Armamentarium
| Flap Harvest |
|
| Microvascular Instruments |
|
| Donor Site Closure |
|
| Flap Insetting |
|
History of the Procedure
First described by dos Santos in 1980, the scapular flap, along with the subscapular artery system upon which it is based, is recognized as the most dynamic donor region available for free tissue transfer to the head and neck. The subscapular artery system gives rise to a variety of flaps: fasciocutaneous (scapular/parascapular/thoracodorsal artery perforator), osteofasciocutaneous (scapular/parascapular with lateral scapular border or tip), musculocutaneous (latissimus dorsi/serratus anterior), and musculo-osteocutaneous (latissimus dorsi/serratus anterior + rib). Vascularized bone, muscle, fat, skin, and fascia may be transferred as discrete components or combined as a chimeric flap on a single pedicle for composite reconstruction involving disparate axes.
The first clinical application of the scapular free flap was reported by Gilbert and Teot in four cases of lower extremity reconstruction. This was followed by a number of successful cases of fasciocutaneous transfer, citing a substantial improvement in postoperative morbidity compared to the latissimus dorsi myocutaneous flap. These studies were possible following earlier dye injection cadaver studies by Saijo, which elucidated the angiosomes of the circumflex scapular, thoracodorsal, and posterior intercostal arteries. He predicted that a fasciocutaneous flap based on the circumflex scapular artery could supply up to 15 × 20 cm of thin, pliable skin supplied by a consistent pedicle of sufficient caliber for microvascular anastomosis. Teot and coworkers first identified the potential for vascularized bone transfer in their report describing the pedicled lateral scapular border as part of an osteocutaneous flap. Further anatomic studies outlined the neurovascular and musculoskeletal anatomy of the subscapular system, providing microsurgeons with parameters to optimize flap perfusion and bone volume. Novel modifications soon followed. Nassif described the vertically oriented parascapular flap as a fasciocutaneous flap based on a vertical branch of the circumflex scapular artery, with the potential to include a portion of latissimus dorsi muscle inferiorly. Batchelor and Bardsley introduced a biscapular fasciocutaneous flap, anastomosing bilateral circumflex scapular arteries in the upper and lower leg for a 40-cm soft tissue defect. Suitability of the superficial temporal artery for anastomosis to the circumflex scapular artery was initially reported in 1984 in several cases of scalp reconstruction.
Mandibular and maxillary reconstruction using scapular bone has been cited extensively with laudable results. Swartz and colleagues first employed lateral borders and lateral border/scapular tip bones for reconstruction in 26 cases of maxillectomy and composite mandibular defects. The course of the angular artery and its periosteal perforators supplying the scapular tip was later described by Deraemaecker and colleagues, leading to its popularization as a source of bone stock. Coleman and Sultan initially described scapular tip for mandibular and midface reconstruction as a bipedicled osteocutaneous flap, with a separate skin paddle based on the circumflex scapular artery. The medial border may be harvested for improved pedicle length, but this bone is of poorer stock than the lateral border and must remain attached to the overlying skin. Baker and Sullivan noted the advantage of separate pedicles for soft tissue and bone segments in their report on one-stage mandibular reconstruction. Large cutaneous or mucosal defects up to 12 × 10 cm with corresponding segmental bone gaps of up to 14.5 cm were restored simultaneously. Suitability for dental implants was reported by Moscoso and colleagues in their study of 28 cadavers. Serial cross sections of the lateral border of the scapula showed greater implantability distal from the glenohumeral joint, where bone stock is thickest. Overall, 78% of harvested scapular bone segments were deemed fit for implant placement, defined as those with a neomandibular height of 10 mm and a width of 5 mm or more. This was significantly more consistent than the fibula free flap. Numerous studies have upheld the importance of dental rehabilitation and mastication in functional outcomes, along with labial competence, deglutition, facial cosmesis, and speech. Since its introduction, the scapular free flap has maintained its role as a readily harvested flap with negligible donor site morbidity and wide reconstructive applications.
History of the Procedure
First described by dos Santos in 1980, the scapular flap, along with the subscapular artery system upon which it is based, is recognized as the most dynamic donor region available for free tissue transfer to the head and neck. The subscapular artery system gives rise to a variety of flaps: fasciocutaneous (scapular/parascapular/thoracodorsal artery perforator), osteofasciocutaneous (scapular/parascapular with lateral scapular border or tip), musculocutaneous (latissimus dorsi/serratus anterior), and musculo-osteocutaneous (latissimus dorsi/serratus anterior + rib). Vascularized bone, muscle, fat, skin, and fascia may be transferred as discrete components or combined as a chimeric flap on a single pedicle for composite reconstruction involving disparate axes.
The first clinical application of the scapular free flap was reported by Gilbert and Teot in four cases of lower extremity reconstruction. This was followed by a number of successful cases of fasciocutaneous transfer, citing a substantial improvement in postoperative morbidity compared to the latissimus dorsi myocutaneous flap. These studies were possible following earlier dye injection cadaver studies by Saijo, which elucidated the angiosomes of the circumflex scapular, thoracodorsal, and posterior intercostal arteries. He predicted that a fasciocutaneous flap based on the circumflex scapular artery could supply up to 15 × 20 cm of thin, pliable skin supplied by a consistent pedicle of sufficient caliber for microvascular anastomosis. Teot and coworkers first identified the potential for vascularized bone transfer in their report describing the pedicled lateral scapular border as part of an osteocutaneous flap. Further anatomic studies outlined the neurovascular and musculoskeletal anatomy of the subscapular system, providing microsurgeons with parameters to optimize flap perfusion and bone volume. Novel modifications soon followed. Nassif described the vertically oriented parascapular flap as a fasciocutaneous flap based on a vertical branch of the circumflex scapular artery, with the potential to include a portion of latissimus dorsi muscle inferiorly. Batchelor and Bardsley introduced a biscapular fasciocutaneous flap, anastomosing bilateral circumflex scapular arteries in the upper and lower leg for a 40-cm soft tissue defect. Suitability of the superficial temporal artery for anastomosis to the circumflex scapular artery was initially reported in 1984 in several cases of scalp reconstruction.
Mandibular and maxillary reconstruction using scapular bone has been cited extensively with laudable results. Swartz and colleagues first employed lateral borders and lateral border/scapular tip bones for reconstruction in 26 cases of maxillectomy and composite mandibular defects. The course of the angular artery and its periosteal perforators supplying the scapular tip was later described by Deraemaecker and colleagues, leading to its popularization as a source of bone stock. Coleman and Sultan initially described scapular tip for mandibular and midface reconstruction as a bipedicled osteocutaneous flap, with a separate skin paddle based on the circumflex scapular artery. The medial border may be harvested for improved pedicle length, but this bone is of poorer stock than the lateral border and must remain attached to the overlying skin. Baker and Sullivan noted the advantage of separate pedicles for soft tissue and bone segments in their report on one-stage mandibular reconstruction. Large cutaneous or mucosal defects up to 12 × 10 cm with corresponding segmental bone gaps of up to 14.5 cm were restored simultaneously. Suitability for dental implants was reported by Moscoso and colleagues in their study of 28 cadavers. Serial cross sections of the lateral border of the scapula showed greater implantability distal from the glenohumeral joint, where bone stock is thickest. Overall, 78% of harvested scapular bone segments were deemed fit for implant placement, defined as those with a neomandibular height of 10 mm and a width of 5 mm or more. This was significantly more consistent than the fibula free flap. Numerous studies have upheld the importance of dental rehabilitation and mastication in functional outcomes, along with labial competence, deglutition, facial cosmesis, and speech. Since its introduction, the scapular free flap has maintained its role as a readily harvested flap with negligible donor site morbidity and wide reconstructive applications.
Indications for the Use of the Procedure
Scapular and parascapular osteocutaneous flaps are associated with acceptable donor site features, including the potential for primary closure without a skin graft, a well-hidden scar, and limited functional impairment. The circumflex scapular artery provides up to 4 cm of length, with a caliber of 2.5 to 4 mm before dividing into transverse and ascending scapular branches, which supply the scapular and parascapular skin paddles, respectively. In patients with peripheral vascular disease affecting the lower extremities and precluding use of the fibular or deep circumflex iliac artery osteocutaneous flaps, the scapular system provides reliable vessels and good bone stock for reconstruction and is rarely affected by atherosclerosis.
Head and Neck Reconstruction
Total Hard Palate Reconstruction
The scapular tip conforms well to defects resulting from subtotal or total maxillectomy without orbital exenteration. Although not always amenable to dental implant rehabilitation, the scapular tip adapts well to hard palate defects, effectively separating the oral and nasal cavities. In their series of 46 patients, Brown and associates cited successful use of the scapular flap in head and neck reconstruction, including midfacial reconstruction with the latissimus dorsi + scapular tip.
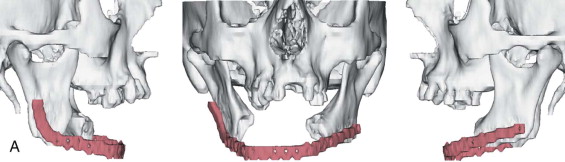
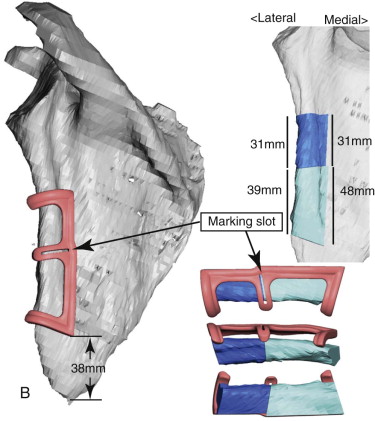
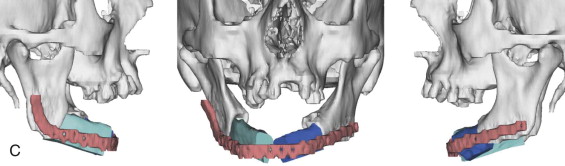
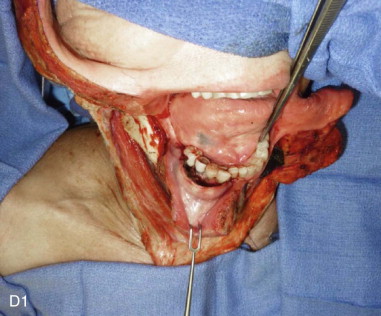
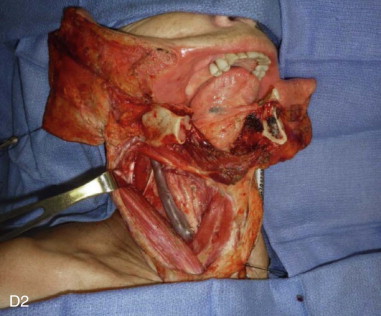
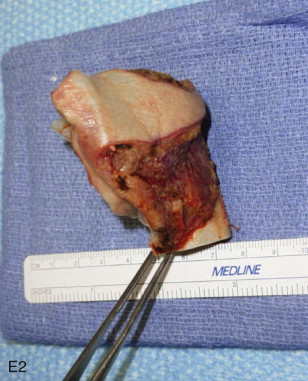
Mandible
Mandibular continuity defects may be reconstructed using a scapular tip for anterior defects or a lateral or medial border for posterior defects. Boahene has successfully applied the scapular tip to temporomandibular reconstruction as a novel condylar head replacement ( Figure 116-1, A-G ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses