Aim
The aim of this study was to evaluate the upper airway changes after simultaneous maxillary advancement/impaction and mandibular setback in skeletal Class III malocclusion.
Methods
The subjects included 76 patients whose treatment included 1-piece LeFort I and bilateral sagittal split osteotomies. Lateral cephalograms were taken before surgery and 2 months and 3 years postoperatively. In order to analyze the effect of maxillary repositioning, the material was divided into subgroups according to whether the maxillary impaction and advancement were clinically significant (≥2 mm) or not.
Results
Advancement of the maxilla with or without impaction resulted in a significant long-term increase ( P <0.001) in airway dimension at the nasopharyngeal level (13%–21% increase). At the oropharyngeal and retrolingual levels, a decrease took place but was significant ( P <0.05) only at the oropharyngeal level when the maxilla was not impacted. When the maxilla was not advanced, there was no significant change, except at the hypopharyngeal level (12% decrease) ( P <0.01).
Conclusions
Clinically significant advancement (≥2 mm) of the maxilla significantly increased the airway dimension at the nasopharyngeal level and to some extent compensated for the effect of mandibular setback at the hypopharyngeal level.
Over the last 2 decades, changes in upper airway dimensions after various orthognathic osteotomies, as well as their capacity to induce or resolve obstructive sleep apnea (OSA) syndrome, have been addressed by several investigators. A number of reports have documented a decrease of the upper airways after isolated mandibular setback. Maxillary advancement may, in contrast, increase nasopharyngeal airways after advancement in cleft patients, and Greco et al observed an increase of the nasopharyngeal as well as the hypopharyngeal airway space after advancement of the maxilla.
Maxillary advancement in combination with forward posturing of the mandible has been used as a treatment approach for OSA over the last decades. Maxillomandibular advancement has a potential to enlarge the upper airways not only in anteroposterior dimension but also in transverse width. The precise effect on pharyngeal morphology after maxillary advancement has not been clarified. Conradt et al identified insufficient maxillary advancement as a reason for unsuccessful resolution of sleep disorders.
It may be assumed that bimaxillary surgery for Class III correction as an alternative to isolated mandibular setback could represent less risk for restriction of the upper airways because a lesser amount of mandibular setback would be needed; hence, more space for the tongue would become available. Some studies comparing effects of isolated mandibular setback versus bimaxillary surgery have indicated less decrease in the posterior airway space after bimaxillary procedures. So far, however, most studies of upper airway changes after bimaxillary surgery have reported significant reduction of the upper airways. Marsan et al observed an increase in the retropalatal space after correction of Class III malocclusion by maxillary advancement and impaction in addition to mandibular setback in females.
Previous studies of isolated mandibular surgery have shown that reduction of the upper airways correlated with the amount of mandibular setback. Even if comprehensive information on the impact of mandibular setback to the upper airways is available, studies assessing the influence of simultaneous maxillary repositioning are scant. A challenge in the planning of orthognathic surgery is to balance concerns related to facial esthetics and airway changes. Therefore, more detailed information about the effects of maxillary movements during bimaxillary Class III surgery is needed.
The present study represents an attempt to investigate the effect of maxillary advancement and/or impaction on upper airway dimensions in patients undergoing bimaxillary surgery for correction of skeletal Class III malocclusion.
Material and methods
The initial sample of this study comprised 84 patients who were operated on consecutively and underwent a combination of 1-piece LeFort I and bilateral sagittal split osteotomies with rigid fixation. Lateral cephalometric radiographs were selected from the files at the Department of Orthodontics, University of Oslo. Surgery had been performed at the Ullevaal University Hospital, Oslo between 1990 and 2003. The follow-up period was 3 years. Patients with syndromes, cleft of the lip and/or palate, or dentofacial trauma were excluded from the study. Records of the patients were collected 1 week prior to surgery (T1) and at 5 different follow-up examinations: 1 week, 2 months, 6 months, 1 year, and 3 years. In the present study, only the follow-up records at 2 months (T2) and 3 years (T3) were used for assessment of changes in airway space. From the initial sample, 6 subjects were excluded because of missing radiographs at T2 or T3, and another 2 patients were excluded because the pharyngeal structures were blurred or had unclear borders. The final sample thus consisted of 76 patients (50 male and 26 female). The age at time of surgery varied from 15.7 to 49.2 years, with a mean of 24.3 years (SD 7.3 years).
