Introduction
Surgically assisted rapid palatal expansion (SARPE) is the procedure of choice for treatment of adults with transverse maxillary deficiency greater than 7 mm. There is no consensus about the dentoskeletal effect of an orthodontic retainer on the outcome of SARPE. Our objective was to assess the effectiveness of an orthodontic retainer on dentoskeletal stability.
Methods
Ninety digitized dental casts of 30 adults undergoing SARPE were divided into 2 groups—no retention (n = 15) and retention (n = 15)—and assessed. The dental casts were obtained at 3 checkpoints: (1) 7 days on average before SARPE (preoperatively), (2) 4 months after expansion, and (3) 10 months after expansion was completed. The retention patients received a transpalatal arch just after expander removal, at checkpoint 2. The transpalatal arch was kept for 10 months after completion of the expansion (checkpoint 3 and end of the study). The dental casts were scanned with a Vivid 9i 3D laser scanner (Konica Minolta, Wayne, NJ). The distances measured were premolar and molar intercusp distances, premolar and molar intercervical distances, premolar and molar inter-WALA (Will Andrews and Lawrence Andrews) ridge distances, and palate height at the maxillary first molar.
Results
The planned maxillary expansion was within the expected amount ( P <0.05). Palatal height at the 4-month checkpoint decreased by 0.79 mm (4.38%) ( P <0.001) and again at the 10-month checkpoint by 0.38 mm (0.98%) ( P >0.05) but not significantly in both groups. The premolar intercusp distance had a relapse at checkpoint 3 of 1.84 mm (7.18%) ( P <0.001) in the no-retention group. Both groups had average relapses of 0.95 mm in the premolar intercervical distances, of 0.88 mm in the premolar inter-WALA ridge distances, of 1.04 mm in the molar intercusp distances, of 0.74 mm in the molar intercervical distances, and of 0.84 mm in the molar inter-WALA ridge distances ( P <0.05) at checkpoint 3.
Conclusions
The analysis of relapse in both groups suggests that the use of a transpalatal arch as a retaining device does not improve dento-osseous stability.
Surgically assisted rapid palatal expansion (SARPE) is the treatment of choice to correct transverse maxillary deficiencies greater than 7 mm in skeletally mature patients. SARPE is an orthopedic procedure in which areas resisting expansion are surgically released by osteotomy, and an expander is activated after surgery until the desired amount of expansion is achieved.
The surgical results are thought to be maintained using fixed or removable retainers, which would ensure the dimensional stability of SARPE. To date, there is no consensus regarding the time allowed for effective bone healing before removing the expansion device, the time to begin orthodontic treatment, and the effectiveness of a transpalatal arch (orthodontic retainer) to guarantee the skeletal expansion with SARPE.
The outcome of SARPE can be assessed indirectly by studying radiographs or tomographs, or directly by analyzing dental casts. Radiographs are not expensive, but superimpositions of cranial bone structures and dental units compromise precise measurements. Tomographic imaging provides a much better visualization but involves high costs and might not be readily available in some countries. Using plaster models to assess the outcome of maxillary dental arch expansion combines low cost, simplicity, and accuracy. Recent advances in technology and computer science have made the accurate digitization of objects available. This enhances the dimensional assessment of dental casts and, most importantly, saves the space formerly used to store models.
Object digitization by laser scanning is simple and fast. Studies have shown that this technology produces measurements that are as reliable as those taken directly on the dental models. Therefore, in this study, we aimed to assess the effectiveness of an orthodontic retainer as a means of guaranteeing dentoskeletal stability after SARPE.
Material and methods
This research was approved by the research ethics committee of the Federal University of São Paulo in Brazil (clinical trials number, NCT01770782; #0949/09). All participants signed an informed consent form.
After sample size calculation, the images of 90 digitized plaster casts from 30 patients who had SARPE at the Cranio-maxillofacial Surgery Outpatient Clinic of the Division of Plastic Surgery were assessed.
Based on a 5-participant sample from the 2 treatment groups and the 2 main measurements of interest—the molar and premolar WALA (Will Andrews and Lawrence Andrews) ridge distance—the relapse variation was less than 0.5 mm in both groups (SD, <0.5 mm). Assuming that the nondifference in relapse between the participants who used or did not use retainers was not greater than 1 mm, with 80% power and a 95% confidence interval, we calculated the number of participants at 4 per group. Nevertheless, to detect even smaller differences in relapse between the 2 groups, 15 participants were included in each group.
Adults with a bilateral crossbite and a transverse maxillary deficiency greater than 5 mm were included in the study. Patients with previous maxillary surgery, congenital craniofacial deformities, or a unilateral transverse maxillary deficiency were excluded.
The sample was randomized with 10-patient blocks in 2 groups. The group without retention comprised 15 patients—8 men (53.3%), 7 women (46.7%); average age, 26.3 years (SD, 5.3 years)—and none was prescribed any type of retention after removal of the expander. The group with retention also comprised 15 patients—10 men (66.7%), 5 women (33.3%); average age, 25.3 years (SD, 6.0 years)—and they received transpalatal arch fixed retainers.
On average, approximately 1 week before surgery, the same orthodontist (G.P.R.P.) placed modified hyrax-like devices (A2620-12; Leone, Florence, Italy) in all participants. The devices were made by the same laboratory technician. Initial plaster casting was performed before expander cementation (preoperatively) using type IV plaster.
Surgery was performed in all 30 participants by the same surgeon (M.D.P.), who used the subtotal LeFort I technique, with separation of the pterygomaxillary fissure. The operation was performed under general anesthesia with orotracheal intubation. After the osteotomies, the expander screw was activated to 1.6 mm intraoperatively until a small diastema was observed between the maxillary central incisors. The incision was sutured in 2 layers.
On postoperative day 4, the expander screw activation protocol was initiated, rotating a quarter turn (0.2 mm) twice per day. After achieving the intended expansion of the maxilla width, the expansion screw was blocked, and the hyrax appliance was left in place for 4 months.
After this 4-month period, the hyrax appliance was removed, and a second plaster casting was performed for all patients. Whereas the patients in the retention group received a transpalatal arch ( Fig 1 ) for orthodontic retention, those in the no-retention group received no orthodontic device.
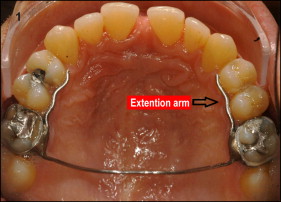
The transpalatal arches in the retention patients were made with a 1.2-mm-diameter stainless steel wire and had welded bands for fixation onto the maxillary first molars. The transpalatal arch’s extension arms reached the first premolars. Both groups resumed their routine activities for 6 months. Then they were contacted to have the transpalatal arches removed (retention patients) and to have a third plaster model cast (all patients).
The digitized plaster casts captured by a surface laser scanner (Vivid 9i; Minolta, Wayne, NJ) connected to a computer (Vaio model PCG-81311X; Sony, Tokyo, Japan) were stored for reading and elaboration of a polygon representing a virtual copy of the original plaster cast; this procedure was performed using software specific for 3-dimensional (3D) data (Qualify, version 12.0; Geomagic, Rock Hill, SC).
Measurements were made on the digitized images of each plaster cast. The dentoskeletal transverse measurements were the following.
- 1.
Premolar and molar intercusp distances: the distances between the palatal cusp tips of the maxillary first premolars and between the mesiolingual cusp tips of the maxillary first molars ( Fig 2 , A ).
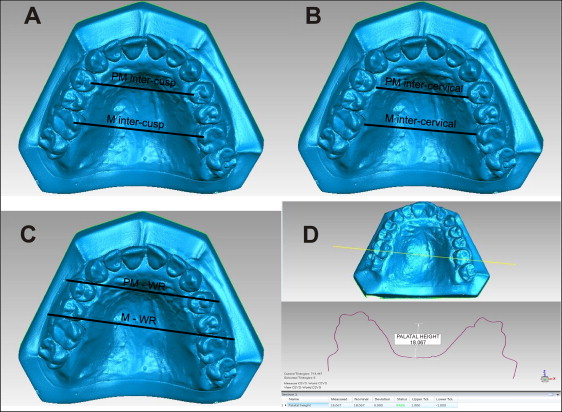
Fig 2 Transverse measurements: A, occlusal view of the premolar and molar intercusp distances; B, occlusal view of the premolar and molar intercervical distances; C, occlusal view of the premolar (P-WR) and molar (M-WR) inter-WALA ridge distances; D, upper , cross section of a 3D model at the main sulcus area of the palatal side (maxillary first molars), and lower , cross-sectional measurement of palatal height. - 2.
Premolar and molar intercervical distances: the distance between the most palatal points of the gingival margin of the maxillary first premolars or molars ( Fig 2 , A ).
- 3.
Premolar and molar inter-WALA ridge distances: the distances between the most prominent points on the alveolar process of the maxillary first premolars and molars ( Fig 2 , B )
- 4.
Palate height at the maxillary first molar: measured at the cross-section on the 3D model at the main sulcus area of the palatal side of the maxillary first molars to the deepest palatal area ( Fig 2 , C and D ).
The measurements were made by 2 investigators (G.P.R.P., J.P.R.B.). One investigator made 2 assessments with a 15-day interval between them, and the other investigator made 1 assessment.
Statistical analysis
The Kolmogorov-Smirnov test was used to investigate the normality of the sample distribution.
The participants’ ages and the expansion amounts were described per group and compared using the Student t test. The associations between the groups and the patients’ sex were analyzed using the chi-square test.
To assess the intraexaminer and interexaminer agreements relative to the 3D scanner method, the intraclass correlation coefficient was calculated with the corresponding 95% confidence interval.
All investigated measurements were described by group (with and without retention) and assessment time (preoperative, 4 months, and 10 months) using summary measures and 2-way repeated-measures analysis of variance (ANOVA) relative to the factor of time point. A first-order autoregressive matrix of correlation among the assessment times was assumed. The Tukey multiple comparison test was performed on the measurements with statistical significance to determine the relevant groups or time points.
The level of null hypothesis rejection was <5%.
Results
The no-retention and retention patients had average expansions of 8.40 mm (SD, 1.46) and 8.95 mm (SD, 1.22), respectively. The groups did not differ regarding age ( P = 0.609), sex ( P = 0.456), or expansion after SAPRE ( P = 0.272).
The intraexaminer agreement was high relative to both measurements, with an intraclass correlation coefficient exceeding 0.90.
Only the premolar intercusp measurement showed an interaction effect between the groups and over the time points ( P = 0.04). The premolar intercervical, premolar WALA ridge, molar intercusp, molar intercervical, molar WALA ridge, and molar palatal height measurements had no interaction effects between the groups and the time points ( P >0.05) and were statistically similar in both groups over time. All means exhibited significant differences over time ( P <0.01). There were no significant differences between groups related to relapse except for the premolar intercusp measurement in the no-retention group ( Table I ).
| Period | Group | ANOVA ∗ | ||||
|---|---|---|---|---|---|---|
| NRG (n = 15), Mean (SD) | RG (n = 15), Mean (SD) | Interaction | Time | Group | ||
| PM intercusp (mm) | Preop | 25.68 (3.58) | 27.12 (3.15) | |||
| 4 mo | 34.10 (3.55) | 35.65 (2.97) | 0.004 ∗ | <0.001 ∗ | 0.061 | |
| 10 mo | 32.26 (3.05) | 35.68 (3.20) | ||||
| M intercusp (mm) | Preop | 34.88 (4.47) | 36.03 (3.82) | |||
| 4 mo | 43.22 (4.72) | 44.91 (3.94) | 0.164 | <0.001 ∗ | 0.199 | |
| 10 mo | 41.73 (4.32) | 44.34 (3.44) | ||||
| PM intercervical (mm) | Preop | 22.78 (3.16) | 24.18 (2.58) | |||
| 4 mo | 30.89 (2.96) | 32.88 (2.57) | 0.079 | <0.001 ∗ | 0.035 ∗ | |
| 10 mo | 29.48 (2.58) | 32.38 (2.96) | ||||
| M intercervical (mm) | Preop | 29.34 (3.93) | 30.97 (3.23) | |||
| 4 mo | 37.58 (4.16) | 39.82 (3.06) | 0.095 | <0.001 ∗ | 0.064 | |
| 10 mo | 36.45 (3.98) | 39.48 (2.71) | ||||
| PM-WR (mm) | Preop | 42.46 (2.57) | 43.62 (2.49) | |||
| 4 mo | 49.58 (2.74) | 51.35 (2.65) | 0.276 | <0.001 ∗ | 0.070 | |
| 10 mo | 48.57 (2.34) | 50.59 (2.94) | ||||
| M-WR (mm) | Preop | 54.46 (4.08) | 54.84 (2.70) | |||
| 4 mo | 62.11 (3.98) | 63.14 (2.89) | 0.300 | <0.001 ∗ | 0.454 | |
| 10 mo | 61.13 (3.99) | 62.45 (2.97) | ||||
| Palatal height (mm) | Preop | 18.22 (2.37) | 17.89 (1.62) | |||
| 4 mo | 17.22 (2.21) | 17.30 (1.94) | 0.340 | <0.001 ∗ | 0.987 | |
| 10 mo | 16.94 (2.24) | 17.23 (1.84) | ||||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


