Retromandibular Approach
The retromandibular approach exposes the entire ramus from behind the posterior border. It therefore may be useful for procedures involving the area on or near the condylar neck/head, or the ramus itself. In this approach the distance from the skin incision to the area of interest is reduced compared to that of the submandibular approach.
SURGICAL ANATOMY
Facial Nerve
The main trunk of the facial nerve emerges from the skull base at the stylomastoid foramen. It lies medial, deep, and slightly anterior to the middle of the mastoid process at the lower end of the tympanomastoid fissure. After giving off the posterior auricular and branches to the posterior digastric and stylohyoid muscles, it passes obliquely inferiorly and laterally into the substance of the parotid gland. The length of the facial nerve trunk substance abuse that is visible to the surgeon is approximately 1.3 cm. It divides into the temporofacial and cervicofacial divisions at a point vertically below the lowest part of the bony external auditory meatus (see Fig. 10.1). The average distance from the lowest point on the bony external auditory
meatus to the bifurcation of the facial nerve is 2.3 cm (Standard deviation 0.28 cm) (1). Posterior to the parotid gland, the nerve trunk is at least 2 cm deep to the surface of the skin. Its two divisions proceed forward in the substance of the parotid gland and divide into their terminal branches (see Fig. 10.2).
meatus to the bifurcation of the facial nerve is 2.3 cm (Standard deviation 0.28 cm) (1). Posterior to the parotid gland, the nerve trunk is at least 2 cm deep to the surface of the skin. Its two divisions proceed forward in the substance of the parotid gland and divide into their terminal branches (see Fig. 10.2).
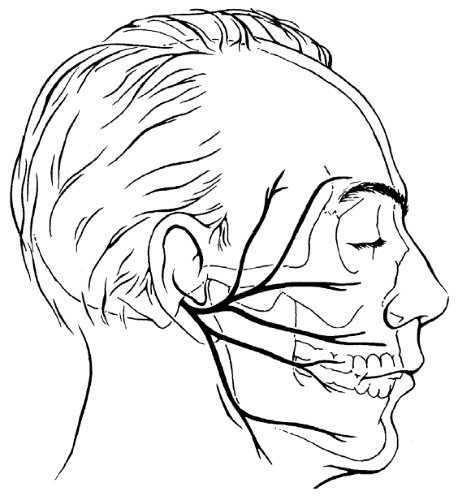
Figure 10.1 Branching of the extracranial portion of the facial nerve. Only the main branches are shown. Many smaller branches occur in most individuals (Fig. 10.2).
|
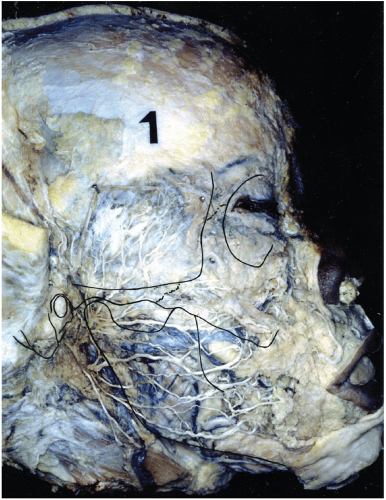
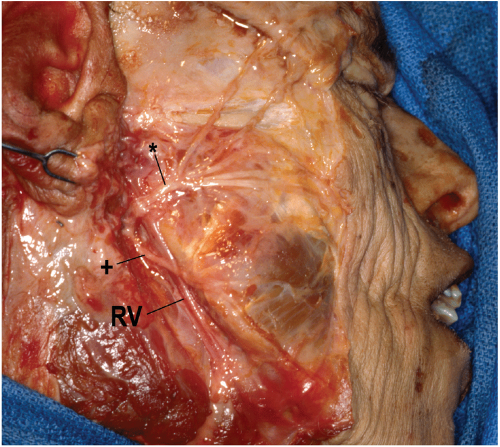
Figure 10.2 Anatomic dissection reveals an extensive branching pattern of the facial nerve (the parotid gland was removed).
|
The marginal mandibular branch courses obliquely and anteriorly downward. It frequently rises from the main trunk well behind the posterior border of the mandible and crosses the posterior border in the lower one third of the ramus. This positioning leaves a void between the buccal branches and the marginal mandibular branch or branches through which the mandible can be approached safely (see Fig. 10.3).
Retromandibular Vein
The retromandibular vein (posterior facial vein) is formed in the upper portion of the parotid gland, deep to the neck of the mandible, by the confluence of the superficial temporal vein and the maxillary vein. Descending just posterior to the ramus of the mandible through the parotid gland, or folded into its deep aspect, the vein is lateral to the external carotid artery (Fig. 10.3). Both vessels are crossed by the facial nerve. Near the apex of the parotid gland, the retromandibular vein gives off an anteriorly descending communication that joins the facial vein just below the angle of the mandible. The retromandibular vein then inclines backward and unites with the posterior auricular vein to form the external jugular vein.
TECHNIQUE
The position of the skin incision, which also dictates the position of the underlying dissection, varies in the retromandibular approach to the mandible. Some surgeons advocate placing of an incision approximately 2 cm posterior to the ramus. The parotid gland is approached from behind and sharply dissected from the sternocleidomastoid muscle, allowing retraction of the gland superiorly and anteriorly to gain access to the ramus. The theoretic advantage of this approach is that it avoids the branching facial nerve, which is contained within the parotid gland. Unfortunately, the primary advantage of the retromandibular approach, which is the direct proximity of the skin incision to the mandible, is then lost. An alternate approach that was described by Hinds (2) is described in this chapter. The incision is placed along the posterior border of the mandible, just below the earlobe. Dissection to the posterior border of the mandible is direct, traversing the parotid gland, and exposing some branches of the facial nerve.
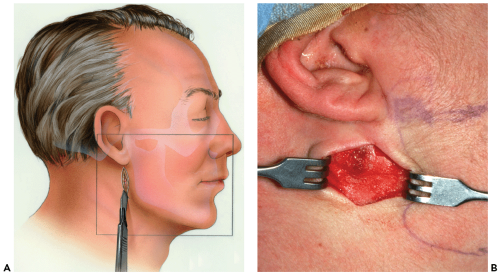
▶ Step 1. Preparation and Draping
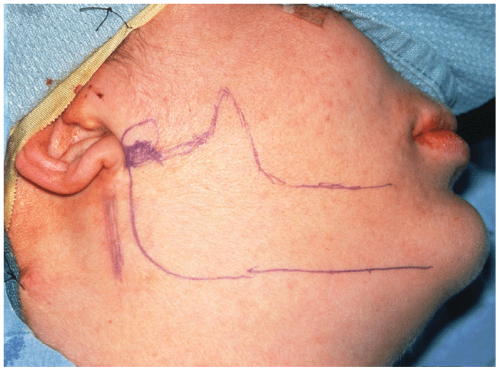
Pertinent landmarks of the face such as the corner of the mouth, lower lip, and the entire ear should be left uncovered during the procedure (see Fig. 10.4). These landmarks orient the surgeon to the course of the facial nerve and allow observation of lip motor function.
▶ Step 2. Marking the Incision and Vasoconstriction
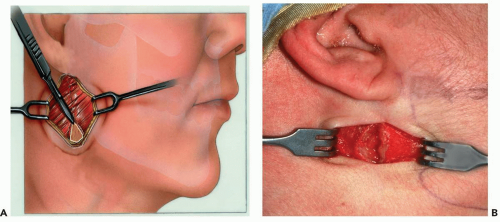
The skin is marked prior to the injection of a vasoconstrictor. The incision for the retromandibular approach begins 0.5 cm below the earlobe and continues inferiorly for
3 to 3.5 cm (see Figs. 10.4 and 10.5). It is placed just behind the posterior border of the mandible and may or may not extend below the level of the mandibular angle, depending on the extent of exposure desired.
3 to 3.5 cm (see Figs. 10.4 and 10.5). It is placed just behind the posterior border of the mandible and may or may not extend below the level of the mandibular angle, depending on the extent of exposure desired.
Epinephrine (1:200,000) without a local anesthetic may be injected deeply, although routine local anesthetics with a vasoconstrictor should be injected only subcutaneously to aid in hemostasis at the time of incision. Even though the facial nerve is located deeper than 2 cm at the earlobe, injection of local anesthetics deep to the platysma muscle risks rendering the facial nerve branches nonconductive, making electrical testing impossible.
▶ Step 3. Skin Incision
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses