The palate has been reported to be a suitable skeletal anchorage site in adolescents and adults. This article introduces new treatment modalities for correction of sagittal discrepancies by molar protraction and distalization with a modified palatal anchorage plate appliance. The effectiveness and versatility of this method are demonstrated in 2 adolescent patients.
Highlights
- •
Modified palatal anchorage plate appliance (MPAP) was used for correction of sagittal discrepancies in noncompliant patients.
- •
MPAP produced dental and skeletal changes in the maxilla.
- •
Both distalization and protraction of the total dental arch were achieved.
- •
The treatment was achieved through bodily movement of the maxillary molars.
For decades, the palate has been used as a foundation for skeletal anchorage because of its strong bony structure and low risk of contacting roots or vital structures. Although palatal bone thickness and density might be adequate for adults, there could be some doubt about applying temporary skeletal anchorage devices (TSADs) on the palate of young patients. Therefore, several studies have assessed the suitability of TSADs as a skeletal anchorage site in the mixed dentition period.
The palatal approach for TSADs has several advantages over buccally placed TSADs, especially in patients in the mixed dentition. Their smaller interradicular spaces and erupting teeth might increase the risk of root contact with buccally placed miniscrews, and the range of action could be limited. Surgical miniplates have been applied for sagittal correction, but placement of palatal plates might be more beneficial than surgical miniplates because they are flapless.
Favero et al applied miniscrews to the palate of a Class III patient in the deciduous dentition for maxillary protraction. In addition, Kook et al placed a palatal plate for molar distalization in adolescents with almost no side effects on the palatal soft tissue. Furthermore, Yu et al reported that based on finite element analysis, palatal plates were the only skeletal anchorages among several anchorage designs that produced bodily movement of the maxillary first molars.
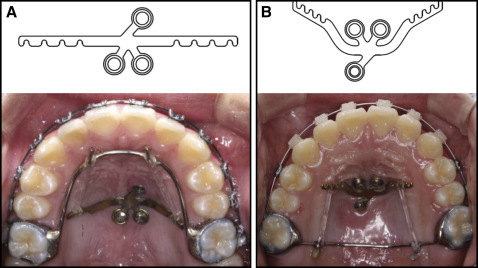
The modified palatal anchorage plate (MPAP) is a new fixed intraoral noncompliance appliance that can be used in its 2 versions: for distalization of the maxillary dentition in maxillary dentoalveolar protrusion ( Fig 1 , A ) and for protraction of the maxillary dentition to correct anterior crossbite ( Fig 1 , B ).
Case reports
Patient 1
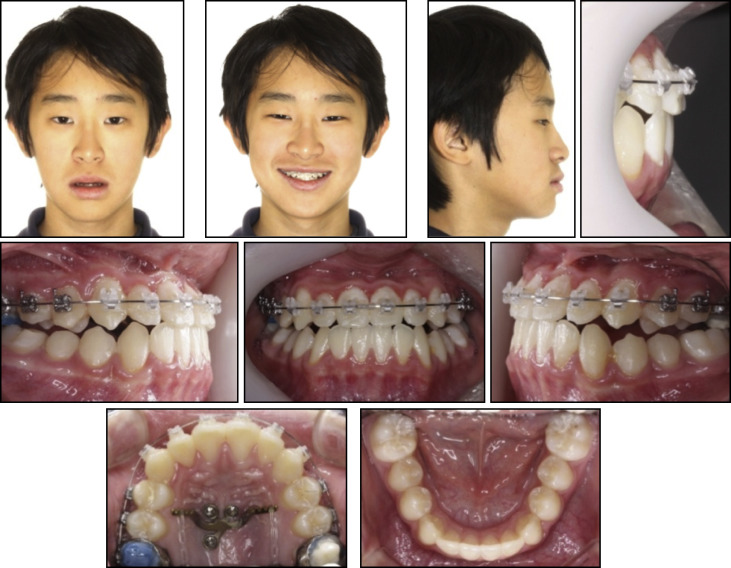
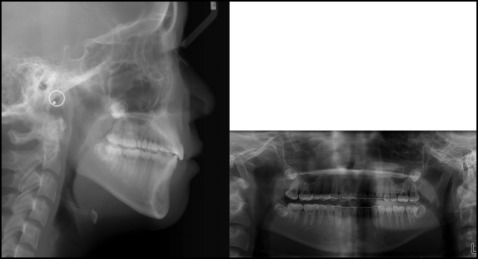
An 11-year-old girl had a chief complaint of protrusive lips. Clinical observation showed a large overjet (6.5 mm), moderate crowding in the maxillary and mandibular arches, a Class I molar relationship, and a convex profile ( Fig 2 ). According to the lateral cephalometric analysis, she had a skeletal Class II pattern (ANB, 4.3°) with proclined maxillary incisors (U1 to SN, 112°), and her lips were protrusive relative to the E-line. In the panoramic radiograph, eruption of the whole permanent dentition was seen, except for the third molars, which were in development ( Fig 3 ).


