Fig. 14.1
Panorex film showing endodontic sealant in the inferior alveolar canal below the lower left first molar. If symptomatic, the material should be debrided promptly
(c)
If there was no witnessed transection, yet the patient is completely anesthetic or has quality of life-altering dysesthesia 2–3 months after injury, surgery is likely indicated.
(d)
If, after 4–6 months, the patient still does not have protective reflexes (cannot feel when hot or cold substances come in contact with the area innervated by the IAN or are in danger of biting their lip continuously), then surgery may be indicated. Protective reflexes are felt to be present when a patient has 30 % or more of normal feeling (usually measured with a combination of Von Frey’s hairs and two-point discrimination) [7].
(e)
Surgery has not been shown to be helpful at any time with injuries related to an IAN local anesthetic block [8]
(f)
Nerve repairs performed after 1 year are felt to provide poor results, but some authors have shown reasonable results with LN repairs, even after as long as 4 years post-injury [9].
14.2 Surgical Approaches to the IAN
The IAN can be approached surgically from an extraoral approach or by an intraoral approach. To a certain extent, this may depend upon surgeon preference, patient preference, and the site of the nerve injury.
Advantages of the extraoral approach are superior surgical access and visualization and, therefore, an increased opportunity to carry out an effective nerve repair. This is particularly true since a surgeon can use the operating microscope at right angles to the mandible, and also bring his/her arms in from the sides, which is the ideal position for carrying out microsurgery. The disadvantages of the extraoral approach are the obvious occurrence of a facial scar (though it is beneath the jaw line), and the possibility of facial nerve involvement, which would add to the original injury.
The intraoral approach is obviously preferable from a cosmetic point of view, but from a surgical standpoint, it is very difficult to use the operating microscope at an oblique angle to the mandible and also difficult to get one’s hands in at the same time. A long focal-length lens is necessary on the operating microscope, and a lens of at least 250 mm focal length should be utilized. Many surgeons prefer to carry out intraoral exploration and repair with surgical loupe magnification, usually in the range of four to five times magnification. As far as the actual approach to the IAN is concerned, a number of possible approaches have been described including the following:
1.
A block decortication of the mandible [10]. This is the author’s personal preference since it does allow isolation and visualization of the IAN over a long portion of its length, allowing visualization of any neuromas, and appropriate mobilization of the nerve to carry out any surgery required. The approach is normally performed with a combination of a reciprocating saw and chisels to fracture off a sufficiently long section of the buccal cortex, revealing the underlying marrow. Care must be taken to avoid penetrating too deeply through the buccal plate with the reciprocating saw so as not to cause further iatrogenic nerve trauma. If necessary, the inferior border-reciprocating saw can be used to score the inferior border of the mandible to facilitate the splitting of the buccal plate. With careful manipulation of the marrow, the IAN can be identified and isolated and hopefully the site of injury identified. Efforts should be made to remove the buccal cortical plate in one piece, so that it is then stored moist in saline, and at the end of the surgery, it can be drilled out on the inner surface to avoid traumatizing or compressing the nerve and reattached with one screw for rigid stabilization. It is felt to be important that the IAN be covered on its buccal aspect by bone so that it is not in direct contact with the soft tissues of the cheek. One must be careful with the placement of the screw that it does not in itself iatrogenically damage the IAN (Fig. 14.2).


Fig. 14.2
(a) A buccal plate ostectomy outlined with a reciprocating saw. (b) Buccal plate removed to show the inferior alveolar nerve. (c) The buccal plate is stored in saline and hollowed out on its inner aspect to avoid compressing the IAN when the buccal plate is replaced. (d) The buccal plate replaced to protect the IAN and secured with one screw. (e) Radiographic appearance of the screw securing the buccal plate following IAN repair
2.
The IAN may be approached via a sagittal split osteotomy, and this can provide quite reasonable access to the nerve. The main complication of this technique is the possibility of a resulting malunion or malocclusion that would add to the patient’s concerns, in addition to the need to use bone screws or plates.
3.
A third approach is to drill directly through the buccal plate to the position of the IAN as identified from cone beam CT scanning (Fig. 14.3). Although the nerve can be approached in this way, it is located at the bottom of a trough, which does not lend itself to adequate exposure and visualization for nerve repair.
Fig. 14.3
The inferior alveolar nerve (arrow) approached directly through an isolated buccal plate decortication with a drill
4.
If the injury is in the region of the mental foramen, then the mental foramen must be identified and dissected out. This is normally done by means of the “donut” technique whereby the buccal cortex is perforated circumferentially about 3 mm from the mental foramen, and then, the perforations are joined together, and the resulting “donut” of bone is removed without injury to the nerve (Fig. 14.4). At this point, the IAN can be identified from the mental foramen and exposed appropriately. In many cases, when performing a mental nerve repair, the incisive branch of the IAN must be sacrificed.
Fig. 14.4
Diagram of the “donut hole” marked out around the mental foramen to gain access to the IAN
5.
It is sometimes recommended to perform a nerve repair through a tooth socket when the nerve has been injured or transected during removal of a tooth. In the author’s experience, this has been virtually impossible to achieve, and the best that can be carried out through a tooth socket is to reposition the two ends of the nerve as close as possible at the base of the socket and cover them with an inert barrier that can be resorbable or non-resorbable.
