Fig. 6.1
Patient electronic dental record. Dentrix screenshot courtesy of Henry Schein Practice Solutions, American Fork, Utah (Reprinted with permission)
6.6 The History of Teledentistry
Telemedicine began in 1924, with the concept of a physician seeing his patient over the radio using a television screen [11]. The initial concept of teledentistry developed as part of the blueprint for dental informatics, which was drafted at a 1989 conference funded by the Westinghouse Electronics Systems Group in Baltimore [12]. The birthplace of teledentistry as a subspecialist field of telemedicine can be linked to a 1994 military project of the United States Army Total Dental Access Project aiming to improve patient care, dental education, and effectuation of the communication between dentists and dental laboratories [3, 11–13]. Teledentistry was put into practice by the U.S. Army by doing consultations on persons located more than 100 miles apart [11]. Since that time, various public health facilities, remote rural clinics, and organizations have practiced teledentistry with various degrees of success. The variation in the levels of acceptance and use of dental EHRs throughout the profession has been determined by the mode of communication preferred, type of software and hardware used, and the type of internet connection.
6.7 Methods of Communication
Teleconsultation through telehealth can take place either in “real-time” or “store-and-forward” methods [3, 11–13]. Real-time consultation involves a videoconference (see Fig. 6.2a) in which dental professionals and their patients, at different locations, may see hear, and communicate with one another actually using advanced telecommunication technology and ultra-high bandwidth network communications [11–13]. Store-and-forward (see Fig. 6.2b) refers to the collection and secure transmission of encoded information including patient documents and images (intraoral photos, radiographs, and extraoral photos) which are stored for review by a dentist or specialist at a later time for consultation and treatment planning [3, 11–13]. A third method has also been described, known as “remote monitoring method” in which patients are monitored at a distance and can either be hospitalized or home-based [12]. Since the patient is not present during the store-and-forward consultation, dentists can share patient information, radiographs, photos, and other information transportable through multiple providers [12]. This data sharing can be of extreme importance for patients in need of a specialist who may not be located nearby, patients who have been displaced by natural disasters who need treatment, and patients who may need to be monitored at a distance.
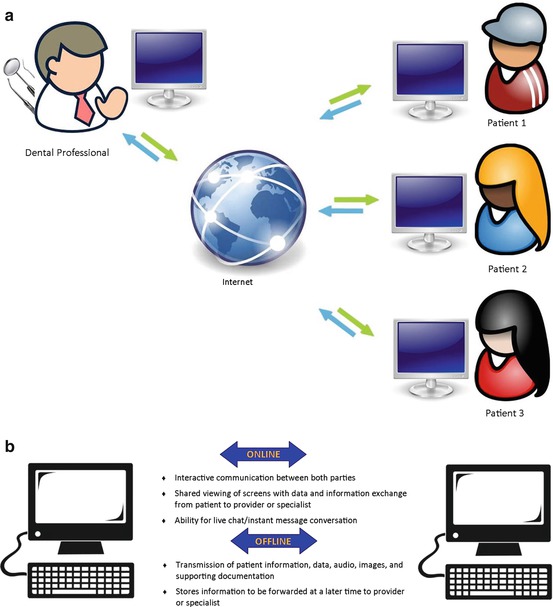
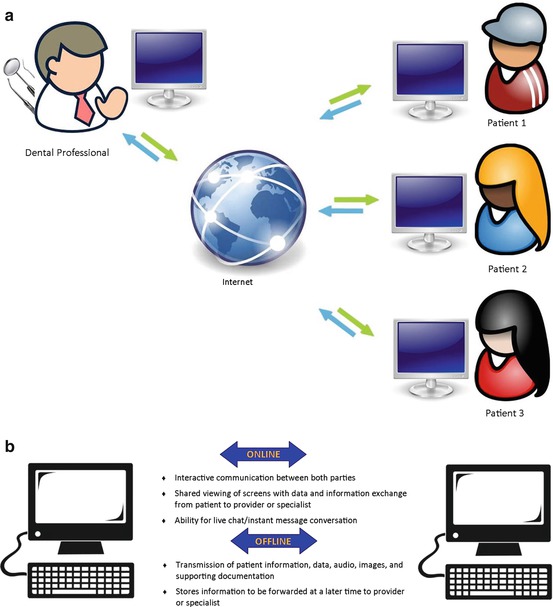
Fig. 6.2
(a) Type of teleconsultation. (b) Types of telecommunication
6.8 Technological Requirements
To practice dentistry within the realm of telehealth, a desktop or laptop computer with a microphone and substantial hard drive memory are needed. In addition, a significant amount of RAM with a speedy processor; a digital camera, video camera and intraoral camera for the capture of pictures [11, 12]; and a portable x-ray unit (NOMAD®) (see Fig. 6.3) are essential. A comprehensive software capable of image acquisition and storage, and transmission of the gathered information and software capable of coding and decoding audio and video is desirable [11]. A fax machine, scanner, and a printer may also be required in some cases [12]. There is great variation in levels of speeds to connectivity to the internet and broadband technology, increasingly widespread and available, offers a selection of cutting-edge alternatives well suited to meet the needs of the telehealth professional and his or her staff [11]. There are many advantages as well as disadvantages to using telehealth technology.


Fig. 6.3
NOMAD® handheld portable radiograph unit (Photo of actual equipment)
6.9 Advantages of Using Teledentistry
Teledentistry provides a unique way to help overcome the barriers or geography and travel time to deliver long-distance clinical training, continuing education, and hands-on training for the dentist/dental hygienist at remote clinics [11, 15]. Its application is of utmost importance and great value in rural and urban underserved areas where there is unavailability of specialist consultation which reduces the costs of service and improves quality of care [12–14]. The results of telehealth usage increase inter-professional communications which will improve dentistry’s integration into the larger health care delivery system [13]. Second opinions, pre-authorizations and other insurance requirements will be met almost instantaneously online, with the use of real images of dental problems, thereby making traditional dental care more efficient [14, 15]. In addition, it will facilitate the greater use of nondentist providers (such as dental hygienists or mid-level providers) and improve early diagnosis and treatment of oral disease [15]. For dental and dental hygiene schools, interactive video-conferencing allows for the evaluation of patient information (with or without the patient’s presence), which allows for the interaction and feedback between the educator and the students [14]. Telehealth can serve as a tool to compliment and expand the capacity of school child care centers to meet the children’s dental care needs by using technology to connect to the health providers at another location [14]. For dental facilities, there is long term cost effectiveness due to savings generated from not purchasing equipment and materials to develop traditional dental radiographs. Although Telehealth is being used nationally and internationally by educational institutions and public health facilities, still many legal, financial, and ethical concerns exist (Table 6.1).
Table 6.1
Teledentistry advantages
|
Financial
|
Social
|
Technical
|
|---|---|---|
|
Increased use of dental hygienists, advanced dental therapists, and mid-level providers
|
Delivery of dental services to remote areas
|
Second opinions, pre-authorizations, and insurance requirements met via electronic dental claims management
|
|
Increased interaction of educators and students at dental and dental hygiene schools via video-conferencing
|
Treatment of underserved rural or urban populations
|
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