The treatment objectives were to obtain normal overjet and overbite, relieve crowding, and improve the patient’s profile. Extraction of 4 premolars was recommended, but the patient declined this option. Therefore, whole arch distalization of both the maxillary and mandibular arches was planned using an MPAP (Jeil Medical, Seoul, Korea). We placed 0.022-in slot brackets (OmniArch; Tomy, Tokyo, Japan). Archwires started with 0.016-in nickel-titanium and increased to 0.019 × 0.025-in stainless steel. After leveling of the maxillary arch, an MPAP was installed ( Fig 4 ).
Miniscrews (length, 8 mm; diameter, 2 mm; Jeil Medical) for the MPAP were placed in the 3 holes of the MPAP, 2 posterior and 1 offset anteriorly in the palate, slightly lateral to the midpalatal suture, under local anesthesia. A stainless steel palatal wire (1 mm [0.039 in] in diameter) with anterior hooks was soldered to the maxillary first molar bands, and approximately 250 g of distalizing force was applied on each side via elastomeric chains between the hooks and the MPAP lever arms. Class III elastics were then used for retraction of the mandibular dentition. After distalization for 16 months, the protrusion was resolved, and the MPAP was removed.
After 4 months of finishing and detailing with up-and-down elastics with a 0.016 × 0.022-in archwire, a fixed retainer was attached on the maxillary anterior teeth. Removable retainers were also delivered to secure the stability. Total treatment time was 32 months.
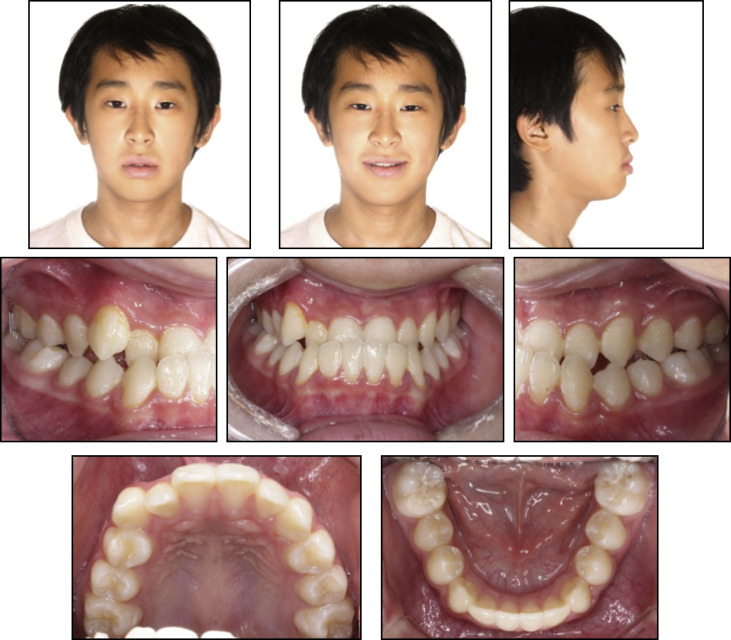
The posttreatment records show that the treatment objectives were achieved. The facial photographs show improved profile esthetics. Acceptable overbite and overjet were achieved, the Class I molar relationship was maintained, and the crowding was relieved ( Fig 5 ).
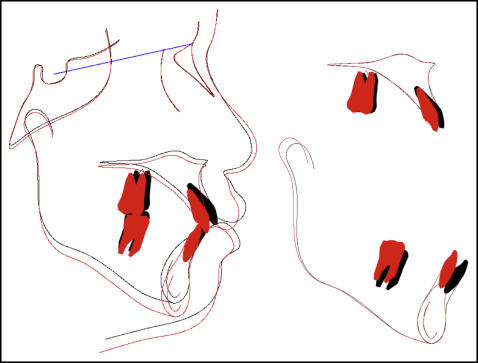
A posttreatment panoramic radiograph showed acceptable root parallelism with no significant sign of bone or root resorption. All 4 third molars were still developing ( Fig 6 ). The patient was referred to her general dentist and an oral surgeon for further evaluation of her third molars. Posttreatment lateral cephalometric analysis and superimposition showed skeletal changes with a slight backward movement of the maxilla but without a significant increase in her mandibular plane angle. To improve her lip protrusion, her maxillary and mandibular incisors were slightly retroclined (U1 to SN, 100.5°; IMPA, 82.0°) ( Fig 7 ; Table ).
| Measurement | Norm | Patient 1 | Patient 2 | ||
|---|---|---|---|---|---|
| Initial | Final | Initial | Final | ||
| SNA (°) | 81.6 | 81.1 | 80.5 | 79.8 | 82.7 |
| SNB (°) | 78.7 | 76.8 | 77.0 | 82.9 | 83.2 |
| ANB (°) | 2.5 | 4.3 | 3.5 | −3.1 | −0.5 |
| Wits (mm) | −2.0 | −0.5 | −2.5 | −10.6 | −7.0 |
| FMA (°) | 24.5 | 30.0 | 32.5 | 29.9 | 29.6 |
| Angle of convexity (°) | 4.0 | 10.0 | 8.0 | −6.5 | −2.5 |
| U1-SN (°) | 106.8 | 112.0 | 100.5 | 108.0 | 112.5 |
| U1 to A-Pog (mm) | 7.8 | 9.0 | 5.5 | 4.5 | 8.0 |
| IMPA (°) | 95.5 | 93.0 | 82.0 | 76.5 | 78.5 |
| L1 to A-Pog (mm) | 3.0 | 5.0 | 2.0 | 7.0 | 5.5 |
| Upper lip to E-plane (mm) | 1.0 | 3.5 | 0.5 | 0.0 | 1.8 |
| Lower lip to E-plane (mm) | 2.0 | 0.5 | 2.0 | 5.5 | 4.5 |
Patient 2
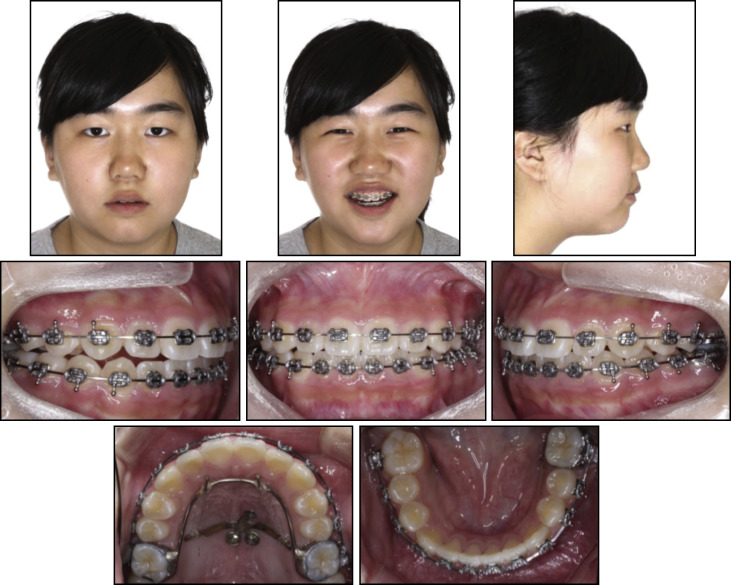
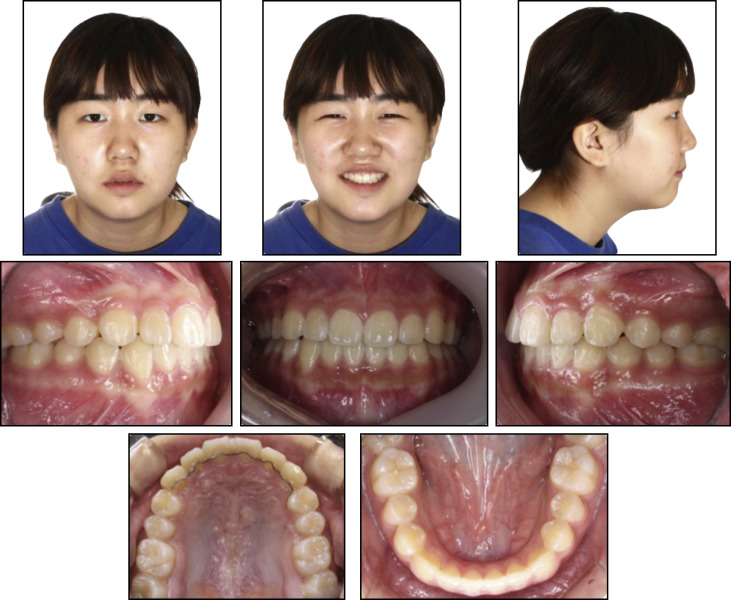
