delivered to nuclear binding sites which may be important in gene expression. Thus their mode of action resembles that of the steroid hormones (page 349).
Apart from effects on the nucleus, retinol has been found to have a stabilizing effect on cell membranes. More specifically retinol seems to take part in glycosyl-transfer reactions and the synthesis of various glycoconjugates (page 407). Effects on cell surface components may mediate changes in intracellular recognition and interactions and also in the process of cell adhesion and aggregation.
Vitamin A and vision
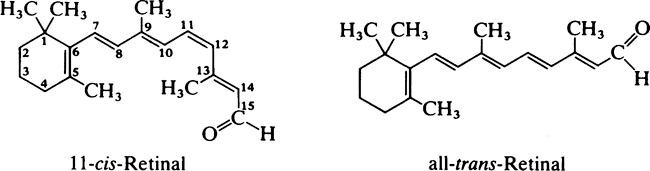
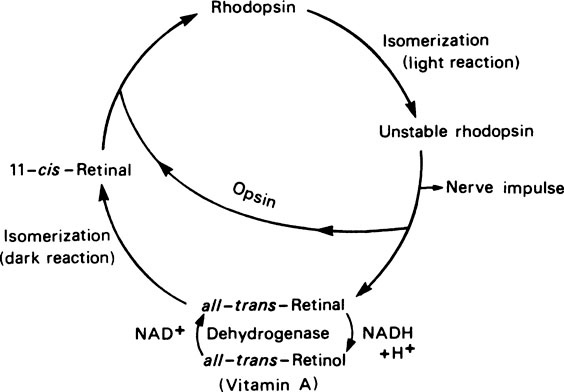
retina to nerve impulses, the cis-retinal undergoes a molecular rearrangement to form all-trans-retinal which is more stable. This change in configuration causes the rhodopsin to dissociate into its constituents, opsin and all-trans-retinal. Rhodopsin can then only be regenerated after the retinal has been rearranged to the 11-cis form and this can only occur in dim light. Reutilization of the retinal is never complete since an appreciable fraction of the all-trans-retinal is reduced to retinol by alcohol dehydro-genase and NADH and some may be lost into the blood. The visual cycle is shown in Figure 12.1.
Vitamin E – the tocopherols
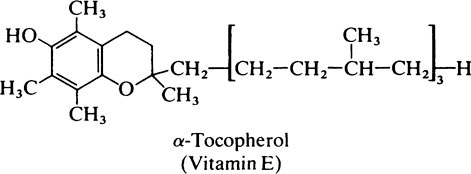
the absence of apoprotein B. Under such circumstances the serum tocopherol level falls and the fragility of the red blood corpuscle membrane is increased. Vitamin E deficiency also occurs in premature and low-birth-weight babies in which it may be responsible for haemolytic normocytic anaemia, blindness and intraventricular haemorrhage.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses