Armamentarium
|
History of the Procedure
Surgeons often must treat head and neck defects caused by ablative surgery or injury. Reconstruction of complex head and neck defects with functional and morphologic restoration has long been a highly challenging and complex surgical undertaking. Many techniques have been developed to treat these defects, including skin grafts, local or regional flaps, free vascularized tissue transfer, and tissue expansion for reconstruction. Although skin grafting is technically simple and can provide good esthetic results with low morbidity, it cannot be used for complex defects. Tissue expansion is another option for cutaneous coverage, but this technique requires multiple operative procedures and a significant commitment by the patient. Random pattern flaps (advancement flap, rotation flap) and platysma myocutaneous flaps can provide a good color match for the face; however, they are often unreliable, and mobility and the amount of tissue that can be used are limited. Also, in many cases the scars at the donor site are unacceptable. A pedicled flap, such as a trapezius or pectoralis myocutaneous flap, can provide sufficient transplant tissue and is suitable for reconstructing large head and neck defects. However, this flap is too bulky to be suitable for reconstructing small or medium-sized defects in the head and neck region.
Advances in microsurgery have allowed many complex facial defects to be reconstructed with free flaps, such as radial forearm or other free fasciocutaneous flaps; however, the color and texture of these flaps show a definite demarcation with the neighboring facial skin. In addition, these flaps are more surgically complex and have the potential for flap failure associated with microsurgical techniques. For reconstruction of head and neck defects, the flap should be reliable, pliable, and functionally and cosmetically acceptable; it also should have minimum donor site morbidity and should match the recipient site in color, texture, and thickness.
In 1993, Martin et al. first described a new axial-patterned island flap based on the submental artery. This new flap, the submental island flap, enhanced the reliability and mobility of the random cervical platysma myocutaneous flap and also was free of the limitations of the latter, described previously. The submental island flap consists of thin, pliable tissues with a perfect color match and is similar to facial skin. It also has a robust blood supply and a good arc of rotation. When applied in older patients, this procedure can also reduce the submental fullness and have positive esthetic results. Significant research on its anatomy and applications has shown that the submental island flap is ideal for head and neck reconstruction. This flap also has been described as a free flap. All these advantages make the submental island flap easy to work with, and it is widely used by numerous other authors.
Anatomy
The basis for the submental island flap is the submental artery, which is reported to be a well-defined, consistent branch of the facial artery with a diameter of 1 to 2 mm. It arises from the facial artery, deep or superficial to the submandibular gland, approximately 1.5 to 2 cm below the inferior border of the mandible, and passes forward and medially on the mylohyoid muscle below the mandibular border, ending behind the mandibular symphysis just lateral to the midline. Most commonly, it runs deep to the anterior belly of the digastric muscle and sends off some branches to the submental skin, lower lip, and sublingual gland ( Figure 112-1 ).
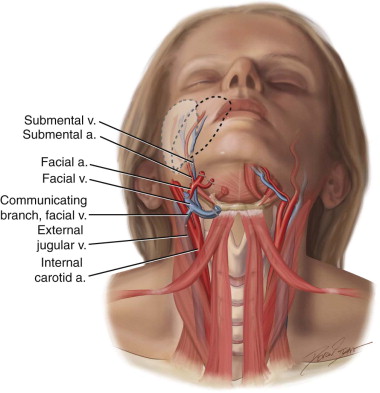
Along its course, one to four cutaneous perforators are found piercing the overlying platysma, forming a subdermal plexus that anastomoses extensively with the contralateral branches, providing a possible large random extension on the other side. Venous drainage of this flap is through the submental vein into the facial vein. There are one to three anastomoses between these vessels and the external jugular vein, which plays a major role in the surgical procedure and in some cases may be used for the venous drainage of the flap. Because of its reliable blood supply, this flap can be harvested from mandibular angle to mandibular angle, with the width determined by the flaccidity of the neck skin; this allows direct closure with a well-hidden donor scar of up to 18 × 7 cm in size. The pedicle may be up to 8 cm long, and the arc of the pedicle is such that the flap easily reaches defects of the face.
History of the Procedure
Surgeons often must treat head and neck defects caused by ablative surgery or injury. Reconstruction of complex head and neck defects with functional and morphologic restoration has long been a highly challenging and complex surgical undertaking. Many techniques have been developed to treat these defects, including skin grafts, local or regional flaps, free vascularized tissue transfer, and tissue expansion for reconstruction. Although skin grafting is technically simple and can provide good esthetic results with low morbidity, it cannot be used for complex defects. Tissue expansion is another option for cutaneous coverage, but this technique requires multiple operative procedures and a significant commitment by the patient. Random pattern flaps (advancement flap, rotation flap) and platysma myocutaneous flaps can provide a good color match for the face; however, they are often unreliable, and mobility and the amount of tissue that can be used are limited. Also, in many cases the scars at the donor site are unacceptable. A pedicled flap, such as a trapezius or pectoralis myocutaneous flap, can provide sufficient transplant tissue and is suitable for reconstructing large head and neck defects. However, this flap is too bulky to be suitable for reconstructing small or medium-sized defects in the head and neck region.
Advances in microsurgery have allowed many complex facial defects to be reconstructed with free flaps, such as radial forearm or other free fasciocutaneous flaps; however, the color and texture of these flaps show a definite demarcation with the neighboring facial skin. In addition, these flaps are more surgically complex and have the potential for flap failure associated with microsurgical techniques. For reconstruction of head and neck defects, the flap should be reliable, pliable, and functionally and cosmetically acceptable; it also should have minimum donor site morbidity and should match the recipient site in color, texture, and thickness.
In 1993, Martin et al. first described a new axial-patterned island flap based on the submental artery. This new flap, the submental island flap, enhanced the reliability and mobility of the random cervical platysma myocutaneous flap and also was free of the limitations of the latter, described previously. The submental island flap consists of thin, pliable tissues with a perfect color match and is similar to facial skin. It also has a robust blood supply and a good arc of rotation. When applied in older patients, this procedure can also reduce the submental fullness and have positive esthetic results. Significant research on its anatomy and applications has shown that the submental island flap is ideal for head and neck reconstruction. This flap also has been described as a free flap. All these advantages make the submental island flap easy to work with, and it is widely used by numerous other authors.
Anatomy
The basis for the submental island flap is the submental artery, which is reported to be a well-defined, consistent branch of the facial artery with a diameter of 1 to 2 mm. It arises from the facial artery, deep or superficial to the submandibular gland, approximately 1.5 to 2 cm below the inferior border of the mandible, and passes forward and medially on the mylohyoid muscle below the mandibular border, ending behind the mandibular symphysis just lateral to the midline. Most commonly, it runs deep to the anterior belly of the digastric muscle and sends off some branches to the submental skin, lower lip, and sublingual gland ( Figure 112-1 ).
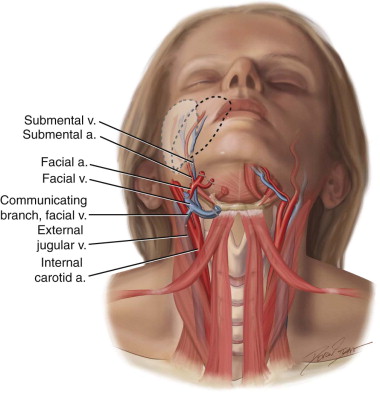
Along its course, one to four cutaneous perforators are found piercing the overlying platysma, forming a subdermal plexus that anastomoses extensively with the contralateral branches, providing a possible large random extension on the other side. Venous drainage of this flap is through the submental vein into the facial vein. There are one to three anastomoses between these vessels and the external jugular vein, which plays a major role in the surgical procedure and in some cases may be used for the venous drainage of the flap. Because of its reliable blood supply, this flap can be harvested from mandibular angle to mandibular angle, with the width determined by the flaccidity of the neck skin; this allows direct closure with a well-hidden donor scar of up to 18 × 7 cm in size. The pedicle may be up to 8 cm long, and the arc of the pedicle is such that the flap easily reaches defects of the face.
Indications for the Use of the Procedure
For reconstruction of head and neck defects, the ideal is to achieve both functional and esthetic outcomes. Additional donor site morbidity should be avoided, especially with benign diseases. The proximity of the donor site and its characteristics of reliability, excellent skin match, minimal donor site morbidity, and a long pedicle make the submental island flap an ideal method for reconstruction of head and neck defects caused by trauma, burns, or surgical defects. Furthermore, the relative simplicity of raising this flap gives the additional benefit of a shorter operative time, especially in older patients and those with significant comorbidities.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