A 12-year-old boy had a chief complaint of chin protrusion. His previous dental history showed 6 months of orthodontic treatment with a facemask at age 8 years. There was no obvious familial skeletal Class III tendency. When his mandible was guided into centric relationship, a functional shift was detected because of anterior crossbites. The pretreatment facial examination showed a concave soft tissue profile caused by a prognathic mandible. In the clinical observation, anterior crossbites (−1.5 mm) and Class III molar and canine relationships were noted. He had a skeletal Class III relationship with a relative maxillary deficiency (ANB, −3.1°; Wits appraisal, −10.6 mm) ( Figs 8 and 9 ; Table ).
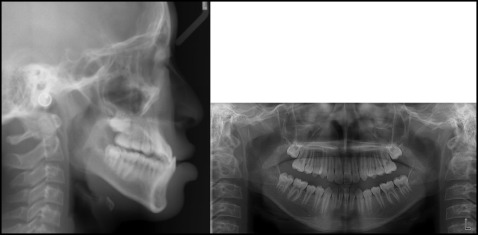
Phase 1 orthodontic treatment with protraction of the maxillary dentition was planned to correct his anterior crossbites. We placed 0.022-in slot brackets (OmniArch; Tomy) on the maxillary dentition only. The archwires started with 0.016-in stainless steel and increased to 0.019 × 0.025-in stainless steel. The miniscrews were placed in 3 holes of the MPAP, 2 anterior and 1 posterior in the palate, slightly lateral to the midpalatal suture, under local anesthesia. A stainless steel transpalatal arch (1 mm [0.039 in] in diameter) crossing the posterior palate with hooks was inserted between the maxillary first molar bands, and protraction force was applied on each side with elastomeric chains between the palatal arch hooks and the MPAP lever arms ( Fig 10 ). The elastomeric chains were changed monthly. Leveling and alignment were achieved simultaneously with protraction.