Armamentarium
|
History of the Procedure
The radial forearm flap was first reported by Yang et al. in 1981 for resurfacing the neck secondary to burn contractures. Use of the flap became popular shortly after Soutar and McGregor in 1986 published a report on a series of 60 consecutive cases in which the radial forearm flap was used for intraoral reconstruction. Since then, numerous articles and book chapters have been written describing both the technique and applications for use of the radial or ulnar artery–based forearm flap for reconstruction in the oral and maxillofacial regions.
This chapter focuses on the radial forearm flap technique and discusses the ulnar forearm flap as an alternate technique for forearm flap reconstruction.
History of the Procedure
The radial forearm flap was first reported by Yang et al. in 1981 for resurfacing the neck secondary to burn contractures. Use of the flap became popular shortly after Soutar and McGregor in 1986 published a report on a series of 60 consecutive cases in which the radial forearm flap was used for intraoral reconstruction. Since then, numerous articles and book chapters have been written describing both the technique and applications for use of the radial or ulnar artery–based forearm flap for reconstruction in the oral and maxillofacial regions.
This chapter focuses on the radial forearm flap technique and discusses the ulnar forearm flap as an alternate technique for forearm flap reconstruction.
Indications for the Use of the Procedure
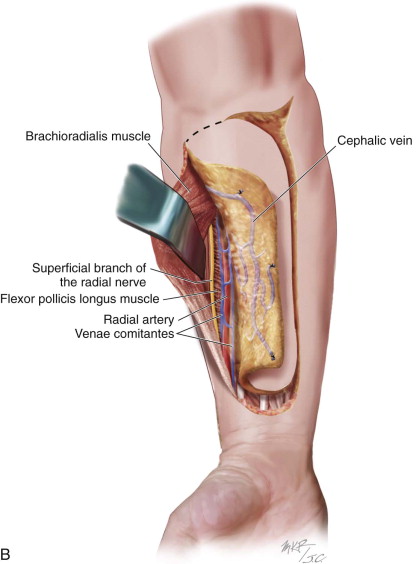
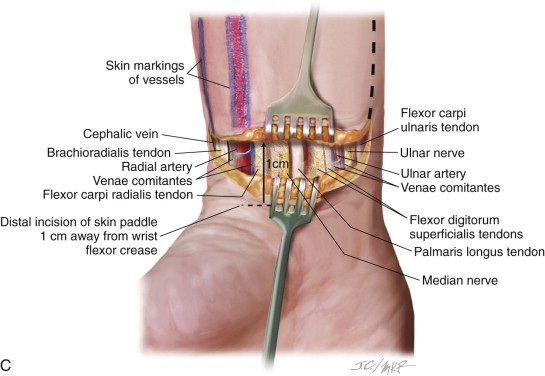
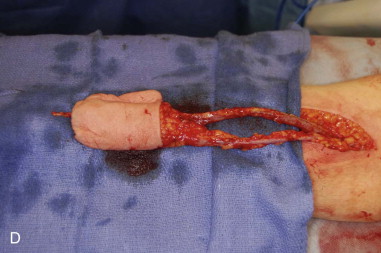
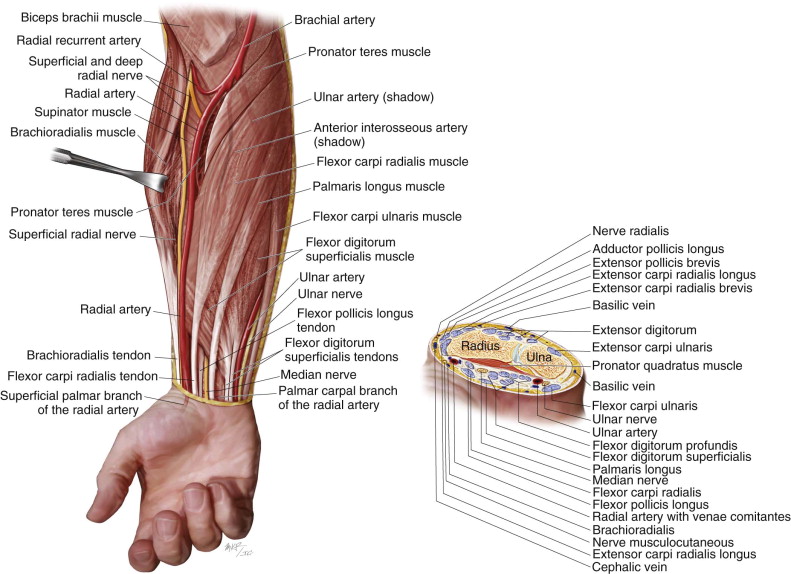
The radial forearm flap is a reliable, versatile flap, based on the radial artery, that can be applied to reconstruction of many anatomic structures in the head and neck. Passing under the bicipital aponeurosis, the brachial artery divides into the radial and ulnar arteries. The radial artery courses deep to the brachioradialis muscle and the pronator teres in the upper third of the forearm and between the tendons of the brachioradialis and flexor carpi radialis in the lower two thirds of the forearm. From this point it travels into the hand, passing through the anatomic “snuff box” and contributing to the dual blood supply of the hand. The skin paddle of the radial forearm flap is supplied by approximately seven to 10 fasciocutaneous branches (average diameter, 0.5 mm) that originate directly from the radial artery ( Figure 114-1 ).Venous drainage is via two independent systems (the superficial [cephalic] vein or the deep venae comitantes traveling with the radial artery), either of which can adequately drain the flap. The pedicle length averages 10 to 12 cm, with good vessel diameter (2.5 mm). Sensory innervation is derived from the lateral antebrachial cutaneous nerves traveling with the cephalic vein or, in the case of an ulnar forearm flap, the median antebrachial cutaneous nerves coursing with the basilic vein. These sensory nerves can be harvested with the flap to provide sensory reinnervation to structures such as the tongue. Most commonly the lingual nerve or inferior alveolar nerve is the selected recipient nerve. Since Urken and colleagues produced the initial reports on sensory radial forearm flap reconstruction for oral and oropharyngeal defects, numerous retrospective cohort series have been detailed. Most series compare the contralateral hemitongue as a control. The results have shown significant differences in neurosensory recovery, with statistical improvements in light touch, temperature sensation, and two-point discrimination. This has also been confirmed on histologic evaluation, with larger, better-arranged, and more numerous nerve fibers identified.
Controversy does exist as to the validity of sensory forearm flap reinnervation with regard to true functional outcomes (speech and swallowing) compared with nonsensate flaps. Many studies are marked by a lack of randomization; poor description of the method of speech and swallow evaluation; and poor reporting of the location and size of the defect and of confounding variables (e.g., adjuvant radiotherapy). Bigliolo et al. reported improved oral function and quality of life with innervated flaps, but Mah et al. found no significant difference between innervated and noninnervated free flaps in terms of speech, swallowing function, or quality of life. Sabesan et al. even demonstrated some level of neurosensory recovery in their series of 40 noninnervated radial forearm flaps.
The superficial branch of the radial nerve supplies sensation to the dorsal aspect of the thumb and index finger. It is located in close proximity to the radial artery and its vena comitans and should be preserved during flap harvest. The flap can be harvested as a fasciocutaneous flap or, if required, bone or tendon also can be transferred. Although many elaborate shapes and designs have been devised, the author routinely uses a rectangular shape and has not found any issue with matching a specific defect. Any redundant tissue can be de-epithelialized or removed during flap inset. The radial artery supplies blood to the bone via fascioperiosteal branches through the intermuscular septum and musculoperiosteal branches through the flexor pollicis longus and pronator quadratus muscles. Up to 10 cm of length and 40% of the cross section of the radius may be safely harvested.
The ulnar forearm flap has similar properties to the radial forearm flap in terms of tissue pliability and thickness. The ulnar artery courses deep to the antebrachial flexor muscles of the upper forearm. In the middle and distal third of the forearm, it travels deep to the muscle and tendons of the flexor carpi ulnaris and flexor digitorum superficialis along an imaginary line from the medial epicondyle of the humerus to the lateral edge of the pisiform bone. The ulnar artery gives off perforating branches to the skin, mostly located in the distal third of the vessel just before traveling into the wrist superficial to the flexor retinaculum. The ulnar nerve is a mixed sensorimotor nerve that travels medially and in close proximity to the ulnar vessels. Preservation of the ulnar nerve is essential for proper function of the hand.
The ulnar artery pedicle generally is shorter than the radial artery pedicle; however, donor site morbidity for the ulnar flap is considered comparable or even superior to the radial flap. Some authors have reported decreased donor site morbidity in terms of neurosensory effects, function, and skin graft loss rates compared to the radial forearm donor site. Other suggested advantages of the ulnar flap, compared to the radial forearm flap, include a skin paddle with less hair and a more esthetic, hidden donor site scar ( Figure 114-2 ).
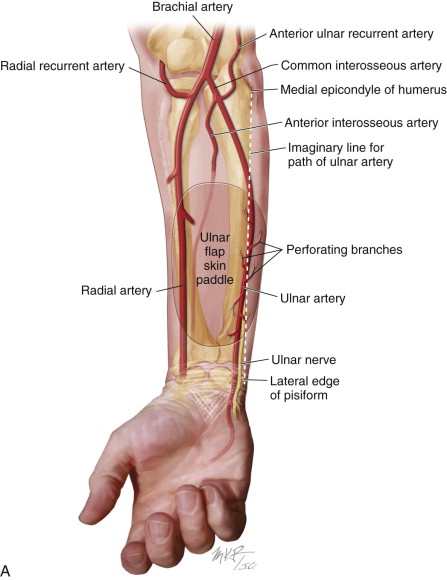

Huang et al. reported on both the anatomy and donor site morbidity in a series of 50 successful ulnar flaps used for reconstruction in the head and neck. The mean diameters of the ulnar artery and vein were 2.3 mm (± 0.6) and 1.7 mm (± 0.6), respectively. The mean number of sizable perforators was 4.3 (± 1.2), and most of the first perforators were located within 5 cm of the proximal wrist crease. There were no long-term complications reported concerning the ulnar nerve.
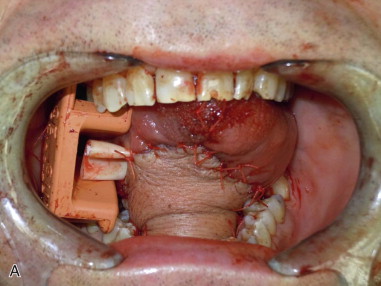
The forearm flap is ideally suited to reconstruct defects of the oral cavity (floor of the mouth, tongue, buccal mucosa, and posterior maxillectomy defects) and oropharynx and also laryngopharyngectomy defects ( Figure 114-3 ). *

* References .
Limitations and Contraindications
Limitations on the use of the forearm flap are based on two main considerations: adequate blood supply to the donor site hand and the type of defect in the head and neck to be reconstructed. The blood supply to the hand is based on the deep and superficial palmar arches. In general terms, the two palmar arches of the hand communicate with each other and form a complete dual loop that communicates with each other to create a dual redundant blood supply to the digits. Blood flow to the deep palmar arch is predominantly supplied by the radial artery, and the superficial arch is predominantly supplied by the ulnar artery. Allen’s test should be performed before surgery to verify an adequate dual blood supply to the hand. In a series of 650 anatomic forearm dissections by Coleman and Anson, 10% of the cases had no branches of the superficial palmar arch to the thumb and index finger and in 50% of the cases, the deep arch did not connect to the ulnar artery. Approximately 5% of the time, both variations are present; in such cases, the blood supply to the thumb and index finger is derived entirely from the radial artery. If there is any question about the integrity of the palmar arches, whether from anatomic variation, previous trauma, or atherosclerotic disease, color flow Doppler ultrasound can be used to assess the adequacy of the palmar arch blood flow. If the forearm donor site is determined to be the best tissue choice for reconstruction and the radial artery is the dominant supply to the hand, the author uses the ulnar forearm flap in the reconstruction of the head and neck defect.
Defects of the head and neck that require large amounts of bulky soft tissue (e.g., subtotal glossectomy, maxillectomy with orbital exenteration, and large skull base defects) are often better suited to reconstruction using donor sites such as the thigh, latissimus dorsi, or rectus abdominis. These donor sites provide more adequate tissue bulk, and their use often avoids the need for donor site skin grafts (as are required with the forearm flap).
The amount of bone available for harvest in the radial forearm osteofasciocutaneous flap is quite limited for reconstruction of the maxillofacial region. Although the use of this flap has been described for short mandibular, maxillary, and orbital rim defects, better donor sites are available, such as the fibula, vascularized iliac crest, and scapula. The latter donor sites provide better bone quality and quantity, allowing for reconstruction of larger bony defects and possibly dental implant rehabilitation as well. Preplating of the osteofasciocutaneous radial forearm donor site has dramatically reduced donor site morbidity; complaints of donor site stiffness and mild wrist weakness are common but do not limit daily activities.
Technique: Radial Forearm Flap Harvest
Step 1:
Allen’s Test to Confirm Adequate Redundant Blood Supply to the Hand
The nondominant hand usually is selected. The radial artery and the ulnar artery are palpated at the wrist. The patient is asked to make a fist, and the arteries are occluded with the surgeon’s fingers. The palm of the hand will appear white. The finger pressure over the ulnar pulse is released, and the hand and digits (including the thumb and index finger) should reperfuse to a healthy color within 15 seconds.
Step 2:
Flap Design and Tourniquet Insufflation
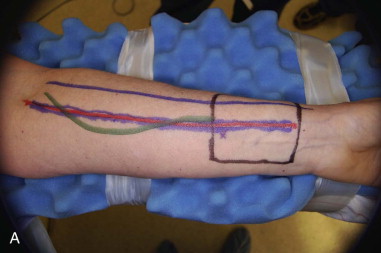
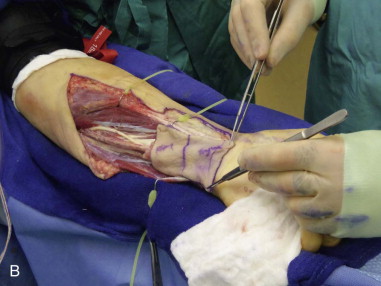
The skin paddle is designed based on the radial artery. The distal end of the skin paddle should be at least 1 cm from the flexor crease of the wrist. Superficial veins (e.g., the cephalic vein) also can be easily identified and marked out on the skin. The forearm is exsanguinated with an Esmarch bandage, and a sterile tourniquet is applied and insufflated to 250 mmHg ( Figure 114-4, A ).
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses