8
Risk factors and complications in bone grafting procedures
8.1 Introduction
Despite the high success rate of modern implantology and bone augmentation procedures, complications cannot be completely avoided. Thus, to avoid or detect them on time, potential risks and complications should be considered when making treatment decisions and conducting follow-ups. These possible complications have to be discussed with the patient before written surgical consent is obtained.
Peri- and postoperative complications are generally similar to other complications occurring after every surgical procedure, e.g. bleeding, swelling, pain or local infection.81,146,148,150, 157,173,178,209 In addition to these, other complications related to the grafting procedure might occur, since this grafting is accomplished in a contaminated area with, at times, compromising vascularization and differing regeneration potential. Other late complications can occur related to the volume stability of the grafted bone and surrounding soft tissue.
Complications may delay healing or even lead to total failure of the procedure, leaving a situation that can be even worse than that at the start of treatment.
8.2 Risk factors
Risk factors must be identified in advance to prevent or reduce possible complications. The literature contains detailed lists of absolute and relative contraindications for dental implant and grafting surgery;25,133,143 however, these have been significantly reduced over the last few years.36,218 Local and general risk factors are also described for bone augmentation procedures (Fig 8-1).
8.2.1 General risk factors
In addition to the anatomical conditions that relate primarily to the bone and soft tissue conditions, patient selection plays a crucial role. Sufficient oral hygiene may be complicated by extensive prosthetic constructions and requires special patient motivation. Moreover, due to its high surface free energy, titanium seems to accumulate more plaque than the natural tooth.171 Lack of compliance on the part of the patient regarding oral hygiene or even nicotine and drug abuse represent risk factors that significantly threaten the success of implant rehabilitation.33

Fig 8-1 Classification of general and local risks for bone augmentation procedures. The decision for any treatment will depend on the individual risk profile of the patient.
8.2.1.1 Influence of smoking
Smoking is a well-known risk factor for dental implants5 and is also an important risk factor for bone grafting procedures. Smoking reduces vascularization and has a negative influence on the microcirculation of the tissue, leading to flap necrosis and dehiscence, with exposure of the bone graft. Data from 64 onlay bone grafts revealed that smoking increases the risk of complications in bone grafting procedures.46 Mild complications such as hematoma, excessive swelling, inflammation or temporary paresthesia occurred in 50% of participants in the smoker group compared with 23.1% in the nonsmoker one. Major complications such as graft exposure or mobility were observed in one third of the smoker group compared with only 7.7% in the nonsmoker one.46 The present authors’ experience strongly underlines these results (Fig 8-2a to c).
Although smoking is a risk factor for implants and bone grafting, it seems to have no significant negative influence on sinus grafting procedures. A study involving 79 sinus lift surgeries revealed no relationship between postoperative complications in sinus lift procedures and smoking or a past smoking habit.46
However, regarding long-term results for implant failure in the augmented sinus, there is a significant difference. A literature review about sinus floor elevation and augmentation revealed a success rate of 46% to 82.9% after 3 to 5 years in smokers, and 93% to 100% in nonsmokers in the same period.86
Different surgical techniques are recommended to minimize the risks of tissue necrosis and exposure of the grafted bone in smoker patients. For this purpose, the two-layer wound closure approach using the pedicle subepithelial connective tissue periosteal flap and the tunnel technique, respectively, are described in Chapter 3.

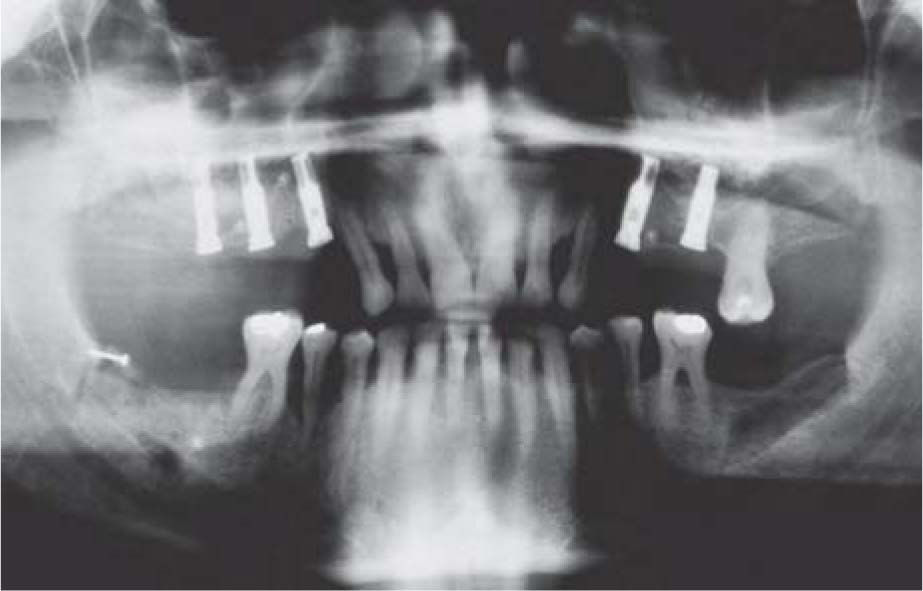
Fig 8-2a Apically repositioned flap for implant exposure after lateral bone graft in a heavy smoker patient.

Fig 8-2b Flap necrosis with exposed grafted bone. Note the nicotine coloration on the grafted bone.

Fig 8-2c Badly vascularized bone graft.
8.1.1.2 Diabetes
By common consensus, the insertion of endosseous implants in a diabetic patient, especially in combination with bone augmentation, is associated with an increased risk. Possible complications such as the increased incidence of severe bleeding, hematoma, infection, and early wound complications due to concomitant vascular defects can, in particular, lead directly to bone grafting failure. After prosthetic treatment, a predisposition to peri-implant inflammation is to be expected.152 Uncontrolled diabetes mellitus may limit the indication for implant and augmentation surgery and is discussed as a relative contraindication. The main problem in diabetic patients is the poor vascularization of the tissue due to the pathologic degeneration of the blood vessels. This leads to lower defense in the tissue against the oral flora, which results in a greater bone loss around the implants within the first 5 years.18
In a controlled, 5-year study of diabetic patients and bone augmentation procedures, double the number of complications was shown in diabetic patients compared with healthy ones. These were, in particular, primary soft tissue healing complications such as suture dehiscence and hyperplastic changes. Significant differences were not found in the long-term success rate or in clinical parameters such as probing depth and attachment level.18 Recent studies show a 5-year survival rate of implants of 94.4% to 97.3%. A correlation between implant failure and glucose levels could not be found.165 An influence on the healing of bone grafts can be assumed but could not yet be clearly established.
8.2.1.3 Corticosteroid medication
Practitioners are increasingly confronted with medically compromised patients requesting an implant rehabilitation. However, there are still no clear treatment guidelines, therefore many questions regarding the operational advantages and aftercare remain unanswered.19 It is well known that the long-term use of glucocorticoid induces osteoporosis and increases bone fracture risk by decreasing bone density. Therefore, bisphosphonate is recommended as an alternative.131,144 Obviously, steroid-induced osteoporosis mainly affects the skeletal system, and to a lesser extent, the jawbone. The removal torque of osseointegrated implants in the mandible was not significantly different with steroid medication than without it; however, this was not the case with skeletal bone.66
The prescription of the long-term use of corticosteroid medication has altered due to the reduced immune response and the healing cascade after a surgery; therefore, such patients are classified as high risk.45,194 However, a significant increase in implant loss in relation to steroid therapy was not confirmed in several studies.63,153,192 Although the healing reaction also depends on the concentration of the medication, due to the reduced immune response and the associated increased risk of infection, it is recommended to carry out bone grafting in such patients at the earliest 3 months after the discontinuation of corticosteroids. A high-dose corticosteroid medication (250 mg) in terms of a perioperative ‘one-shot’ prophylaxis medication for swelling in extensive bone grafting seems to have no negative impact on wound healing. Some authors recommend the systematic administration of antibiotics and glucocorticosteroids as part of sinus lifting medication.149
8.2.1.4 Bisphosphonate therapy
Today, bisphosphonates are an important treatment for osteoporosis, bone metastasis, Paget’s disease, and hypercalcemia.181 However, especially when a high dose is administered intravenously for the prevention or treatment of bone metastasis, bisphosphonates can lead to complex bone exposure, with necrosis of a large part of the jaw that is very difficult to treat (Fig 8-3a).72,187
The mechanism of bisphosphonate-induced osteonecrosis is mostly based on suppressing the activity of osteoclasts. Thus, it disturbs the natural balance of bone remodeling between osteoblasts and osteoclasts, since the former are not really affected by the treatment.71,145 New bone formation continues to occur through osteoblast activity, but without the removal of old bone by the suppressed osteoclasts. In time, the bone will become very dense, significantly reducing the space for the blood vessels, which will make the bone very vulnerable to infection. Since the surgical treatment in the oral cavity occurs in the presence of the oral flora, a contamination of the wound can lead to severe bone infection, with bone necrosis and exposure due to a lack of vascularization.
In a literature study covering the years 1966 to 2006, attempts were made to prove a relationship between osteonecrosis and the use of oral bisphosphonates, alendronate, ibandronate, etidronate, clodronate or pamidronate for the treatment of osteoporosis. About 70% of the very rarely occurring osteonecroses (less than 2%) were related to the mandible – significantly more than for the maxilla. Nearly 80% of patients were older than 60 years, and only 13% of them were male. The release of osteonecrosis in 80% of the cases was in oral surgery. A clear correlation between the duration of the medication and the occurrence of osteonecrosis of the jaw could not be determined. Considering the millions of patients using bisphosphonates to treat osteoporosis, the relative prevalence of osteonecrosis is relatively limited, in the opinion of the authors. This is not the case when a high dose of bisphosphonate is administered in the prevention or treatment of bone metastasis, where the risk of osteonecrosis is much more significant.206
Depending on the indication and its relationship to the dose of the administered bisphosphonate, different decisions for an implant treatment (with or without bone augmentation) can be taken after performing an individual risk profile of the patient. While intravenously administrated bisphosphonate for the treatment and prevention of bone metastasis of breast or prostate carcinoma or other serious disease (e.g. plasmacytoma) represents an absolute contraindication for any implant treatment, treatment with low-dose or oral bisphosphonate is considered a relative contraindication. Therefore, after an individual risk profile – including the general health of the patient, the healing capacity of the oral tissue (e.g. normal healing without any disturbance after tooth extraction, whether the patient is a smoker, whether the patient is on regular medication that influences bone or soft tissue healing) – it is possible to discuss an implant treatment, even with extensive bone augmentation (Fig 8-3b to k), especially in cases where no alternatives exist.120

