Submandibular Approach
The mandible can be exposed by surgical approaches using incisions placed on the skin of the face. The position of the incisions and anatomy vary depending on the region of the mandible that is approached. Because there are almost no anatomic hazards in the transfacial exposure of the mandibular symphysis, this approach is not presented. The focus of this section is on the submandibular, retromandibular, and rhytidectomy approaches. All these are used to expose the posterior regions of the mandible and all must negotiate important anatomic structures. Approaches to the temporomandibular joint are presented in Section 6.
|
The submandibular approach is one of the most useful approaches to the mandibular ramus and posterior body region, and is occasionally referred to as the Risdon approach. This approach may be used for obtaining access to a myriad of mandibular osteotomies, angle/body fractures, and even condylar fractures and temporomandibular joint (TMJ) ankylosis. Descriptions of the approach differ on some points, but in all the incision is made below the inferior border of the mandible.
SURGICAL ANATOMY
Marginal Mandibular Branch of the Facial Nerve
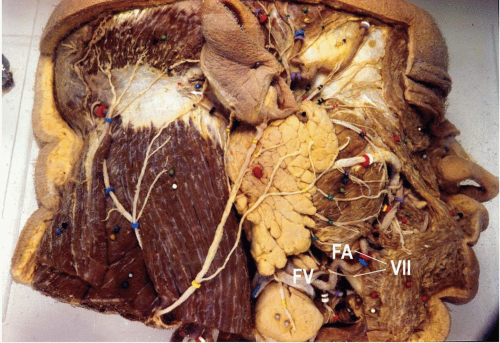
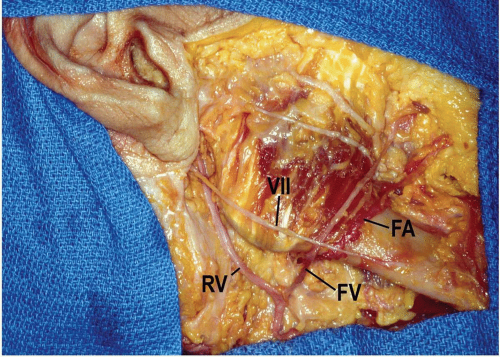
After the facial nerve divides into temporofacial and cervicofacial branches, the marginal mandibular branch originates and extends anteriorly and inferiorly within the substance of the parotid gland. The marginal mandibular branch or branches, which supply motor fibers to the facial muscles in the lower lip and chin, represent the most important anatomic hazard while performing the submandibular approach to the mandible. Studies have shown that the nerve passes below the inferior border of the mandible only in very few individuals (see Fig. 9.1). In the Dingman and Grabb classic dissection of 100 facial halves, the marginal mandibular branch was almost 1 cm below the inferior border in 19% of the specimens (1). Anterior to the point where the nerve crossed the facial artery, all dissections in the above study displayed the nerve above the inferior border of the mandible.
Ziarah and Atkinson (2) found more individuals in whom the marginal mandibular branch passed below the inferior border. In 53% of 76 facial halves, they found the marginal mandibular branch passing below the inferior border before reaching the facial vessels, and in 6%, the nerve continued for a further distance of almost 1.5 cm before turning upward and crossing the mandible. The farthest distance between a marginal mandibular branch and the inferior border of the mandible was 1.2 cm. In view of these findings, most surgeons recommend that the incision and deeper dissection be at least 1.5 cm below the inferior border of the mandible.
Another important finding of the study by Dingman and Grabb (1) was that only 21% of the individuals had a single marginal mandibular branch between the angle of the mandible and the facial vessels (see Fig. 9.2); 67% had two branches (Fig. 9.1), 9% had three branches, and 3% had four.
Facial Artery
After it originates from the external carotid artery, the facial artery follows a cervical course during which it is carried upward medial to the mandible and in fairly close contact with the pharynx. It runs superiorly, deep to the posterior belly of the digastric and stylohyoid muscles, and then crosses above them to descend on the medial surface of the mandible, grooving or passing through the submandibular salivary gland as it rounds the lower border of the mandible. It is visible on the external surface of the mandible around the anterior border of the masseter muscle (Figs. 9.1 and 9.2). Above the inferior border of the mandible, it lies anterior to the facial vein and is tortuous.
Facial Vein
The facial (anterior facial) vein is the primary venous outlet of the face. It begins as the angular vein, in the angle between the nose and eye. It generally courses along with the facial artery above the level of the inferior mandibular border, but it is posterior to the artery (Figs. 9.1 and 9.2). Unlike the facial artery, the facial vein runs across the surface of the submandibular gland to end in the internal jugular vein.
TECHNIQUE
▶ Step 1. Preparation and Draping
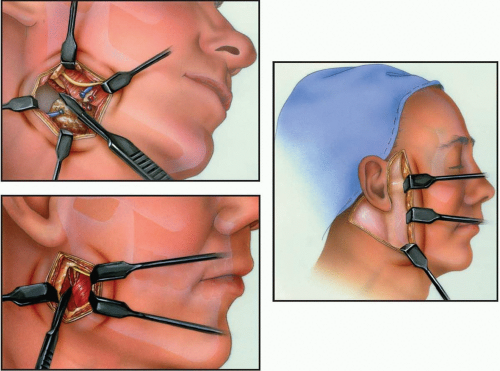
Pertinent landmarks on the face, useful during dissection, should be left exposed throughout the procedure. For surgeries involving the mandibular ramus/angle, the corner of the mouth and lower lip should be exposed within the surgical field anteriorly and the ear, or at least the ear lobe, posteriorly. These landmarks help the surgeon to mentally visualize the course of the facial nerve and to see whether the lip moves if stimulated.
▶ Step 2. Marking the Incision and Vasoconstriction
The skin is marked prior to the injection of a vasoconstrictor. The incision is placed 1.5 to 2 cm inferior to the mandible. Some surgeons place the incision parallel to the inferior border of the mandible; others place the incision in or parallel to a neck crease (see Fig. 9.3). Incisions made parallel to the inferior border of the mandible may be unobtrusive in some patients; however, extensions of this incision anteriorly may be noticeable unless hidden in the submandibular shadow. A less conspicuous scar results when the incision is made in or parallel to a skin crease. It should be noted that skin creases below the mandible do not parallel the inferior border of the mandible but run obliquely, posterosuperiorly to anteroinferiorly. Therefore, the further anterior the incision in or parallel to a skin crease, the more the distance to dissect to reach the inferior border of the mandible. Both incisions can be extended posteriorly to the mastoid region if necessary.
Mandibular fractures that shorten the vertical height of the ramus by their displacement (e.g., condylar fractures in patients without posterior teeth or those not placed into MMF) will cause the angle of the mandible to be more superior than it would be following reduction and fixation. Therefore, the incision should be placed 1.5 to 2 cm inferior to the anticipated location of the inferior border.
The incision is located along a suitable skin crease in the anteroposterior position that is needed for mandibular exposure. For a fracture that extends toward the gonial angle, the incision should begin behind and above the gonial angle, and extend downward and forward until it is in front of the gonial angle. For fractures located more anterior than the gonial angle, the incision does not have to extend behind and/or above the gonial angle, but may have to extend further anteriorly.
Vasoconstrictors with local anesthesia injected subcutaneously to aid hemostasis should not be placed deep to the platysma muscle because the marginal mandibular branch of the facial nerve may be rendered nonconductive, making electrical testing impossible. Alternatively, a vasoconstrictor without local anesthesia can be used both superficially and deep to the platysma muscle to promote hemostasis.
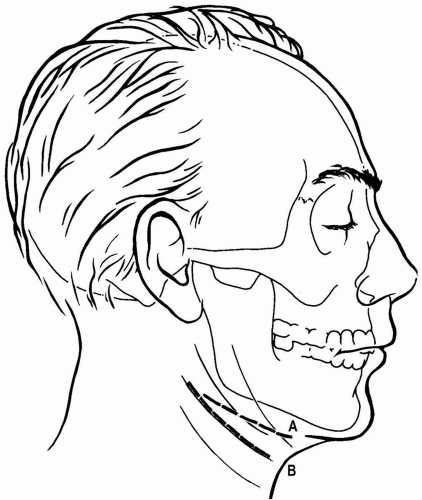
Figure 9.3 Two locations of submandibular incisions. Incision A parallels the inferior border of the mandible. Incision B parallels or is within the resting skin tension lines. Incision B leaves a less conspicuous scar in most patients.
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

|