The purpose of this article was to describe the closure of a maxillary median diastema of a 26-year-old woman that had been corrected before during orthodontic treatment but reopened after dental trauma in a car accident. A clear esthetic device made from a tray like those used for home bleaching was used, providing a comfortable, nearly undetectable, and efficient solution. A permanent fixed retainer was bonded again to the maxillary central incisors to prevent relapse.
Relapse is an unwanted outcome after orthodontic treatment and retention, especially when it is related to the reopening of spaces in the anterior portion of the mouth. According to Bernabé and Flores-Mir, anterosuperior spacing, more than incisal irregularity, was the occlusal characteristic with the most negative influence on self-perceived dental appearances in a study in young adults in Peru.
A maxillary median diastema is a common esthetic problem in the permanent dentition. Sashua and Årtun concluded that about 10% of orthodontic patients have a maxillary median diastema larger than 0.5 mm after the eruption of the permanent canines. The etiology of a maxillary median diastema is multifactorial, controversial, and not completely elucidated. The relapse of the maxillary median diastema after orthodontic space closure, however, might be as great as 50%. Sullivan et al found no predictors for relapse. Sashua and Årtun observed that the initial width of the diastema, a family member with diastema, and additional spaces between the maxillary anterior teeth are the most predictive factors of relapse.
Permanent retention has been suggested to minimize relapse, since information on the stability after maxillary midline diastema closure is limited. Stability can then be maintained with a fixed permanent retainer.
Case report and treatment
The patient was examined at the age of 26 years. She had received orthodontic treatment in her teenage years. She reported that, in her original malocclusion, there was a persistent maxillary median diastema. She also reported a frenectomy during the orthodontic treatment. The patient had recently been in a car accident and had noninvasive dental trauma with a minor intrusion of the maxillary right central incisor. During this trauma, the permanent retainer bonded to her maxillary central incisors was debonded.
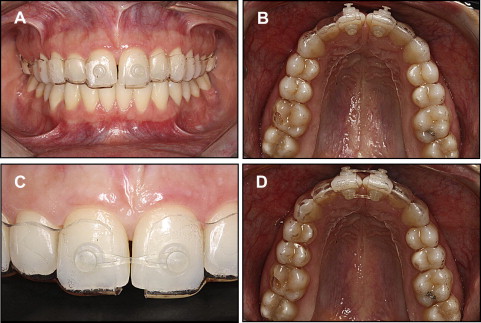
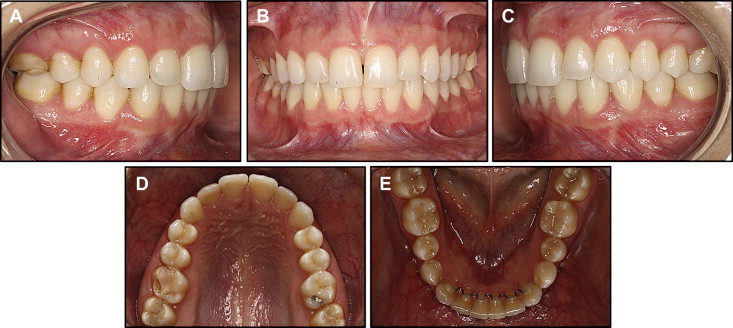
At the clinical examination, a good Class I interarch relationship was observed, and there was a permanent fixed retainer bonded to the mandibular anterior teeth. The restoration of the maxillary right first molar was fractured ( Fig 1 ). A 0.5-mm diastema was noticed between the maxillary central incisors, and this bothered the patient greatly ( Fig 2 ).

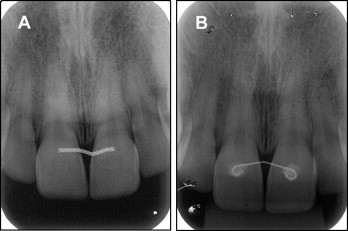
The periapical radiograph showed no signs of lesions in the apical area of the traumatized tooth. It was agreed not to close the diastema before a 6-month follow-up. After 6 months, the maxillary right central incisor showed vital signs, and the aspect on the periapical radiograph was similar to the first one, with no signs of lesions or resorption ( Fig 3 ). The tooth was not discolored.
Therefore, it was decided to close the diastema. The patient did not want retreatment with fixed appliances. Because the diastema was small, for esthetic reasons, a clear device was made to close the space between the maxillary central incisors. A 0.040-in polyethylene terephthalate copolyester thermoplastic sheet was used to make a tray over the dental cast of the patient’s teeth on a vacuum-forming unit. This process is similar to making a tray for home bleaching, described by Newman and Bottone. The tray was trimmed in the vestibular surface of the teeth, avoiding the gingival margin, and extended to the palatal soft tissues for retention. The tray was then cut in half in the midline, and a 2-mm extension from the mesial portion of the maxillary central incisor of each side was cut from each half of the tray so as not to interfere with the closure of the diastema. Two polycarbonate glass-fiber bondable buttons were attached to the region corresponding to the center of the vestibular and lingual surfaces of the maxillary central incisor in each half of the tray with ethyl cyanoacrylate. Special care was taken to prevent the mandibular incisors from touching the buttons bonded in the lingual area in normal occlusion. Two segments of clear medium elastic chain were then applied to the buttons in the vestibular and lingual surfaces ( Figs 4 and 5 ).