Armamentarium
|
History of the Procedure
The reconstructive utility of the rectus abdominis flap was first described in cardiothoracic surgery literature as a modality to reconstruct chest wall defects following sternotomy complications. A regional rotational epigastric island skin flap based on the deep inferior epigastric vessels was used to reconstruct chest wall defects. Taylor and Boyd elegantly clarified the cutaneous perfusion of the abdominal skin based on the deep inferior epigastric artery and vein through ink injection studies. Pennington and Pelly subsequently reported some of the first clinical applications of the free rectus abdominis musculocutaneous flap. The rectus abdominis free flap (RAFF) has been used to reconstruct a multitude of surgical defects crossing multiple anatomic regions and surgical disciplines. The reliable anatomy, ease of harvest, and availability for a two-team approach have made it a first-tier choice for complex reconstructions including sternal wounds, lower extremity defects (especially those in the distal one third of the leg), perineal defects, and breast reconstruction following mastectomy.
History of the Procedure
The reconstructive utility of the rectus abdominis flap was first described in cardiothoracic surgery literature as a modality to reconstruct chest wall defects following sternotomy complications. A regional rotational epigastric island skin flap based on the deep inferior epigastric vessels was used to reconstruct chest wall defects. Taylor and Boyd elegantly clarified the cutaneous perfusion of the abdominal skin based on the deep inferior epigastric artery and vein through ink injection studies. Pennington and Pelly subsequently reported some of the first clinical applications of the free rectus abdominis musculocutaneous flap. The rectus abdominis free flap (RAFF) has been used to reconstruct a multitude of surgical defects crossing multiple anatomic regions and surgical disciplines. The reliable anatomy, ease of harvest, and availability for a two-team approach have made it a first-tier choice for complex reconstructions including sternal wounds, lower extremity defects (especially those in the distal one third of the leg), perineal defects, and breast reconstruction following mastectomy.
Indications for the Use of the Procedure
Although advances in radiotherapy and chemoradiotherapy have vastly altered the practice of head and neck oncology since the late 1980s, surgery remains a mainstay in advanced-stage disease as a component of multimodality therapy. Evidence from the Veterans Affairs (VA) larynx trial is often credited for initiating a paradigm shift that focused on organ preservation and quality of life. Thereafter, many patients with index tumors in areas other than the larynx were subjected to radiation therapy with curative intent rather than surgery. A primary tenet of oncologic surgery is complete surgical extirpation of a tumor including a margin of histologically uninvolved tissue to achieve negative surgical margins. Surgical margins are influenced by the underlying clinical behavior of the tumor as well as proximity to vital structures; however, the intent of surgery remains improved local-regional control translating into improved disease-specific survival. Among all head and neck subsites, squamous cell carcinoma to the oral cavity continues to be managed primarily with surgery based on superior response rates evidenced by improved locoregional control. Moreover, surgical salvage is commonly employed in the setting of local-regional failure among many cancer subsites within the head and neck. The advent of reliable reconstructive options in head and neck surgery gave birth to a new category of surgical defects, creating an ongoing process of discovery.
The introduction of vascularized free flaps revolutionized the extirpative approach to surgical therapy for head and neck cancer and expanded the envelope of surgical feasibility for advanced disease that would not have been otherwise treated with surgery. Reliable regional flaps and free tissue transfer to a greater degree have also improved or maintained form, function, and quality of life for head and neck oncology patients. Nakatsuka and colleagues reported some of the initial favorable results of head and neck reconstruction utilizing the RAFF. Following widespread acceptance in the surgical community, the RAFF continues to serve as a workhorse flap in head and neck reconstruction because of its consistent anatomic landmarks, long vascular pedicle, ease of harvest, and reproducible results. The RAFF filled a void left by the available reconstructive options prior to its development, in particular the broadly celebrated pectoralis major myocutaneous flap. Some of the head and neck indications of this flap include the following advantages.
Advantages
- 1.
Reliable soft tissue donor.
- 2.
Long pedicle that allows connecting to the contralateral side of the defect.
- 3.
Favorable vessel diameter for microvascular anastomosis.
- 4.
The flap can be harvested with multiple skin islands, which allows reconstruction of large through-and-through defects. This can be a great advantage compared to the use of two flaps (free flap and a regional flap or two free flaps); the latter option has a significantly increased operating time, increased donor site morbidity, and increased risk of flap loss as well as the increased need for anatomizing vessels in the neck, which might be decreased by irradiation or previous neck dissection.
- 5.
Easily located landmarks.
- 6.
Possibility of motor nerve harvest by including the segmental nerve.
- 7.
Allows two simultaneously working surgical teams.
- 8.
Primary closure of the donor site, avoiding the morbidity of a second donor site.
- 9.
Minimum volume changes to the rectus abdominis free flap after radiation therapy.
- 10.
Can be used as a single flap to reconstruct radical composite through-and-through defects.
Total and Subtotal Glossectomy Defects
The goal of total and subtotal glossectomy reconstruction is to provide ample, durable tissue bulk to provide glossopalatal contact, which is a key component for bolus transport in the swallowing sequence. Dynamic glossopalatal closure preserves swallowing, creates a narrow oropharyngeal space, and relies on the creation of height and roundness in the neotongue. The rectus abdominis free flap is ideally suited for tongue reconstruction in part because of the inherent bulk imparted by variable degrees of muscle and adipose tissue. Design modifications, including surgical overbulking, functionally improve speech and swallowing and prevent aspiration. Larger defects commonly include portions of the tongue and floor of mouth. The RAFF has the advantage of structurally creating a new mylohyoid muscle through suspension of the anterior rectus sheath to the anterior and posterior mandible to form a hammock-like configuration. From a reconstruction perspective, this maneuver maintains flap bulk while counteracting flap ptosis and thereby preserving necessary glossopalatal contact.
Maxillary and Midface Reconstruction
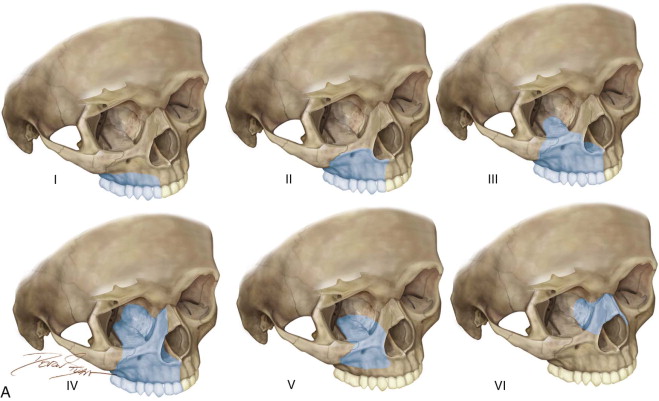
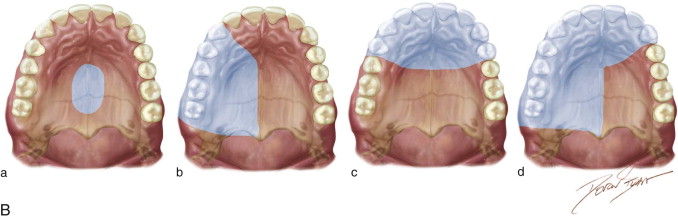
The incidence of maxillary and midface malignancies is comparatively lower than that in other head and neck subsites; however, the functional and cosmetic implications often require free tissue transfer as a component of the surgical treatment plan. Several classifications have been described, commonly sharing the goal of providing a reconstructive scaffold to guide clinical decision making. The Brown classification is a defect-based algorithm that includes vertical and horizontal dimensions and opines broad recommendations according to defect characteristics. A subsequent expanded classification by the same authors included orbital and nasomaxillary defects ( Figure 117-1 ). An ideal maxillary reconstruction should aim not only to isolate the mouth from the sinus and nasal cavity but also to provide bone for potential dental rehabilitation with endosseous implants. The RAFF has been used extensively for maxillary defects, predominantly for class III defects involving the orbital contents.
The advantages of primary midface and maxillary reconstruction include immediate functional restoration and isolation of the nasal cavity and maxillary sinus from the oral cavity, preventing hypernasal speech and alimentary regurgitation. Immediate reconstruction decreases the time frame to begin radiation therapy. Yetzer and Fernandes demonstrated improved quality of life in patients who underwent soft tissue maxillary reconstruction compared with patients who elected obturators as their reconstructive modality. Composite reconstruction of radical midface defects has included the use of nonvascularized bone graft and titanium mesh to reconstruct the osseous orbital walls in conjunction with the rectus abdominis free flap. Yamamato and colleagues described the use of the RAFF with vascularized costal cartilage to reconstruct the orbital floor. The use of the RAFF has been advocated for reconstructing through-and-through defects of the cheek. The available bulk, design versatility, and pedicle length make the RAFF a viable choice for midface and maxillary reconstruction when bone is not required.
Mandibular Reconstruction
The gold standard for composite segmental mandibular reconstruction is free tissue transfer such as the fibula free flap, deep circumflex iliac artery free flap, and scapula free flap. Altered vascular anatomy, venous insufficiency, and functionally significant atherosclerosis of the peroneal vascular system, for instance, may preclude the use of the fibula free flap. Pure soft tissue reconstruction of lateral defects is also used when patients have significant medical comorbidities, lack available donor sites, or are unwilling to undergo composite free tissue transfer. Soft tissue reconstruction of lateral mandibular segmental defects can be used in selected cases, and the RAFF has been used to reconstruct such defects with and without mandibular hardware. The RAFF can be easily modified to accommodate through-and-through defects, particularly of the cheek through the creation of multiple skin islands or partial segmental de-epithelialization. In an effort to decrease plate exposure in soft tissue lateral defects, Yokoo and colleagues espoused a wrapping technique in which the hardware is circumferentially wrapped with muscle, and a portion is de-epithelialized to facilitate closure. The anterior rectus sheath fascia is placed in proximity to the hardware, and the cutaneous element is used for intraoral closure. Wound complications including plate exposure and extrusion are less frequent with this approach.
Dynamic Facial Reanimation
Adynamic reconstruction for patients with Bell’s palsy and facial paralyses provides good resting symmetry and shorter operating time; however, the use of free-tissue transfer has allowed dynamic facial reanimation, which adds the emotional component to the reconstruction. The innervated RAFF has been utilized in dynamic facial reanimation by harvesting the segmental nerve.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