14.3 Surgical Procedures of the IAN
After having exposed, identified, and isolated the IAN via any of the above techniques, it must now be examined to determine the type of injury and the possibility of performing an adequate nerve repair. Conceptually, when visualized, the injury may be a crush-type injury or a partial transection or complete transection, which is usually relatively easy to identify. Stretch-type injuries and injuries from possible intraneural hematomas are more difficult to identify and tend to involve a greater length of the nerve. Iatrogenic injuries caused by a scalpel or other sharp instrument are often quite clean in nature, whereas those caused by a dental drill are often quite ragged [11]. Where the injury is more profound, and the time from injury to surgical intervention is increased, there is a higher possibility that neuroma formation has taken place. Depending upon the type of injury, this can be a lateral neuroma over a partial transection or a terminal neuroma over a complete transection [12]. Neuromas normally form on the proximal side of an injury, but smaller neuroma type lesions can also develop on the distal aspect of a nerve injury site. One of the advantages of operating early is that there is less possibility of neuroma formation, since it is generally felt that neuroma formation does not commence for 6–8 weeks after an injury and are not fully formed for several months. If there is a complete transection, or a neuroma has to be excised, it may be difficult to perform an end-to-end anastomosis since the IAN will only stretch a few millimeters, in contrast to the lingual nerve that can often be stretched 1–2 cm. Therefore, if a nerve gap of over 7 or 8 mm develops in the IAN, it probably cannot be reapproximated directly and will likely need an interpositional graft of some type.
In addition to the possibility of neuroma formation, another sequelae of delayed repair of a transection injury is that the nerve ends tend to retract away from the site of injury, and the gap may be filled with fibrous tissue, making surgical dissection difficult. There is also often some atrophy of the distal portion of the nerve, such that after several months, it may only be a fibrous strand of tissue (Fig. 14.5) and therefore very difficult to anastomose, with a predictably poor result. This may be due in part to the Wallerian degeneration that has occurred in the distal stump, and, in order for an effective repair to be performed, will require distal dissection to locate normal nerve fascicles for repair with an interpositional graft.
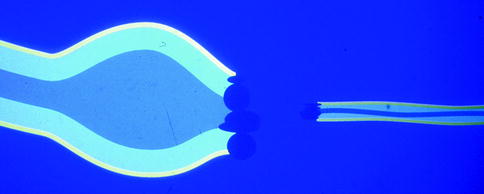
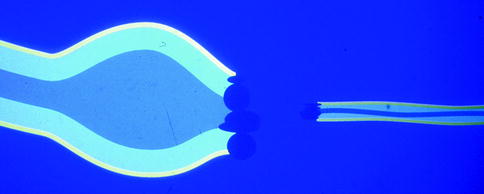
Fig. 14.5
Diagram of a transected IAN showing a neuroma at the proximal end (on left), and atrophy of the distal end (on right), making any nerve repair more difficult
In general, the sequencing of surgery is to first isolate the IAN, then examine it to determine the site and type of injury, and finally determine the type of repair that is necessary (direct vs. indirect (gap) repair).
Possible repair procedures include the following:
1.
If there is a clean transection with a sharp instrument, and the repair is carried out within 6–8 weeks, then a direct end-to-end anastomosis can often be carried out quite successfully, and, in fact, the fascicles can be lined up correctly (i.e., coaptation) on many occasions offering a better prognosis.
2.
If there is a partial transection, then it is sometimes possible to perform a direct repair on the partial transection by approximating the arms of the “V defect” together (Fig. 14.6).


Fig. 14.6
Nerve specimen showing a partial transection injury leaving a V-shaped defect, amenable to epineurial repair
3.
If there is a crush injury that can be clearly identified, or a neuroma that has to be excised, then the nerve should be mobilized as much as possible to perform a tension-free anastomosis following resection of the damaged segment, but, if this is not possible, an interpositional graft will be required, as will be described.
4.
Implant-related injuries of the IAN can be variable (Fig. 14.7). If the nerve injury is caused by the implant itself, it will usually take the form of a crush-type injury requiring removal of the implant from the area and possible excision of the crushed area of the nerve with a possible reanastomosis. In the author’s experience, if the patient has an implant-related IAN damage, immediate removal of the offending implant leads to neurosensory recovery in about 20 % of cases. However, most implant-related IAN injuries are likely caused by the initial drilling process involving the pilot twist drills. In this case, the injury to the nerve is often ragged and quite severe [11] and may be too extensive for a direct anastomosis and therefore may require an interpositional graft, with a subsequently lower success rate.
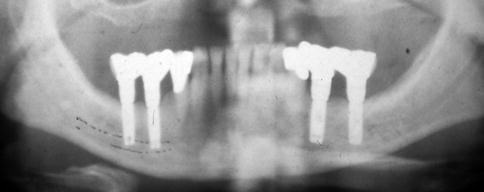
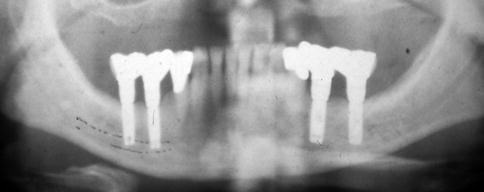
Fig. 14.7
Panorex showing implants encroaching on the inferior alveolar canal and IAN
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