The same cephalostat was used for all radiographs, and the cephalograms were taken with the head in a standardized position with the teeth in occlusion and the lips relaxed. No instructions were given to patients regarding swallowing during the procedure. All cephalograms were hand traced by the same examiner (G.J.) on acetate paper. The cephalogram of the best quality was traced first, and then tracings of the other radiographs were superimposed on sella (S), nasion (N), and anterior and posterior cranial base using the “best-fit” method. The tracings were scanned and digitized with the Dentofacial Planner Plus software (Dentofacial Software, Toronto, Canada) on a computer with a digitizing screen (Numonics Cooperation, Montgomeryville, Pa). The measurements were not corrected for magnification (5.6%). Skeletal changes were recorded using a coordinate system: the x-axis was drawn through S at an angle of 7° down from S-N line, and the y-axis was constructed perpendicular to the x-axis through S.
The following landmarks were identified in the upper airways ( Fig 1 ):
| PNS: | Posterior nasal spine |
| U: | Tip of the uvula, the most posteroinferior point of the uvula |
| V: | Vallecula, the intersection of epiglottis and the base of the tongue |
| UPW: | Upper pharyngeal wall, intersection of the PNS–Ba (basion) line and the posterior pharyngeal wall |
| MPW: | Middle pharyngeal wall, intersection of a perpendicular line from U with the posterior pharyngeal wall |
| LPW: | Lower pharyngeal wall, intersection of a perpendicular line from V with the posterior pharyngeal wall |
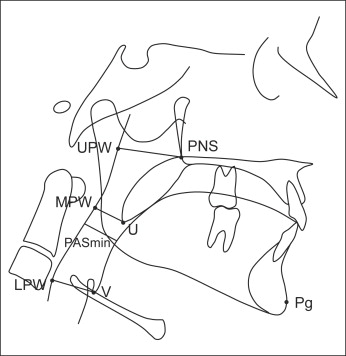
Posterior airway space (PAS) was measured by the following linear distances:
| PNS-UPW: | The distance from PNS to UPW, representing the nasopharyngeal airway space |
| U-MPW: | The distance from U to MPW, representing the oropharyngeal airway space |
| V-LPW: | The distance from V to LPW, representing the hypopharyngeal airway space |
| PASmin: | The minimal distance between the base of tongue and the posterior pharyngeal wall, representing the minimal pharyngeal (retrolingual) airway space |
In order to evaluate the effect of varying repositioning of the maxilla on airway dimensions, the patients were divided in 4 subgroups according to whether horizontal and/or vertical movement of the maxilla at PNS during surgery was clinically significant (≥2 mm) or not:
-
Group 1. Maxillary advancement ≥2 mm and impaction ≥2 mm (n = 24)
-
Group 2. Maxillary advancement ≥2 mm and impaction <2 mm (n = 29)
-
Group 3. Maxillary impaction ≥2 mm and advancement <2 mm (n = 9)
-
Group 4. Maxillary advancement and impaction <2 mm (n = 14).
Surgical repositioning of the jaws is presented in Table I .
| Maxillary advancement and impaction (n = 24) (Group 1) |
Maxillary advancement (n = 29) (Group 2) |
Maxillary impaction (n = 9) (Group 3) |
No maxillary advancement or impaction (n = 14) (Group 4) |
|
|---|---|---|---|---|
| PNS horizontal | 5.0 (2.5) | 4.7 (2.0) | 0.4 (1.1) | 0.3 (1.4) |
| PNS vertical | −4.5 (2.4) | 0.1 (1.2) | −4.0 (2.1) | 0.6 (1.7) |
| Pg horizontal | −5.5 (7.7) | −5.4 (6.2) | −6.6 (7.8) | −6.6 (5.7) |
| Me vertical | −3.6 (4.6) | −1.4 (3.1) | −3.6 (5.6) | −0.7 (5.0) |
For analysis of method error, 20 radiographs, chosen at random, were traced and digitized by the same investigator on 2 separate occasions at least 2 weeks apart. Statistical analyses were performed with SPSS for Windows software (SPSS, Chicago, Ill). The data were tested for normality of distribution. Paired t tests were used to analyze changes in the cephalometric variables over time. Differences between subgroups were tested with the analysis of variance (ANOVA) test.