Fig 8-3a Bisphosphonate-associated osteonecrosis of the jaws (BP-ONJ) showing exposed white and necrotic bone in a patient under intravenous bisphosphonate treatment for prostate carcinoma.
Bisphosphonate-induced osteonecroses are described for both intravenous and oral administration of the drug; other related issues include the type of administrated bisphosphonate, its dose and concentration, and the treatment duration. The majority of osteonecrosis cases, however, involve intravenous administration.72 According to a study by Grant et al,72 even if the implant success is not significantly affected by oral bisphosphonate medication, osteonecrosis occurrence after implant treatment is reported.206 Often, patients over 55 years of age with limited health are affected.38
Fig 8-3b Important bony defect in the posterior maxilla in a patient who has been under clodronate treatment for 5 years (Bonefos; Bayer Oy, Turku, Finland; 800 mg oral/week).

Fig 8-3c Three-dimensional bone augmentation in combination with sinus grafting through a tunnel approach.

Fig 8-3d Postoperative radiograph documenting the amount of vertical bone augmentation in the right maxilla and the bone harvested area in the right mandible.

Fig 8-3e Implant insertion in the grafted area 4 months postoperatively: very low remodeling with no resorption of the grafted bone, which still has a white color.

Fig 8-3f Implant and bone exposure 2 months after implant insertion.

Fig 8-3g Removal of the exposed thin cortical layer, insertion of healing abutments, and soft tissue augmentation with a palatal pedicle connective tissue flap.
Fig 8-3h Photodynamic decontamination with the Helbo system.

Fig 8-3j Control radiograph 3 years postoperatively confirming the stability of the grafted bone.

Fig 8-3i Wound closure.

Fig 8-3k CBCT of the augmented area 10 years postoperatively documenting the stability of the grafted bone.
In general, patients should be informed and made aware of possible complications after oral surgical procedures. Currently, there are no effective and predictable treatment options in case of bisphosphonate-associated osteonecrosis of the jaws (BP-ONJ). The bone exposure can persist for years and may result in a significant weight loss in the patient due to the difficulty of eating.38 In an individual case, a wound healing disturbance that occurred after implantation was successfully treated with systemic antibiotics, local antiseptic rinses, and aggressive defect management with local tetracycline. Finally, according to this case report, a bone block grafting procedure was performed after medication with oral bisphosphonates.206
8.2.1.5 Bone systematic diseases
Bone systematic diseases can have a negative impact on the osseointegration of endosseous implants and their prognosis. To date, no long-term study has clearly defined a negative prognosis or even a contraindication for implantation in the case of established osteoporosis.65,140 A recent study correlates increasing complications such as graft resorption, inadequate graft healing, and a higher implant failure rate in augmented areas in cases of osteoporosis. Despite this, osteoporosis is not seen as an absolute contraindication for implant therapy.57 Rather, the side effects of corticosteroid or bisphosphonate therapy seem to cause the occurring complications.63,187,206 Other studies, in turn, assume that osteoporosis affects the body skeleton but not the jawbone.41,63 However, bone system diseases causing circulation problems and hypoperfusion of the bone such as Albers-Schönberg disease and Paget’s disease are still an absolute contraindication for bone augmentation and implantation.20,89,210
8.2.1.6 Hemorrhagic diathesis
Hemorrhagic diseases can be hereditary or acquired. Since patients with severe hereditary diseases can mostly be treated before surgery through substitution of the missing factor, acquired hemorrhagic diseases are usually caused by anti-thrombosis medications. Anti-coagulant therapy is always connected with a risk of increased bleeding tendency in all kinds of surgery. The traditional approach calls for the cessation of those medications; however, there is an increasing risk of life-threatening thromboembolism. The discontinuation, alteration or reduction of anticoagulation therapies increases the potentially fatal risk of thromboembolic events. The latest conclusions are that it is better not to interrupt the anticoagulant medication when coumarin, aspirin, or heparin are administered, but to use local methods of hemostasis.1,47,186
In general, dental surgeries are assessed as having only a low risk of dangerous severe bleeding.85 However, it is important to determine whether sufficient wound care is possible, e.g. through suture care or compressibility by bolting or tamponing in the case of bone bleeding. In addition, intraoperative block anesthesia should be avoided to prevent heavy bleeding in the tissue through the injury of important blood vessels.
A central question is the compressibility of the wound, which is usually possible in different areas of the jaws except the floor of the mouth, the maxillary sinus, and the retromaxillary space. Furthermore, in the case of infected wounds or abscesses, no primary wound closure is sought, and therefore the risk of bleeding may increase.
For procedures involving a greater risk of bleeding as well as extensive bone grafting – especially in lateral and vertical augmentation, when multiple tension-free wound closure is performed with many releasing incisions of the periosteum – it is recommended that a highly experienced specialist provides such a treatment, including the possibility of postoperative observation under hospitalization conditions. Local homeostasis methods are recommended such as (bipolar) vessel coagulation, collagen fleece, fibrin glue, and a compression splint (especially for the maxillary and palatal area).81
Platelet aggregation inhibition
Platelet aggregation inhibitors are mainly used for primary (acetylsalicylic acid) and secondary prevention of heart attack and stroke because their effect extends mainly to the arterial part of the vascular system.14,69 There is a 1.5-fold increase in the risk of bleeding complications during low-dose acetylsalicylic acid medication (75 to 100 mg) during general surgery;30 studies relating to dental surgery showed only a weak, if any, correlation.69 Furthermore, none of the bleeding was life threatening and could easily be stopped through the use of local measures. In contrast, the risk of a cardiovascular event increases threefold when acetylsalicylic acid is discontinued.199 Discontinuation of acetylsalicylic acid prior to dental surgery is therefore not necessary and should not be performed.184
Thienopyridines (Clopidogrel, Plavix, Prasugel, Efient)
The mechanism of thienopyridines is based on an irreversible inhibition of the platelet ADP-P2Y12 receptor. The indications are secondary prophylaxis after ischemic insult and myocardial infarction, peripheral arterial disease, and secondary prevention of cardiovascular diseases as well as after the insertion of stents. The plasma half-lives are between 6 to 15 h.54,69,163,199
Patients on Clopidogrel have an up to twofold increased relative risk of prolonged rebleeding after oral surgery,69 with no impact on morbidity and mortality.199 Prasugel leads to more pronounced platelet inhibition than Clopidogrel, with fewer interindividual fluctuations.69,163 The discontinuation of such medication, especially in high-risk patients, can lead to severe and dangerous cardiovascular disorders.
For simple dental surgeries in the compressible area, monotherapy with Clopidogrel and Prasugel should be continued. For dental interventions with a higher risk of hemorrhage under monotherapy, treatment by specialists or under hospitalization should be considered. If a short-term discontinuation is possible after consultation with the treating cardiologist, it is advisable to discontinue the morning intake prior to the dental surgery.14,69,184
Ticagrelor (Brilinta)
The effect of this medication is a reversible inhibition of the ADP-P2Y12 thrombolytic receptor. It is indicated for dual therapy in combination with acetylsalicylic acid to prevent atherothrombotic events such as myocardial infarction or apoplexy. The plasma half-life is about 7 to 12 h.54,69,163,199
Monotherapy with platelet aggregation inhibitors, unlike dual antiplatelet therapy, has little correlation with prolonged bleeding events after dental surgery. For smaller procedures, e.g. multiple extractions, flap scars, alveoloplasties and biopsies, no correlation could be found between the type of intervention and the occurrence of rebleeding.69
Frequently, two-platelet aggregation inhibitors are used in patients after stent placement: primarily acetylsalicylic acid and a thienopyridine (Clopidogrel, Prasugrel or Ticagrelor). Acetylsalicylic acid is usually formulated for life in these patients. Thienopyridines are also recommended in cases of bare metal stents for 4 weeks and for coated drug-eluting stents for at least 6 months.74 In patients with acute coronary syndrome, dual platelet aggregation inhibition with Ticagrelor is prescribed for at least 12 months. In general, an extension of the individual case decision remains reserved.74 This, in turn, can lead to significant postoperative bleeding complications even after dental surgeries.69 The main risk of developing stent thrombosis (hazard ratio: 89.9), which causes fatal myocardial infarction in up to 75% of cases, is related to the discontinuation of dual platelet aggregation inhibition.91,184 In patients with a newly implanted stent, the discontinuation of platelet aggregation increases mortality by 20% to 40%.105 Therefore, elective dental procedures should not take place until dual platelet aggregation is complete.74 Even in an emergency situation, the anti-aggregator medication cannot be changed. The use of hemostyptic measures such as sutures, the application of tranexamic acid, and local pressure has already shown good results in the prevention of bleeding complications.180
Oral anticoagulation
Based on a recent systematic review, it has been shown that dental surgeries under continuous therapy with phenprocoumon (Marcumar) or warfarin (Coumadin) are possible in the therapeutic area.104 However, even with strict restrictions – international normalized ratio (INR) of < 4 and the use of hemostatic measures – increased bleeding can be expected but without fatal risks, as is the case when anticoagulant medication is discontinued.60,104
The introduction of newer oral anticoagulants (NOACs) presents new possibilities for treatment protocols that simplify the treatment plan of such patients.54,100,184,220
Dabigatran (Pradaxa)
The mechanism of this medication is based on a competitive and reversible binding to thrombin, which blocks the conversion of fibrinogen to fibrin. Indications include prevention of stroke and systemic embolism in nonvalvular atrial fibrillation, the treatment and prevention of deep vein thrombosis and pulmonary embolism, and the primary prevention of venous thromboembolic events after elective hip or knee replacement surgery. The plasma half-life of this orally available NOAC is 12 to 17 h, and its maximum anticoagulative effect occurs 2 h after ingestion.83,126
For simple dental-surgical procedures in the compressible area, dabigatran therapy can either be discontinued for 1 day or continued. Based on general surgery data, discontinuation of dabigatran is recommended for about 2 days preoperatively prior to intervention with high bleeding risks. However, this discontinuation should not exceed 1 day for all kinds of oral surgeries. As far as any bleeding occurring within the individual postoperative observation period is concerned, all NOACs should be restarted immediately after surgery.83,184
Rivaroxaban (Xarelto), apixaban (Eliquis), and edoxaban (Lixiana)
The effect of this group of drugs is a direct, reversible, and selective inhibition of factor Xa. Indications include the prevention of stroke and systemic embolism in nonvalvular atrial fibrillation, and the treatment and prevention of deep vein thrombosis and pulmonary embolism. The plasma half-lives of these NOACs are 7 to 14 h.
For simple dental-surgical procedures in the compressible area, therapy with direct factor Xa inhibitors should be continued. Elective dental surgeries with a higher risk of bleeding under direct factor Xa inhibitors should not be performed earlier than 12 to 24 h after the last dose, depending on which drug is usually used. Urgent dental surgeries with a higher risk of bleeding less than 12 to 24 h after the last dose has been taken should be delayed or the patient should be sent to a specialist clinic. Generally, it is advised to pause medication 1 to 2 days before invasive procedures.83,182,184
In a single-blind, prospective, case-control study, the bleeding events of patients treated with rivaroxaban after the insertion of dental implants were compared with a group without hematologic features who had also received implants. The differences between the groups were not significant.70 When co-administered with rivaroxaban (Xarelto) and antiplatelet agents, the risk of bleeding increases greatly – and for this reason, special care is required in such cases.104 If no bleeding has occurred within the individual postoperative observation period, the next intake of direct factor Xa inhibitors, as with all NOACs, should be immediately after surgery.83,182,184
In a study in which patients on anticoagulant treatment had, on the morning of surgery, INR values of < 5.5, and an atraumatic surgical technique was carried out, only 1.96% of the patients developed severe bleeding complications.61 In another study on oral anticoagulant therapy, no significant difference was established between a group of patients with INR values of 1.5 to 1.99 and another group of patients with INR values of up to 3.5.24 In all these cases, local hemostatic measures were carried out.
Bridging
For bridging, vitamin K antagonists should be discontinued about 2 to 4 days preoperatively. Subcutaneously administered, low-molecularweight heparin (LMWH) or intravenously administered unfractionated heparin is used when the INR of the therapeutic range is undershot; a higher efficiency was demonstrated for LMWH.203 If the postoperative risk of bleeding is reasonable, oral therapy with vitamin K antagonists will usually resume on the first day after the procedure, with heparins discontinued only when the INR is > 2.13. Bridging with heparins may be useful in vitamin K antagonists and NOACs, but not in antiplatelet agents.
However, due to the increased risk of thrombosis, the practice of bridging is currently very controversial and should not, in the present authors’ point of view, be carried out any longer.
8.2.1.7 Influence of vitamin D on bone healing and osseointegration
Vitamin D plays an important role in the regulation of phosphocalcic metabolism as well as in a large number of biologic and metabolic processes. The prevalence of vitamin D deficiency in the population is high and is associated with impaired peri-implant bone regeneration.53
Following the failure of a bone graft or an implant placement, biologic abnormality is rarely considered to be a possible cause. Vitamin D is a key factor for linking innate and adaptive immunity. Both of these factors are compromised under the conditions of vitamin D deficiency. Therefore, vitamin D deficiency slows implant osseointegration and increases the risk of graft infection. Vitamin D is also involved in immune function, and therefore also in allergic reactions.40 Since osseointegration depends on bone metabolism, low levels of vitamin D in the blood may negatively affect bone formation around dental implants.
The importance of vitamin D supplementation on osseointegration is still largely unclarified, whereas its influence on peri-implant bone regeneration has been investigated. Although its depletion in an animal study in rats led to a decrease in cortical bone–implant contact, the rate of apposition in the peri-implant bone remained unchanged. It was concluded that vitamin D deficiency had a negative impact on peri-implant bone formation in the cortical bone, although this can be compensated for by appropriate supplementation.53
An association between vitamin D deficiency and early dental implant failure is not properly verified, but its role in osteoimmunology has been discussed. Two case reports on vitamin D deficiency and early implant failure showed successful implant placement after vitamin D supplementation.64 However, the efficacy of vitamin D supplementation on osseointegration of implants remains controversial and requires further investigation.
8.2.1.8 Influence of cholesterol (dyslipidemia) on bone growth and healing
Following the failure of a bone graft or an implant osseointegration, the hypothesis of a biological abnormality is rarely considered as a possible cause.
A high-fat diet inducing hyperlipidemia has been associated with the pathophysiology of major diseases such as atherosclerosis and osteoporosis. A high-fat diet has significant adverse effects on bone, including lower bone density, volume, and strength. Statins (drugs that lower serum cholesterol levels) have beneficial effects on bone metabolism. Since the host’s bone quantity, quality, and healing potential play a crucial role in the osseointegration of dental implants, it is hypothesized that hyperlipidemia may negatively affect implant osseointegration.110 It is reported that hyperlipidemia affects the quality and density of bone, and adversely affects wound healing. It was found that hyperlipidemia may negatively affect implant stability and so decrease peri-implant bone regeneration.197 Excess low-density lipoprotein cholesterol (dyslipidemia) is responsible for slower bone metabolism and lower dental implant osseointegration.40 The results of an animal study showed that a high-fat diet resulted in significantly increased implant loss; it also decreased the formation and strength of the bone-to-implant interface. The results supported the hypothesis that a high-fat diet can significantly compromise osseointegration, causing poor outcome in dental implant therapy.110 In another study that aimed to verify the effect of hypercholesterolemia on implant and bone augmentation failures, the results showed that high total serum cholesterol levels tended to increase graft failure rates but did not influence the failure rate of implants.198
8.2.1.9 Infection prophylaxis and penicillin allergy
In cases of simple and normal implant placement without bone augmentation, recent protocols have recommended short-term antibiotic prophylaxis in the form of a perioperative prophylaxis, with the administration of one-shot antibiotic directly before surgery and sometimes another dose after 6 h. This seems to be beneficial for reducing dental implant failures. However, if there is a need for additional bone grafting, the situation becomes different: As bone grafting procedures are carried out using autogenous free bone grafts, allografts, and/or different biomaterials in the contaminated oral cavity, the use of prophylactic antibiotics is essential for 7 to 10 days until complete wound healing in order to prevent infection and wound complications. Comparison studies have demonstrated a high infection rate when bone grafting procedures were carried out without prophylactic antibiotics in comparison with those with antibiotics.81,134
For many decades already, antibiotics from the penicillin family (beta-lactam antibiotics) have generally been the best and most widely used for both the prophylaxis and treatment of infections of the oral cavity. Especially, penicillin in the form of the narrow-spectrum antibiotics such as penicillin V (oral application) or penicillin G (intravenous application) are very effective against pathogens of the oral cavity. They also present the lowest toxicity in comparison with other antibiotics. Broad-spectrum penicillin, e.g. amoxicillin, is generally used in surgeries affecting not only the oral cavity but also the neighboring areas such as the sinus (sinus lift procedures). It is also used to treat heavy infections. However, the main problem with this family of antibiotics is allergy. About 15% of patients today are allergic to antibiotics from this family. Clindamycin has been used for many years as an alternative antibiotic in case of penicillin allergy but has never reached the efficiency of penicillin. The odds of failure for implants placed in penicillin-allergic patients were 3.1 times higher than those in non-allergic patients.62 For immediate implant placement, penicillin-allergic patients had a failure rate 10 times higher than the non-allergic cohort.62 This is mostly due to increasing resistance against clindamycin: Penicillin-allergic patients treated with clindamycin presented almost four times the risk of suffering dental implant failure.179 Prophylactic clindamycin therapy following sinus augmentation procedures also seems to be a risk factor for infection and loss of grafting material following these surgeries. A recent publication reports on infection of the graft material inside the sinus floor, with the development of an abscess at the site of surgery 4 to 6 weeks postoperatively, and a buccal fistula with pus draining 5 to 8 weeks postoperatively, in about 30% of the patients treated with prophylactic clindamycin for sinus lift procedures. A common process in all patients in this study was the administration of clindamycin (1.2 gr/day for 10 days) due to self-reported penicillin allergy.121
Unfortunately, there are no effective alternatives to date for clindamycin in case of penicillin allergy. New antibiotics from the fluoroquinolone family, e.g. ciprofloxacin or moxifloxacin, have been discussed as possible alternatives, but it is recommended to at least limit their use because of severe unintended side effects (e.g. Achilles tendon rupture) and adverse reactions. Therefore, penicillin-allergic patients are classified today as risk patients for bone augmentation procedures.
Preoperative antiseptic mouth rinses with 0.2% chlorhexidine gluconate solution significantly reduced the number of microorganisms before bone grafting procedures.215 The key role played by the inhibition of plaque formation for 2 to 3 weeks postoperatively is well known in the use of membranes and is highly recommended, also after bone grafting.31,32,46
8.2.2 Local risk factors
8.2.2.1 Radiotherapy
Radiotherapy involving the jawbone is often seen as a contraindication for implant treatment42 because it destroys all cells with a high mitosis rate. Unfortunately, this involves not only the tumor cells but also other healthy areas, e.g. the bone marrow. In addition, radiation reduces the vascularization of the bone through radiation-induced degeneration of the blood vessels, making the bone more vulnerable to infection and bone necrosis (osteoradionecrosis). Especially as patients after tumor surgery and extensive resections of bone and soft tissue mostly require dental implants to give them back function and esthetics, certain recommendations and conditions were developed to allow for implant-supported restorations in these situations. These recommendations focus on reducing the risk of complications and osteoradionecrosis in cases of implant treatment. A decisive factor in the irradiated jaw is the amount of the total dose, which has to be under 60 Gy (gray), administered in small doses (4 to 5 Gy) for several weeks. It is also recommended to wait a minimum of 1 year after radiation therapy before performing implant surgery under antibiotic prophylaxis, which has to begin in this special situation at least 24 h before the surgery. Hyperbaric oxygen therapy seems to have a positive influence on the prognosis of such a treatment.9 Thus, under certain conditions, good results are possible even in this challenging situation.7,9,96 If bone augmentation is necessary, it is recommended to harvest bone from a nonirradiated area, optionally the iliac crest.
8.2.2.2 Periodontitis
Many studies have shown that peri-implant tissue affected by peri-implantitis can have similar clinical and bacteriologic characteristics of the natural dentition affected by periodontal disease.17,124 The relationship between rapidly progressive periodontitis and implant failure is also described in the literature.139 Typical periodontal bacteria such as bacteroides, fusobacterium, gram-negative rods, actinomycetemcomitans, and capnocytophaga were detected in conjunction with implant losses.86,151
In terms of long-term success, apart from patient instruction and motivation, it is mandatory before an implant and bone augmentation procedure to complete all periodontal treatments to reduce the concentration of intraoral bacteria. Furthermore, after the completion of treatment, such periodontally compromised patients must remain in a regular maintenance program. If these criteria are followed, it is possible to achieve similar long-term results in such patients as for periodontally healthy patients, even in combination with intensive bone augmentation procedures.108
Severe periodontal diseases are usually associated with significant bone loss. In the case of vertical bone augmentation following tooth loss caused by periodontal disease, the neighboring teeth of areas to be grafted may also be affected by bone loss. Denudated roots caused by periodontal disease, with or without deep periodontal pocketing, always present a high risk for bone grafting because no bone is able to grow over the contaminated and dead cementum. In addition, the grafted bone can be infected through the periodontal pocket. Alternatives must be considered whenever the denudated teeth have to be removed before bone augmentation, or another treatment choice should be made that does not involve bone grafting. Bone augmentation only has a good prognosis if the neighboring roots are covered by bone (Figs 8-4a to c). An exception is the situation where the neighboring teeth have lost the bone that covers the roots due to trauma: in this situation, a periodontal attachment is normally still present without any pathologic pocketing, and so a bone grafting procedure can be successfully performed (Fig 8-4d to j).
Fig 8-4a Vertical bony defect of more than 8 mm, but the roots of the neighboring teeth have a thick bony coverage.

