Local anesthetics are commonly used in both dentistry and medicine. These drugs are also used in some office-based medical practices. Except for minor procedures, most physicians who require complicated nerve blocks rely on anesthesiologists to administer the local anesthesia. Both ester and amide local anesthetics are routinely used in medical practice. This article reviews the types and uses of local anesthesia in anesthesiology.
Local anesthetics are commonly used in both dentistry and medicine. These drugs are similarly used in some office-based medical practices. For example, in dermatology local infiltration, which dentists commonly use in the maxilla, is provided for minor surgical procedures such as excisional biopsy of skin lesions. In ophthalmology a retrobulbar nerve block, similar to what a dentist would commonly provide for mandibular anesthesia, is used for local anesthesia of the globe. These are but 2 examples of minor medical procedures that can be performed by office-based physicians.
Anesthesiologists can also provide regional anesthesia for most surgical procedures, although for various reasons the use of general anesthesia is frequently preferred. Peripheral surgical procedures, such as many upper and lower extremity procedures, some head and neck surgery, and superficial abdominal procedures (eg, inguinal hernia) can be easily completed with local anesthesia with or without sedation. Even some major abdominal surgeries can be performed with the use of neuraxial anesthesia, such as local anesthesia applied around the spinal cord or epidural space. As opposed to anesthesiologist practice, the typical doses of local anesthetic administered for dental procedures are usually well below the levels associated with toxicity issues, such as altered consciousness, seizures, or unconsciousness. However, many of the regional anesthesia techniques discussed here require larger volumes of local anesthetic (up to 40–50 mL), far exceeding the volumes usually used in dentistry. As expected, toxicity complications are more common, requiring close monitoring during administration; rapid recognition of overdose symptoms; and prompt treatment, including immediate endotracheal intubation and advanced supportive measures, when indicated. Except for minor procedures, most physicians who require complicated nerve blocks rely on anesthesiologists to administer the local anesthesia, usually in combination with some form of sedation, and at times, general anesthesia in the hospital operating room or ambulatory surgery center setting.
This article reviews the types and uses of local anesthesia in anesthesiology.
Local anesthetics used in medicine
Both ester and amide local anesthetics are routinely used in medical practice ( Table 1 ). The general pharmacology of these agents has been reviewed in the introductory article “Local anesthetics: pharmacology and toxicology” in this issue by Moore and Hersh. By far the most commonly used agents in office-based medical practice are the amides, specifically lidocaine (Xylocaine) and bupivacaine (Marcaine) with or without epinephrine. Examples of the commonly used ester local anesthetics include benzocaine (Hurricaine, Cetacaine), cocaine, procaine (Novocaine), chloroprocaine, and tetracaine (see Table 1 ). Some unique aspects of local anesthesia as used in medical practice are reviewed here.
| Agent | pKa | % Total Drug in Base Form at pH 7.4 | Onset | Duration | Class |
|---|---|---|---|---|---|
| Benzocaine | 3.5 | 100 | Fast | Short | Ester |
| Mepivacaine | 7.6 | 39 | Fast | Moderate | Amide |
| Lidocaine | 7.9 | 24 | Fast | Moderate | Amide |
| Etidocaine | 7.7 | 33 | Fast | Long | Amide |
| Bupivacaine | 8.1 | 17 | Slow | Long | Amide |
| Tetracaine | 8.6 | 14 | Slow | Long | Ester |
| Procaine | 8.9 | 3 | Slow | Short | Ester |
| Chloroprocaine | 9.1 | 2 | Slow | Short | Ester |
Ester Local Anesthetics
The benzocaine molecule is very insoluble in water, and as such is indicated for topical applications in a spray or gel form. Benzocaine is used to provide topical anesthesia for a limited duration to nasal, oral, or orotracheal mucosa. One preparation in particular, Cetacaine, is a mixture that includes benzocaine, tetracaine, and butyl aminobenzoate (Butamben), which is an additional lipophilic ester local anesthetic. Cetacaine spray has historically been used to provide topical anesthesia to the oronasopharyngeal mucosa for procedures such as esophagogastroduodenoscopy, bronchoscopy, or “awake” endotracheal intubation, in which endoscopes are passed into the esophagus or trachea through the mouth or nose. However, Cetacaine, a topical anesthetic containing tetracaine, benzocaine, and butyl aminobenzoate, can cause methemoglobinemia, especially if administered in large quantities, which can occur with these procedures.
Cocaine, which was the first local anesthetic to be discovered, is still occasionally used clinically. However, it is restricted to topical use only, most commonly administered as a 10% solution delivered with cotton pledgets, usually before nasal surgery or nasal endotracheal intubations. Because cocaine is the only local anesthetic with intrinsic vasoconstrictor properties, it would seem to be an ideal agent for this purpose. However, despite cocaine being a potent local anesthetic, its rare usage is most likely attributed to the high potential for complications involving the cardiovascular and sympathetic nervous systems. Systemically, cocaine inhibits the reuptake of norepinephrine, which causes stimulation of the sympathetic nervous system. In addition, cocaine sensitizes the myocardial cells to stimulation from norepinephrine or epinephrine release. Of particular concern are the cardiovascular side effects if administered concurrently with nonselective β-blockers. Use of nonselective β-blockers in conjunction with cocaine can lead to an unopposed alpha response, leading to hypertensive emergency.
Procaine is still occasionally used for spinal block or skin infiltration when a very short duration of action is preferred. Another commonly used ester is chloroprocaine, which has a rapid onset and low toxicity, making it an ideal drug for administration during labor and delivery for infiltration or more commonly via an epidural. It can also be administered for peripheral nerve blocks. Chloroprocaine is often avoided during spinal (intrathecal) injections because of reports of neural complications, including prolonged sensory and motor deficits, particularly when sodium metabisulfite is used as an antioxidant.
Tetracaine is the most commonly used ester local anesthetic administered for spinal blocks. When placed intrathecally, tetracaine has a rapid onset and produces a dense neural blockade. Used in conjunction with epinephrine, spinal blocks can last for 4 to 6 hours. Tetracaine is also supplied as a topical spray, often used to anesthetize the upper airway to help the patient tolerate naso-oropharyngeal endoscopic procedures. However, because of its rapid uptake, excessive topical use can lead to toxic reactions such as methemoglobinemia.
Amide Local Anesthetics
As in dentistry, amides are the most commonly used local anesthetics. In addition to lidocaine, mepivacaine (Carbocaine) and bupivacaine (Marcaine), all used in dentistry, ropivacaine (Naropin) and levobupivacaine (Chirocaine) are also used. In this section, when applicable, differences in uses or preparations in medical versus dental practice are highlighted.
Lidocaine has a rapid onset along with moderate potency and duration of action. Along with bupivacaine, it is the most commonly used local anesthetic. Whereas a 2% solution is the only available concentration in dental cartridges, single-dose and multidose vials are supplied in 0.5% to 4% solutions with or without epinephrine. In fact, 0.5% or 1% solutions are mostly used in medicine.
Although routinely administered for infiltration anesthesia and peripheral nerve blocks, within the last 20 years lidocaine has fallen out of favor with anesthesiologists for spinal blocks after multiple reports of complications involving lower back pain. Initially thought to be related to the use of highly concentrated lidocaine solutions, reports persisted of lower back pain lasting approximately 2 days, despite trials with lower concentrations of lidocaine.
Mepivacaine has a very similar clinical profile when compared with lidocaine. When administered in the epidural space, it provides a slightly longer duration of action. It is also frequently combined with longer-acting local anesthetics such as bupivacaine or ropivacaine during peripheral nerve blocks. This combination provides a quick-onset anesthetic that also has the benefits of a prolonged duration.
Bupivacaine, because of its higher log dissociation constant (pKa) of 8.1, has a somewhat slower onset than lidocaine. Its more prolonged duration of action is due to its increased lipophilicity and greater protein-binding properties. These properties make it a useful local anesthetic when delivered via peripheral and neuraxial blocks. Many clinicians believe that it is more predictable than tetracaine when administered for intrathecal or spinal blocks. Because of its slow onset of action, it is often used concurrently with a local anesthetic that has a more rapid onset when administered for peripheral nerve blocks. Of special concern is the cardiotoxicity of bupivacaine. If accidentally administered intravascularly, bupivacaine can cause cardiac dysrhythmias and ultimately, cardiovascular collapse. This potentially life-threatening complication can only be treated with prompt intravenous administration of intralipid, a fat emulsion, which acts as a bupivacaine sink, causing a rapid decrease in bupivacaine concentration in the blood plasma. Levobupivacaine, the S -enantiomer of bupivacaine, is reported to have decreased cardiac and central nervous system toxicity.
Ropivacaine is a local anesthetic that is popular for use during peripheral nerve blocks because of the extended clinical half-life in addition to a predilection for sensory over motor nerves. However, it does not share the cardiac toxicity profile that is unique to bupivacaine. As such, clinicians often use ropivacaine for peripheral nerve blocks, especially if larger doses are needed to cover multiple areas.
Etidocaine has a long duration of action similar to that of bupivacaine. However, because its lower pKa is closer to physiologic pH, the onset of anesthesia is noticeably quicker. Also, etidocaine produces a denser motor blockade than bupivacaine, which can be beneficial if skeletal muscle relaxation is desired in addition to anesthesia.
Local anesthesia techniques in medicine
Primary Surgical Anesthesia
As in dentistry, infiltration and localized peripheral nerve blocks are the more common techniques for administration of local anesthetics in medicine. Nerve block techniques are often used as the sole anesthetic technique in the medicine for a large variety of surgical procedures, just as in dentistry. Nerve blocks serve as a useful alternative for patients who would otherwise be at a higher risk for complications of general anesthesia because of complex medical conditions. For example, a patient requiring an incision and drainage of an infected ankle fracture who has a compromised cardiac history may be at an increased risk for further cardiopulmonary complications if the surgery is performed under general anesthesia. The placement of a nerve block, with or without sedation, not only lowers the potential risk for additional systemic complications but also provides the patient and surgeon with a comfortable, reliable, high-quality anesthetic experience.
Infiltration Anesthesia
Similar to maxillary infiltration techniques used in dentistry, local anesthetics are delivered subcutaneously and allowed to diffuse into the surrounding tissue. This method provides adequate anesthesia for the overlying skin and subcutaneous structures. With the use of a longer needle and injecting while simultaneously withdrawing the needle, local anesthetic coverage to a larger area or field is achieved. Infiltration or field blocks are used frequently during carpal tunnel surgeries to anesthetize the nerves of the wrist or during ankle procedures to block the nerves of the ankle. Although useful, field blocks often require larger volumes of local anesthetic, especially if vasoconstrictors are not added.
Major regional nerve blocks
Regional nerve blocks are conceptually identical to the various nerve blocks used in dentistry, but larger nerves covering broader areas are targeted. For example, by delivering local anesthetic to the main nerve branches innervating the extremities, it is possible to provide adequate anesthesia to allow a patient to undergo an invasive arm or leg surgical procedure without any intraoperative pain. Anesthesiologists almost exclusively provide major regional anesthesia, and have additional equipment at their disposal that helps identify anatomic relationships and direct needle placement. These techniques include the use of electronic nerve stimulators, portable ultrasound machines, and even fluoroscopy. An electronic nerve stimulator emits small electrical stimuli that can elicit motor or sensory responses when delivered in the proximity of a nerve. By attaching the nerve stimulator to a special needle, anesthesiologists watch for a motor response and are then able to amplify that response by directing the needle closer to the nerve. Once the motor response is maximized, the local anesthetic is delivered through the needle, right at the level of the targeted nerve. This procedure helps to eliminate problems associated with missed blocks. Portable ultrasound machines are now used to visualize the anatomic structures so that the needle can be guided directly toward the targeted neural structures. Ultrasound machines are even capable of visualizing vascular structures, which helps reduce the likelihood of an intravascular injection. Similarly, the use of fluoroscopy, a conventional x-ray unit that relays immediate information from both static and moving images, allows for real-time visualization of both soft and hard tissue. With this technique, it is possible to inject medications directly at the level of specific nerve roots as they exit the spinal column with visualization of the needle and surrounding tissue simultaneously.
Specific regional nerve blocks: upper extremities
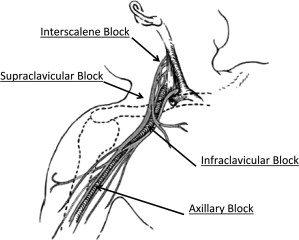
The main innervations of the upper extremities all arise from levels C5–C8 and T1. These nerves coalesce to form the brachial plexus shortly after exiting the intervertebral foramina. After intermingling within the brachial plexus, they extend distally to provide motor and sensory innervation to the shoulder, upper arm, forearm, and hand. There are several techniques that are used to provide anesthesia via deposition of local anesthetic along the distribution of the brachial plexus nerves. From the proximal aspect of the brachial plexus distally, the techniques include interscalene, supraclavicular, infraclavicular, axillary, and digit blocks ( Fig. 1 ). Selection of the type of upper extremity block depends on what dermatomes or areas of the arm are involved in the surgery. As expected, deposition of local anesthetic at each specific nerve will provide anesthesia to all areas innervated distally from that site of injection. Upper extremity nerve blocks are easily placed; are usually fairly well tolerated by patients, requiring minimal sedation for comfort; and have a fairly low complication rate when performed by trained personnel, such as an anesthesiologist.