Results
The method error ranged from 0.36 mm to 0.68 mm for linear measurements (Dahlberg calculation), and the intraclass correlation coefficient (ICC) ranged from 0.951 to 0.990.
Mean changes in the position of the maxilla and the mandible during surgery (T1 to T2) are presented in Table I . The ANOVA test did not detect differences among the groups for the horizontal (Pg) and vertical (Me) changes of the mandible. There were no statistically significant differences between groups 1 and 2 nor between groups 3 and 4 with respect to horizontal surgical changes at PNS. Likewise, groups 1 and 3, as well as groups 2 and 4 were similar regarding the vertical movements at PNS. Short- and long-term mean changes in the airway space dimensions are presented in Tables II to V .
| T1 | T2 | T3 | Change T1–T2 |
P value | Change T1–T3 |
P value | |
|---|---|---|---|---|---|---|---|
| PNS-UPW | 22.0 (5.1) | 25.6 (5.1) | 24.9 (5.0) | 3.7 (2.4) | 0.000 | 3.0 (2.4) | 0.000 |
| U-MPW | 12.1 (3.2) | 12.1 (2.8) | 11.5 (3.7) | −0.1 (2.9) | 0.922 | −0.9 (2.3) | 0.091 |
| V-LPW | 19.3 (3.4) | 19.3 (3.5) | 19.5 (3.3) | 0.0 (2.8) | 0.948 | 0.3 (3.2) | 0.703 |
| PASmin | 11.3 (3.5) | 11.5 (3.4) | 10.6 (3.8) | 0.2 (3.2) | 0.654 | −0.8 (3.1) | 0.230 |
| T1 | T2 | T3 | Change T1–T2 |
P value | Change T1–T3 |
P value | |
|---|---|---|---|---|---|---|---|
| PNS-UPW | 21.6 (4.9) | 27.0 (5.5) | 26.1 (5.7) | 5.4 (2.7) | 0.000 | 4.4 (3.4) | 0.000 |
| U-MPW | 14.6 (4.9) | 13.7 (4.2) | 13.3 (4.6) | −1.0 (2.6) | 0.058 | −1.3 (3.0) | 0.025 |
| V-LPW | 19.4 (4.0) | 18.8 (3.5) | 19.7 (3.2) | −0.6 (3.5) | 0.385 | 0.2 (3.5) | 0.748 |
| PASmin | 12.9 (3.6) | 12.1 (3.6) | 12.2 (3.7) | −0.8 (3.6) | 0.268 | −0.7 (3.7) | 0.308 |
| T1 | T2 | T3 | Change T1–T2 |
P value | Change T1–T3 |
P value | |
|---|---|---|---|---|---|---|---|
| PNS-UPW | 22.0 (3.8) | 22.3 (3.4) | 22.8 (4.4) | −0.7 (1.9) | 0.279 | −0.2 (3.3) | 0.828 |
| U-MPW | 12.8 (2.5) | 11.6 (3.8) | 12.3 (3.3) | −1.1 (2.5) | 0.211 | −0.4 (2.3) | 0.591 |
| V-LPW | 20.0 (4.4) | 19.0 (4.4) | 19.7 (4.4) | −1.0 (1.5) | 0.089 | −0.3 (1.9) | 0.632 |
| PASmin | 13.3 (3.2) | 11.8 (2.4) | 12.3 (4.0) | −1.4 (2.6) | 0.133 | −1.0 (1.8) | 0.142 |
| T1 | T2 | T3 | Change T1–T2 |
P value | Change T1–T3 |
P value | |
|---|---|---|---|---|---|---|---|
| PNS-UPW | 24.9 (5.0) | 26.2 (4.7) | 26.4 (5.0) | 1.3 (2.6) | 0.081 | 1.4 (2.7) | 0.064 |
| U-MPW | 13.2 (4.7) | 11.4 (3.0) | 12.0 (4.2) | −1.8 (4.0) | 0.109 | −1.1 (3.6) | 0.273 |
| V-LPW | 20.6 (3.5) | 18.6 (3.2) | 18.1 (2.9) | −2.1 (2.8) | 0.015 | −2.5 (3.1) | 0.010 |
| PASmin | 13.3 (2.4) | 11.3 (3.5) | 12.0 (3.3) | −2.0 (3.4) | 0.044 | −1.4 (2.4) | 0.054 |
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