Fig 8-4b Three-dimensional bony reconstruction with mandibular grafts.

Fig 8-4c Clinical situation demonstrating an almost complete regeneration of the defect 3 months postoperatively.

Fig 8-4d Vertical bony defect with the almost completely denudated root of the neighboring lateral incisor. The tooth and bone loss were both caused by trauma. Clinically, there is no pathologic pocket on the lateral incisor and its attachment is intact.

Fig 8-4e Reconstruction of the buccal and palatal bone walls with mandibular bone blocks.

Fig 8-4f The box is filled with autogenous bone chips.
Fig 8-4g Palatal connective tissue flap for a two-layer closure and improvement of the soft tissue volume.

Fig 8-4h Implant insertion 3 months postoperatively in the well-regenerated bone. The root of the lateral incisor is now well covered by bone due to its vital attachment.

Fig 8-4i Clinical appearance with the restored implant.

Fig 8-4j Radiographic control 4 years postoperatively demonstrating the stability of the grafted area.
8.2.2.3 Bone quality and quantity
The possibility of oral rehabilitation with dental implants depends primarily on the alveolar bone. A prerequisite for osseointegration of endosseous implants is the primary stability of the implant,28 which depends on the bone quantity and quality of the implant site.3
Four classes of bone are distinguished to describe the bone quality:129
 Class D1: homogeneous compacta.
Class D1: homogeneous compacta.
 Class D2: compact bone surrounds wide-meshed spongy bone.
Class D2: compact bone surrounds wide-meshed spongy bone.
 Class D3: thin cortical bone surrounds dense cancellous bone.
Class D3: thin cortical bone surrounds dense cancellous bone.
 Class D4: thin cortical bone surrounds loose cancellous bone.
Class D4: thin cortical bone surrounds loose cancellous bone.
Besides different bone qualities, different jaw shapes are clinically observed. Thus, bone atrophy of the jaws (resorption) is divided into five classes:130
 Class A: almost totally preserved alveolar ridge.
Class A: almost totally preserved alveolar ridge.
 Class B: slight resorption of the alveolar ridge.
Class B: slight resorption of the alveolar ridge.
 Class C: advanced resorption of the alveolar ridge to the basal bone.
Class C: advanced resorption of the alveolar ridge to the basal bone.
 Class D: incipient resorption of the basal bone.
Class D: incipient resorption of the basal bone.
 Class E: extreme resorption of the basal bone.
Class E: extreme resorption of the basal bone.
Appropriate implant–prosthetic treatment concepts can be planned through combining the classes of bone quality with those of bone atrophy.130 For both jaws, bone quality classes D2 and D3, in combination with resorption classes B and C, are considered therapeutically unproblematic because in these cases the primary stability of the implant is easily accessible. In contrast, the combination of bone quality class D4 and resorption class A causes problems in terms of the primary stability of the implant, unless additional measures are taken to improve bone quality such as the condensation technique with osteotomes. Resorption classes D and E of the mandible, in conjunction with bone quality classes D1 and D2, are considered to be particularly problematic due to the effort involved in penetrating the extremely hard cortical bone for implant site preparation and implant insertion, which may be connected with an overheating of the jaw bone, leading to the so-called Burned Bone Syndrome114. In addition, usually only short implants are placed in these cases, leading to an unfavorable implant–crown ratio.
Resorption class D and E are especially problematic in the maxilla because, as a result of the vertical bone loss, it is often much more difficult to meet patients’ esthetic and phonetic requirements. An implant rehabilitation is much more complex in these cases due to the frequent need for extensive bone augmentation.115 The same applies to the ridge width: The implant should be surrounded by the insertion of at least a 1- to 2-mm–thick peri-implant bone lamella. Otherwise, as a result of unavoidable postoperative bone resorption, implant surfaces will already be exposed after a short time. If this condition is not met prior to implant bed preparation, appropriate augmentation procedures will have to be used such as lateral augmentation, bone splitting, bone spreading or alveolar ridge extension plastic.118
Under bone augmentative measures, the success of transplantation depends on the revascularization of the graft. The prognosis of a transplant is always determined by the quality and intensity of revascularization.141,158 The faster the vessel connecting the transplant, the better its regeneration and survival. The regeneration potential of the recipient site plays a crucial role.56
Multi-walled bone defects are desirable as they promote the closest possible and most extensive contact with the graft. Single-walled recipient sites are more difficult to regenerate. Also, failed augmentation with biomaterials may considerably limit the regeneration potential of the recipient site. Reduced regeneration potential arises from the fact that partially osseointegrated, unabsorbed biomaterial remains on the bone surface of the recipient site and blocks the revascularization and thus the regeneration of bone grafts (Fig 8-5a). These situations have to be treated through substantial removal of the biomaterial (Fig 8-5b).

Fig 8-5a Clinical appearance after the failure of augmentation with bovine material. The remaining parts of the material (arrows) should be removed before a new augmentation is performed.

Fig 8-5b The exposition of the roots of the neighboring teeth is due to the chronic infection of the augmentation material. In this situation, no new bone is able to grow over the dead cementum of the neighboring teeth. The potential of vertical bone augmentation is therefore reduced and is only possible up until the bone level of the neighboring teeth.
8.2.2.4 Soft tissue quality
The quality of soft tissue plays a central role in implant therapy. Therefore, a preoperative inspection of the surgical field should be performed. It is a necessity to obtain adequate soft tissue coverage of the implant site and the grafted bone. Later, peri-implant soft tissue has to be augmented, mostly during implant exposure surgery, to guarantee the long-term stability necessary for esthetics and function.21,143 Trauma, severe periodontal lesions as well as several surgeries can sometimes lead to soft tissue defects with significant scar tissue (Fig 8-6a to c). Similarly, the soft tissue situation can significantly deteriorate due to tumor resection and the associated soft tissue reconstruction with skin grafts.84,162 Thus, a tension-free adaptation to cover implants or bone grafts may be problematic. Additionally, decreased vascular supply to the flap and the scarring of the periosteum lead to poor bone regeneration by the periosteal cells (Fig 8-7a). Especially after failed augmentation with biomaterials, the soft tissue is extremely scarred, with a very poor blood circulation (Fig 8-7b). The use of membranes, especially in this indication, is not recommended because additional foreign bodies increase the already high risk of dehiscence, with subsequent infection.129
The soft tissue in the esthetic region represents a major challenge for the implantologist. As early as during the planning phase, the expectations and desires of the patient must be considered as well as the anatomical morphology of the area to be treated such as the smile line, the papillae, and the soft tissue biotype. The thickness of the gingiva plays an important role, since certain surgical techniques can be performed satisfactorily only when sufficiently thick gingiva is present.4,143
Fig 8-6a Poor tissue quantity and quality after the failure of a guided tissue regeneration (GTR) in the anterior area.

Fig 8-6b Soft tissue augmentation with a palatal pedicle connective tissue flap.

Fig 8-6c Clear improvement of the anterior soft tissue.

Fig 8-7a Extremely poor soft tissue quantity and quality after several attempts at guided bone regeneration (GBR) with bovine material: Scar tissue and poor vascularization increase the risk of soft tissue necrosis.

Fig 8-7b Similar situation as described in Fig 8-7a, but with additional denudation of the neighboring roots.
8.3 Intraoperative complications
Various complications can occur during the surgical procedure, including the general complications that are possible with every surgery, e.g. pain due to anesthesia failure, heavy bleeding, and specific complications directly related to the type of surgical procedure.
The preoperative diagnosis plays a central role in the prevention of complications. Palpation of the bony structures is routine for obtaining information about the morphology of the potential donor site.80,119 Similarly, the soft tissue ratios must be examined. Access to the surgical site and wound closure can be made more difficult by scar tissue, which can also negatively affect wound healing.84,162
The imaging standard diagnostic procedure begins with the preparation of a panoramic radiograph to obtain the position of the nerves, the mental foramina, and the tooth roots. In addition, if necessary, dental radiographs, lateral cephalometric radiographs, computed tomography (CT), or cone beam computed tomography (CBCT) can be performed. In addition, the radiopacity allows conclusions to be drawn regarding bone quality.
8.3.1 Burned Bone Syndrome
Drilling in the bone for implant bed preparation must be carried out under very good cooling, especially when the bone is particularly cortical and dry. External and, if possible, internal cooling of the burs can prevent the overheating of the bone, which already occurs at about 56°C. High pressure on the bone during the drilling procedure should be used very carefully as it can be very risky for overheating the bone, since such burs have a wide surface adherence to the bony walls with very narrow cooling canals. The narrow cooling canals can easily become obstructed with bone powder, which results in an increase in temperature. An overheating of the bone will burn the bone and can lead to Burned Bone Syndrome.114 This syndrome includes several symptoms that can be attributed to thermal damage to the bone through drilling or during implant placement. The observations indicate a predisposition for the development of this syndrome in the application of long-screw implants (15 and 18 mm in length) in very cortical and dense bone. Clinical symptoms consist of postoperative continuous complaints in the surgical area that last longer than a month. In addition, recurrent swelling and tenderness have been observed.
Radiographically, demarcated peri-implant bone loss in the apical region similar to the apical granuloma on natural teeth can be detected as early as 8 weeks after implant placement (Fig 8-8).

Fig 8-8 Comparison between radiologic appearance of Burned Bone Syndrome (BBS) with other bone density changes (from left to right): a) burned bone, b) non-osseointegration, c) peri-implantitis, d) peri-implantitis with complete bone loss, e) nonpathologic overextended preparation of the implant bed.
Burned Bone Syndrome is initially treated with broad-spectrum antibiotics – amoxicillin 2 g/day and metronidazole (Clont) 750 mg/day for 1 week. In case of nonremission or aggravation of the symptoms, surgery in the form of an apical cleaning with the removal of the granulation tissue, decontamination, and possible grafting of the affected area should be carried out. In cases where the buccal bone is still present, the bony lid approach is recommended to preserve the bone walls and enhance the healing (Fig 8-9a to j). In cases of nontreatment or treatment that occurs too late, the aggravation of the symptoms can range from recurrent abscesses to a spontaneous intra- or extraoral fistula. In such situations, it is recommended to remove the implant (Fig 8-10a to f). Apart from trephine drills, autogenous bone can also be obtained during implant bed preparation with conventional twist drills without cooling at low speed. Again, possible thermal bone damage must be taken into consideration. In rotating implant bed preparation, special care should be taken on the adjacent structures such as roots and nerves so as not to injure and perforate an undercut ridge area or the maxillary sinuses. If problems occur during implant bed preparation, such as a perforation in the ridge area, a change of implant direction is advisable, although it still has to be acceptable from a prosthetic point of view. Alternatively, a shorter implant can be used.

Fig 8-9a Typical radiologic appearance of BBS: periapical radiologic bone demineralization around the implant. Clinical symptoms were also present in the form of an uncomfortable sensation on loading the implant crown after the restoration.

Fig 8-9b CBCT scan confirming the demineralization around the apex of the implant.

Fig 8-9c A bony lid is prepared with the MicroSaw.

Fig 8-9d Exposed implant with the apical granuloma after the removal of the bony lid.
Fig 8-9e Clinical situation after removal of all the granulation tissue from the implant surface and the bone cavity.

Fig 8-9f The implant surface is cleaned with hydrogen peroxide (H2O2) 3% for 2 min.

Fig 8-9g Photodynamic decontamination with the Helbo system.

Fig 8-9h The bony lid is replaced at the end of surgery.

Fig 8-9i Radiologic healing of the periapical lesion 7 months postoperatively.

Fig 8-9j Clinical appearance 7 months postoperatively: all clinical symptoms had already disappeared 2 weeks postoperatively.
Fig 8-10a Extraoral fistula at about 4 months after implant insertion in a very hard bone. A smooth instrument is introduced into the fistula for the radiologic diagnosis. After the surgery, the patient experienced an uncomfortable feeling in the area, with some chronic pain.
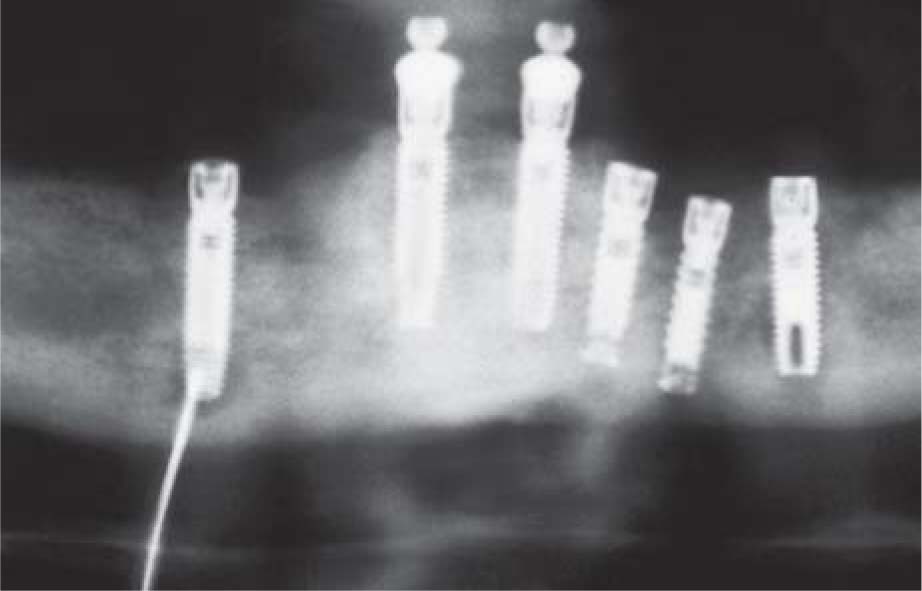
Fig 8-10b Radiologic confirmation of the clinical diagnosis.

Fig 8-10c A bony lid is prepared with the MicroSaw.

Fig 8-10d The connection of the apical part of the implant to the fistula is confirmed after removal of the bony lid and the implant.

Fig 8-10e Repositioning of the bony lid after removal of all the granulation tissue and cleaning of the socket.

Fig 8-10f Complete healing after 3 weeks.
8.3.2 Complications during bone harvesting procedures
Compared with extraoral bone harvesting, intraoral bone harvesting offers very low morbidity and several advantages.107,171,172,181 Intraoral bone harvesting can be performed with a minimally invasive approach, mostly under local anesthesia and without hospitalization. Various donor regions in the maxilla and mandible can be used for intraoral bone harvesting of autogenous bone; important neighboring anatomical structures such as roots, blood vessels, and nerves must be taken into account in each case.75 Block bone grafts, which are suitable for the 2D and 3D reconstruction of alveolar ridge defects,112,115 can be harvested intraorally, usually only in the mandible,102,103,148,150 namely in the retromolar region, the chin or edentulous sections (e.g. under pontics).111,142,148,208 These are mainly cortical and corticocancellous grafts. The potential risks and complications depend on the anatomical variation of the donor site.41,150
8.3.2.1 Complications during bone harvesting from the retromolar region
Before intraoral mandibular bone block harvesting, a palpation of the bony structures is routinely performed before the surgery. This provides information on the morphology of the potential donor site. The extension of the external oblique ridge and the body of the mandible can be determined in this manner. The imaging standard diagnostic procedure begins with a panoramic radiograph from which the position of the mandibular nerve, the mental foramina, and the tooth roots can be determined. A pronounced external oblique ridge can be felt clinically and is seen on the panoramic radiograph as a radiopaque cortical line (lamina dura).
In addition, a CBCT scan can be useful when the alveolar nerve, detected on the panoramic radiograph, is in a crestal position that can be close to the harvesting area, or when the harvesting of a voluminous bone block is planned that reaches the vertical part of the mandible. In this situation, the CBCT scan gives precise information on the position of the nerve and its distance from the surface of the buccal bone.6,119,160,214,216,217
It is recommended to use a local anesthesia with vasoconstriction to reduce intraoperative bleeding and to allow a good view of the surgical site.
Harvesting of a bone block from the retromolar area following the MicroSaw protocol is a fast and safe surgical procedure. Protection devices mounted on the hand- and angle-piece prevent injury to the soft tissue (Fig 8-11). The method described in Chapter 4 significantly reduces the risk of mandibular nerve injury.73,113 The distance of the mandibular canal to the buccal surface of the mandible in the region of the first and second molars is an average of 5.4 mm, and up to 4.6 mm in the area of the wisdom tooth and the retromolar region.68,106 Usually, the nerve in the molar region is much closer to the lingual cortex (Fig 8-12). Mesially, the osteotomy line is normally limited to the mesial border of the external oblique line, which usually ends between the first and second molars. In this area, a nerve injury with the diamond disc of the MicroSaw is extremely unlikely because its maximum penetration depth is 3.2 mm, which cannot reach the mandibular canal. Only more distally, in the area of the ramus, can the mandibular canal be more superficial (Fig 8-13a to d).

Fig 8-11 The tissue protector of the MicroSaw allows for a secure harvesting with a good view and without injuring the soft tissue.
Fig 8-12 The alveolar nerve is mostly in a lingual position in the molar and retromolar area.

Fig 8-13a The MicroSaw can cut to a maximum depth of 3.2 mm.

Fig 8-13b Exposure of the inferior alveolar nerve after harvesting a voluminous bone block from the retromolar area. The posterior part of the nerve is more buccal (a depth of 2.6 mm) than the anterior part (6.8 mm).

Fig 8-13c The thickness of the buccal cortical bone over the mandibular nerve is about 3.4 mm.

Fig 8-13d Exposed alveolar inferior nerve with details regarding nerve position after bone block harvesting from the retromolar area.

Fig 8-13e Harvested bone block with part of the bone wall of the mandibular canal.
Nerve exposures can occur when the external oblique line is weak and the basal osteotomy is carried out below the nerve course (Fig 8-13e). Even then, it is difficult to reach the nerve with the diamond disc, as long as the withdrawal is limited to the retromolar area. If the bone block removal has led to nerve exposure, great care must be taken not to traumatize or compress the exposed nerve with sharp-edged bone particles.
The dangers of nerve injury are significantly higher when the distal vertical osteotomy is performed in the region of the ascending ramus, as the alveolar nerve in this posterior area often runs close to the buccal cortical bone before it moves mesially into a deeper, more lingually oriented position (Fig 8-14a to d). In these cases, it is advisable not to sink the diamond disc to its full cutting depth, both at the distal vertical and distal horizontal basal osteotomies. Instead, the disc should only be sunk to a maximum of 2 mm (the diamond tip is 1-mm wide) or the 6-mm–diameter diamond disc with the maximum cutting depth of 2.1 mm (Fig 8-14e) should be used. Alternatively, a first bone block can be harvested above the nerve course to collect information about the bone structures, and in particular the width of the vestibular cortical bone. If necessary, a second, more apically located bone block can be harvested under direct view. In very rare cases, the lamina dura of the mandibular canal is very dense and is directly sealed to the buccal cortical bone, so that the bone block, even after its dislocation, still seems to be attached to something elastic. In this situation, the bone block should be removed slowly and carefully so that the nerve can be gently released from the bone block (Fig 8-15). Permanent nerve damage after its exposure is not known, but it may lead to a temporary sensory disturbance.99,146 Nerve injury in bone harvesting surgery from the retromolar area can be caused by other instruments, e.g. through the improper use of the chisel.
Therefore, the protocol for bone harvesting with the MicroSaw (see Chapter 4) should be respected, dislocating the bone block by creating tension. In this way, an uncontrolled deep sinking of the chisel and potential nerve damage are avoided. Should the bone block not be dislocated after three to four controlled hammer blows, the osteotomies should be checked first. In particular, it is important to clarify whether the osteotomies completely cross over each other (Fig 8-16a). Especially on the distal side of the prepared osteotomy, there is often an incomplete crossing of the vertical and horizontal section. The cuts should be parallel or tapered.
The MicroSaw bone harvesting protocol from the retromolar area is based on the presence of a cortical bone on the vestibular side of about 3 mm (to be cut with the saw), and a spongy bone area that will present no resistance after the dislocation of the cortical part. In a case where this balance is disturbed through the presence of a very dense and cortical bone without any spongy bone area, the harvesting of the bone blocks following the presented protocol becomes more difficult.
However, dense bony structures such as sclerosis can often be recognized in the preoperative radiograph (Fig 8-16b). In this situation, it is recommended to first harvest a small bone block, making it easier to then harvest a second bigger one (Fig 8-16c). In addition, the crestal drill perforations should be positioned above the remaining cancellous bone and not within the buccal cortical bone. The angulation of the chisel should be aligned parallel to the buccal mandibular wall and the dislocation made just above the point of drilling, whereas to avoid nerve injury, the chisel must not enter deeply into the mandible.
In a study, 3874 bone blocks were harvested according to the MicroSaw protocol from the external oblique line of the mandible in 3328 patients within 10 years.119 During the study time, 419 patients (12.59%) underwent bilateral bone block harvesting, and 127 patients (3.82%) underwent more than one block harvesting from the same area. In 2285 donor sites, osteotomy lines were positioned basally of the level of the alveolar nerve. In 168 (7.35%) of those cases, mandibular alveolar nerve exposition occurred, generally in the distal area of the donor site, leading to transient sensory problems that lasted for a maximum of 6 months. In 20 cases, minor nerve injury occurred (0.5%): 8 patients (0.2%) demonstrated a hypoesthesia and 12 (0.31%) a paranesthesia lasting for up to 1 year. In four patients (0.1%), the paranesthesia was present for more than 1 year. No major nerve lesion of the mandibular nerve with permanent anesthesia was observed in any case. Heavy bleeding at the donor site, which was controlled through compression with collagen fleece and/or bone chips, occurred in 56 harvesting cases (1.44%). Postoperatively, only a little pain was observed in 1624 patients (48.8%), another 1589 patients (47.74%) experienced moderate pain, and only 115 patients (3.45%) had severe pain.
Fig 8-14a Extremely coronal position of the mandibular canal in the retromolar area after orthognathic surgery (mandibular anterior advancement): no presence of an external oblique line.

Fig 8-14b Complete exposure of the superficial nerve after bone block harvesting extended to the ramus area.

Fig 8-14c The harvested bone block demonstrates the extremely superficial position of the nerve.

Fig 8-14d The risk of nerve injury through the distal incision must be considered when harvesting bone blocks from the ramus area.

Fig 8-14e Two diamond discs with an 8-mm (left) and 6-mm (right) diameter can be used for the harvesting procedure. It is useful to use the smaller (6-mm diameter) disc when harvesting bone blocks close to the alveolar nerve.
CBCT is a helpful tool for prediagnostic anatomical evaluation and thus reduces the risk of potential complications.161 In the authors’ experience, this additional diagnostic is not essential for a safe bone harvesting procedure using the MicroSaw; however, it provides further information such as the thickness of the cortical wall and the position of the mandibular nerve.101 It therefore provides helpful presurgical information, especially if the osteotomies are located underneath the level of the mandibular nerve. The thickness of the cortical bone in the area of the distal osteotomy is 1.5 to 3.5 mm (average thickness: 2.2 mm). The cortical bone in the area of the mesial osteotomy is much thicker, with a minimum thickness of 2.5 to 5.5 mm (average: 3.3 mm). The distal osteotomy seems to be more critical and requires special attention concerning the cutting depth.119 In another study of 968 retromolar bone harvesting procedures, one case was observed that concerned a fracture of the lingual bony wall. The fragment was fixed with an osteosynthesis screw, allowing for uneventful healing (Fig 8-17a and b).
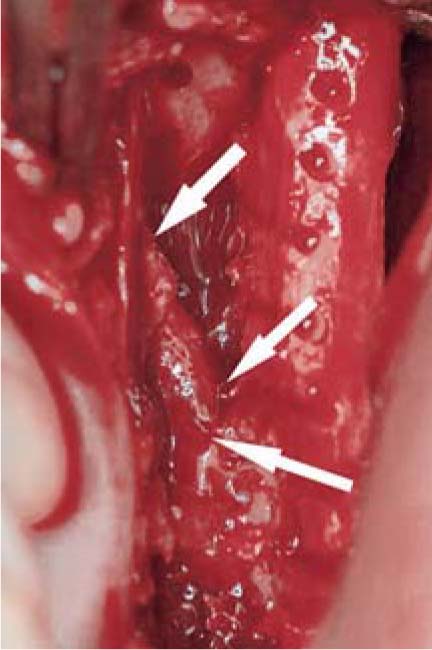
Fig 8-15 In very rare situations, the alveolar inferior nerve can move with the harvested block outside the mandibular body: care should be taken to detect such a situation on time to avoid nerve injury. [Fig 8-15 courtesy of Dr. J. Tunkel.]

Fig 8-16a The horizontal osteotomy should cross over the vertical one.

Fig 8-16b Intensive sclerotic bone in the retromolar area without the typical external oblique line will make it difficult to harvest bone following the described protocol.

Fig 8-16c Removal of a small bone block first will simplify the harvesting of the remaining graft in case of sclerotic bone quality.
Fig 8-17a Accidental harvesting of a bicortical bone block from the retromolar area. Before the complete bone block dislocation, separation of the buccal from the lingual bone, repositioning of the lingual bone, and stabilization with a screw were performed.

Fig 8-17b Good healing 5 months postoperatively.
Fractures of the mandible were described to possibly occur not during the harvesting procedure but about 2 to 3 weeks postoperatively, which is similar to the situation after the removal of an impacted wisdom tooth.107 For this reason, it is very important after bone harvesting from the retromolar area to instruct the patient regarding the essential need for a soft diet for least 6 weeks postoperatively. The greatest risk of mandibular fracture is about 2 to 3 weeks after the surgery, when the patient can resume eating regular food after not having been able to eat solid food at all before this due to pain and swelling (Fig 8-18a to c).
The complication rate for retromolar bone harvesting is very low. Although infections (0.5%)43 or hematoma in the donor site can be observed, nerve injury and an altered sense of perception seldom occur.41,113,150,157 After removal of the bone block graft, cancellous bone is exposed. This increases the probability of postoperative hemorrhage or hematoma. To counteract complications such as bleeding or hematoma and to achieve a stabilization of the blood clot, the donor site is filled with lipophilized allogenic collagen matrix (Resorba, Nürnberg, Germany).
Since the extent of surgical retromolar bone block removal corresponds to the removal of impacted third molars, the postoperative morbidity in both cases is comparable. In a clinical study, patients’ classified postoperative pain in the donor site was significantly lower compared to that in the recipient area.157
In summary, the retromolar region is a suitable area for the harvesting of medium-sized bone block grafts with little expenditure of time, not much stress for the patient, and minimal risk of complications.
8.3.2.2 Complications during bone harvesting from the chin
As part of the preoperative diagnosis made before the harvesting of intraoral bone blocks, the chin is routinely palpated to obtain information about the extension of the bony mental protuberance. The location of the mandibular nerve, the mental foramina, and the roots can be determined on a panoramic radiograph. In addition, a lateral cephalometric radiograph is performed, which is used for the estimation of bone quantity and quality, the thickness of the anterior cortex, and the determination of the localization and angle of inclination of the anterior roots in the existing mandibular anterior teeth.80
Fig 8-18a Free-end situation in the right mandible with bone atrophy.

Fig 8-18b Fracture of the right mandible 3 weeks after bone block harvesting.
In accordance with the protocol described in Chapter 4, the mental nerve is exposed on both sides before the bone block is prepared with the MicroSaw. A monocortical bone block is cut while maintaining a minimum distance of 3 to 5 mm from the root tip, about 8 to 10 mm from the alveolar crest in edentulous patients, and 3 to 5 mm from the basal mandibular border.3,146
Another study based on CBCT recommends a safe zone for implant surgery and bone harvesting surgery of 4 mm anterior to the mental foramina and 10 mm above the inferior margin of the mandible. According to this study, the chin bone should be harvested at least 10 mm below the tooth apices, along with a limited depth of 4 mm.214 However, this recommendation leads to an important limitation of the harvesting procedure and at least to a small bone block graft.
The most important intraoperative risk in bone block harvesting from the chin area is the injury of the rami dentali inferior of the alveolar nerve, with the consequence of a neurosensory disturbance of the mandibular anterior teeth. In one study, this was shown to persist for more than 6 months in 7% of the patients (Fig 8-19a and b).113 Furthermore, although very rare, sensitivity changes of the mucosa, the chin or the outer lip surface have also been described.37,41,98,157,160,216 Another study reported that 19 months after the removal of bone from the chin, 15 of 29 patients still had reduced sensory disturbance in the anterior area.41 For this reason, it is recommended to harvest bone blocks from the chin area, if possible only in the case of an edentulous anterior mandible.

Fig 8-18c Stabilization of the fracture with an osteosynthesis plate.
A possible postoperative complication in the donor site at the chin is wound dehiscence, with or without wound infection, the frequency of which is reported in the literature to be 2.5% to 10%.10,11,41,43,98,113,150,157 This is due to the strong muscle activity in this area in the presence of a thin gingival biotype. Adequate soft tissue coverage is the key factor for nonirritating wound healing. For this reason, a double-layer closure is strongly recommended. With existing mandibular anterior teeth, after infiltration anesthesia, the soft tissue incision is therefore made at an angle below the mucogingival border in order to obtain broad wound edges and allow for a multi-layered wound supply. Resorbable suture material for submucosal sutures is essential.

Fig 8-19a Ramifications of the inferior dental rami are often injured during bone block harvesting from the chin area.

Fig 8-19b Exposure of the inferior alveolar nerve with its ramification after the removal of a bone block from the chin area.
In edentulous patients, and in simultaneous implant placement in the mandibular anterior region, the incision is made on the alveolar ridge. The donor site is exposed after removal of a mucoperiosteal flap. The risk of dehiscence increases when membranes and biomaterials are used to regenerate the defect. Early dehiscence with nonresorbable membranes requires rinsing with chlorhexidine solution or gel, which is applied daily by the patient for 3 to 4 weeks until the membrane is finally removed. In late exposure or infection, an immediate removal of the membrane is performed. Infections can lead to pus and a bad defect regeneration.
Bone harvesting close to the root apex of the mandibular canines can lead to pulp necrosis of these teeth. For this reason, it is strongly recommended to maintain a minimum distance of 5 mm from anatomical structures such as the roots, the mental foramen, and the mandibular border. The mandibular border provides the framework for bone regeneration.113 No changes were observed either in the extraoral profile or to the chin prominence after these recommendations were followed.146
8.3.2.3 The flying bone block
During the splitting of the harvested bone block, especially if it is not stabilized adequately between the two fingers, the block can fly away and land on the ground if the diamond disc is blocked in a bone retention. In this situation, it is important not to throw away the bone. Instead, it should be collected, cleaned with 3% hydrogen peroxide (H2O2), and conserved in an antibiotic solution of 1 g amoxicillin for 10 min. A photodynamic decontamination can be useful before closing the wound after the grafting procedure (Fig 8-20a to f). It is important not to forget the tetanus prophylaxis if a bone block lands on the ground. In the 14 cases of flying bone blocks documented in the authors’ hospital in the last 25 years and treated with the presented protocol, all the grafted bones healed uneventfully and without any complications.
Fig 8-20a Strong atrophy of the alveolar crest in the right maxilla.

Fig 8-20b Insertion of two implants in combination with bone splitting.

Fig 8-20c Bone block grafting to support the broken vestibular bone: The flying bone blocks landed on the ground and were treated with the described protocol.

Fig 8-20d Photodynamic treatment before wound closure.

Fig 8-20e Clinical appearance 2 years postoperatively.

Fig 8-20f Radiographic control 2 years postoperatively demonstrating the good osseointegration of the implants.
8.3.3 Complications during alveolar extension and bone-splitting techniques
Extension techniques such as bone spreading or bone splitting allow for the insertion of implants even in relatively narrow ridges. During such techniques, complications may occur. The most frequently seen complication is a fracture of either the buccal or the lingual plate, with total or subtotal dislocation of the fragment (Fig 8-21a to c). The procedure then changes into a kind of block grafting, because the fragment has to be secured with osteosynthesis screws (Fig 8-22a and b).

Fig 8-21a Fracture of the buccal bone after implant placement in combination with bone splitting.

Fig 8-21b Stabilization of the fractured buccal bone with a bone block graft.

Fig 8-21c Occlusal view of the grafted area.
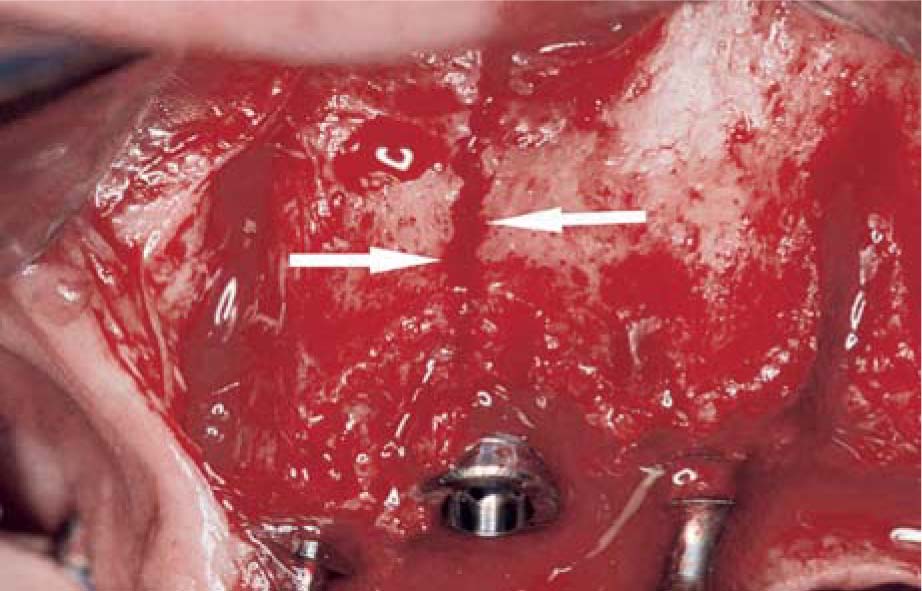
Fig 8-22a Vertical fracture of the maxillary bone through excessive spreading during implant placement.

Fig 8-22b Fracture stabilization with a bone block at the crestal side and with an osteosynthesis plate in the apical part.
Fig 8-23a Fracture of the buccal bone in the first 5 mm of the crestal bone.

Fig 8-23b Implant insertion inside the bony contour.

Fig 8-23c Stabilization of the fractured bone with a nonresorbable membrane.

Fig 8-23d Clinical appearance 3 months postoperatively after membrane removal.

Fig 8-23e Occlusal view after membrane removal.
In cases of smaller fractures, the stabilization of the fragments can also be obtained by means of a membrane (Fig 8-23a to e). There is a better chance of healing in the situation where the periosteum still covers the bone surface. This means that the broken buccal or palatal luxated bone wall is still pedicled by the periosteum. Moreover, in such a situation, the loosened buccal wall can simply be stabilized with a suture on the periosteum, to the lingual side (Fig 8-24a to c). Chisels and osteotomes may damage adjacent tooth roots, nerves or the maxillary sinus.113,150
An excessive use of bone condensing or bone spreading instruments in the maxilla is very uncomfortable for the patient and can lead to headache and disturbance of equilibrium through direct transmission of the forces to the brain (mini commotio cerebri).

Fig 8-24a Bone splitting in the anterior maxilla.

Fig 8-24b After implant insertion, the buccal bone (still attached to the periosteum) is mobile.

Fig 8-24c Stabilization of the mobile bone with a resorbable 6-0 suture, connecting the buccal and palatal periosteum.
8.3.4 Complications during sinus floor elevation
Knowledge of the anatomy and physiology of the sinus area is very important to prevent complications during sinus floor elevation. The maxillary sinus is lined with a membrane, the Schneiderian membrane, which provides a so-called mucoperiosteal, i.e. periosteum covered with respiratory epithelium. The ventilation of the maxillary sinus occurs via the maxillary ostium. Bony septa divide the sinus part into several compartments. The number and intensity of the septa can be very different. They are visualized on panoramic radiographs, CT and CBCT scans (Fig 8-25a). The sinus mucosa, like the maxillary sinus walls, is intensely vascularized and is supplied by branches of the posterior superior alveolar and infraorbital arteries. Important blood vessels in the sinus wall can be preoperatively detected through CBCT (Fig 8-25b and c).
Accordingly, risks must be identified in terms of the intensive preoperative diagnosis so that possible complications that can negatively influence the treatment outcome can be prevented or treated appropriately.97,137,195,196,211
8.3.4.1 Heavy bleeding
The vascular supply of the maxillary sinus and the alveolar ridge, particularly the buccal sinus wall, is supplied by the posterior superior alveolar artery and the infraorbital artery. The two vessels are connected via an intraosseous arterial anastomosis.193 An extraosseous, vestibular vascular anastomosis was found in 44% of cases. Usually, medium-sized blood vessels, mostly arteries, can be found in the area where the bony window has to be prepared for external sinus floor elevation (Fig 8-25d). The exposure and isolation of these arteries, which permits the surgeon to continue without disturbing the sinus floor elevation, is very time consuming and can lead to severe bleeding due to a breach of the vessels. It is recommended, if possible, to change the position of the bony lid and to prepare it under the artery. Otherwise, a careful preparation is required to expose the artery inside the bone for the whole length of the bony lid by using a small round diamond bur (Fig 8-25e). After sufficient exposure of the vessels, it is recommended to strangulate or coagulate the arteries (Fig 8-25f to h), allowing the surgical procedure to continue.
The sinus mucosa is well supplied with blood vessels and is prone to profuse bleeding when injured. Stopping the bleeding from the sinus mucosa by compression is rather difficult, but normally this bleeding will stop slowly by itself after placement of the augmentation material, which softly compresses the bleeding area in the sinus mucosa. On the other hand, the good blood circulation in the Schneiderian membrane ensures the quick healing of the surgical wound.22

Fig 8-25a Multiple septa in both sinuses.

Fig 8-25b CBCT scan demonstrating a blood vessel in the facial sinus bone.

Fig 8-25c CBCT scan demonstrating two thick vessels.

Fig 8-25d Blood vessel in the facial bone of the sinus.
Fig 8-25e Exposure of a thick artery with a diamond bur during the sinus lift procedure.

Fig 8-25f Exposed artery.

Fig 8-25g Coagulation of both borders of the artery with a bipolar device.

Fig 8-25h After the coagulation, the elevation of the sinus mucosa can be performed as planned.
8.3.4.2 Perforations of the sinus mucosa
The incidence of perforation of the sometimes extremely thin and fragile sinus mucosa22 during sinus floor elevation procedures is given as 10% to 35% of cases.15,95,167,172,175,195,207,212 Scar tissue caused by inflammation and large bone defects can increase anatomical difficulties and risks, especially due to the strong adhesion of the thin mucosa to the underlying bony surface. Chronic sinusitis, however, leads to a thickening of the membrane and thus an easier preparation and elevation of the sinus mucosa.95
In the case of a perforation, it is necessary to continue the elevation of the remaining sinus membrane from the bony sinus floor, releasing the tension from the membrane and simultaneously obtaining more tissue and material to close the perforation. Awareness and sensitivity are required in order to avoid an increase of the perforation. Therefore, it is often useful to enlarge the prepared bone window in order to better expose the area of perforation. Regardless of the size of the perforation, its borders have to be adapted mechanically, closing the perforation to prevent the migration of grafting material to the sinus, which can lead to infection and sinusitis. This procedure also reduces the risk of contamination of the graft by the sinus flora. The adaptation of the borders of the perforation is stabilized with a thin resorbable 7-0 suture using a small round needle (e.g. PGA; Resorba) (Fig 8-26a to c). In some situations, and depending on the extension of the perforation, many sutures are performed to hermetically close the perforation (Fig 8-26d to h). In cases where the perforation is very close to the bone, a sufficient suturing together of the borders of the perforation is very difficult. In this situation, it is recommended to prepare a small hole in the adjacent bone wall and to suture one side of the perforated mucosa directly through the hole to the bone (Fig 8-26i to k).
In cases of sinus perforation where there is the presence of a thin sinus mucosa, it is recommended to use fibrin glue in addition to the sutures. Sutures alone on a very thin sinus mucosa are not stable enough and can break under the respiratory overpressure inside the sinus or during the application of the augmentation material. In these situations, fibrin glue will offer more stability to the weak sutures and protect them from uncontrolled tension (Fig 8-27a to f). Fibrin glue is also used to close sinus perforations with very poor accessibility for suturing, as for instance in the distal region of the maxillary sinus. In this situation, the borders of the perforation have to be very close to each other before the gluing is performed (Beriplast; Behring, Marburg, Germany). Fibrin glue has shown very good results for this kind of treatment.39,112 Centrifuged blood, e.g. platelet-rich fibrin (PRF) or plasma rich in growth factors (PRGF), can be used as an alternative to fibrin glue but has to be stabilized correctly; the advantage here is, of course, the use of autogenous material with some growth factors.
The attempt to close a perforated sinus membrane with a resorbable collagen membrane is risky and unphysiologic. On the one hand, the collagen is not stable enough to prevent a dislocation of the augmentation material into the sinus; on the other hand, there is a high risk of contamination of the exposed collagen membrane to the inner part of the sinus mucosa by the sinus flora, which can also lead to an infection of the augmentation material and ultimately to sinusitis and failure of the augmentation. In a study by Choi et al39 concerning the treatment of perforation of the sinus mucosa during sinus lift procedures, the authors found that wounds repaired with autologous fibrin glue showed newly formed continuous epithelium across the previous perforation site. However, extensive fibrosis, inflammatory infiltration, and absent epithelium were observed in wounds treated with the collagen membrane (control).39
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses