Armamentarium
| Essential to Fracture Repair |
|
| Osteosynthesis |
|
History of the Procedure
Rigid internal fixation of the mandible, although technically described now for almost a century, has only recently been popularized. Traditional treatment of mandibular trauma has centered around the use of closed reduction and immobilization of the jaws. This allowed for secondary bone healing with callus formation, but it did not allow for convalescent jaw function and was susceptible to difficulty in achieving union and infection because of constant micromovement of the fracture site.
The first published descriptions of the use of internal fixation were by Lambotte, Warnekros, and Wassmund during the intervening years of the great world wars. However, it was not until the late 1960s and early 1970s when Luhr, Schilli, and Becker advocated plate and screw fixation for mandibular trauma using bicortical screws at the inferior border of the mandible. In the late 1970s further development of the concept of mini-plate fixation with monocortical screws was developed by Champy.
Since these early reports, substantial research and refinement of the techniques and materials used today for contemporary internal fixation of the mandible has occurred. This has allowed for the routine and safe use of the techniques for the betterment of patient recovery and function during healing.
History of the Procedure
Rigid internal fixation of the mandible, although technically described now for almost a century, has only recently been popularized. Traditional treatment of mandibular trauma has centered around the use of closed reduction and immobilization of the jaws. This allowed for secondary bone healing with callus formation, but it did not allow for convalescent jaw function and was susceptible to difficulty in achieving union and infection because of constant micromovement of the fracture site.
The first published descriptions of the use of internal fixation were by Lambotte, Warnekros, and Wassmund during the intervening years of the great world wars. However, it was not until the late 1960s and early 1970s when Luhr, Schilli, and Becker advocated plate and screw fixation for mandibular trauma using bicortical screws at the inferior border of the mandible. In the late 1970s further development of the concept of mini-plate fixation with monocortical screws was developed by Champy.
Since these early reports, substantial research and refinement of the techniques and materials used today for contemporary internal fixation of the mandible has occurred. This has allowed for the routine and safe use of the techniques for the betterment of patient recovery and function during healing.
Instrumentation
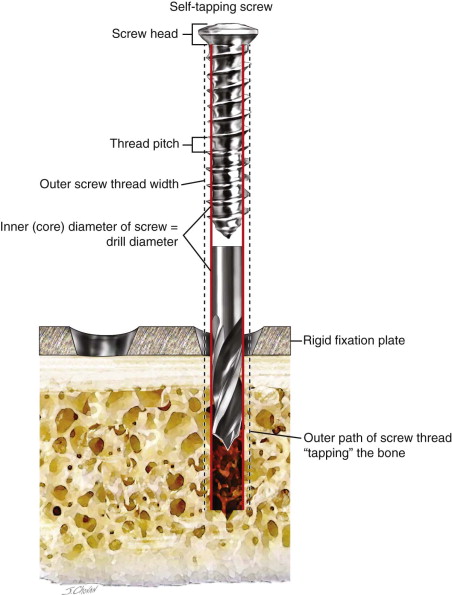
Rigid fixation screws serve to secure plates to fractured bone or compress bone fragments together. Screw holes are usually predrilled, and the size of the drill is equal to the inner diameter of the screw. The outer diameter of the screw is usually the basis for the sizing system of many fixation systems; for example, “2.0 system” might use a 1.8-mm-diameter drill and a screw with an inner diameter of 1.8 mm and an outer diameter of 2.0 mm ( Figure 62-1 ). The outer diameter of the screw is the thread width, which advances the screw and engages bone. The threading of bone by the screw is called “tapping,” and it accounts for the feeling of torque resistance during initial screw placement. Some older fixation systems with non–self-tapping screws required an additional instrument to “tap” the drill hole, but contemporary sets are mostly metallic screws and are self-tapping. Threads engage the bone, transferring forces across the plate and bone, resisting dislodgement or “pull out” forces. Screws from different systems have different head shapes screw driver interfaces (i.e., hex, slot, cross) and pitch (the distance between the threads). Screws may require pretapping (biodegradable screws) or may be self-tapping (as described above) or self-drilling.
The function of a plate is to stabilize adjacent bone fragments long enough to allow healing or “union.” Various designs include adaption (round plate holes), compression (dynamic sloped, oval holes), locking (threaded holes), and reconstruction (wider, higher profile, stronger) plates. In addition, any to a combination of these designs may be seen. Compression plates have sloped holes designed to cause fragment movement (compression) when an eccentrically drilled screw head is tightened against the plate. Reconstruction plates are optimal for atrophic, comminuted, or mandibular fractures with defects in which little or no bone fragment buttressing exists. Mandibular reconstruction plates are generally straight or longer curved plates designed to follow the contours of the mandibular inferior and posterior border. Each system includes smaller and larger profile sizes (plate depth and width), along with various configurations to adapt to specific areas such as the condylr and angle region.
Biomechanical Principles of Rigid Fixation
Definition
Internal fixation is a process of bone fragment stabilization achieved by internal (directly on bone) placement of implants, such as plates and screws. Rigid fixation is one type of internal fixation, and has multiple definitions, including “a form of fixation applied directly to bones which is strong enough to prevent interfragmentary motion across the fracture when actively using the skeletal structure.” Another definition is, “any form of bone fixation in which otherwise deforming biomechanical forces are either countered or used as an advantage to stabilize the fracture fragments and to permit loading of the bone so far as to permit active motion.” Forms of fixation designated as rigid are generally stiff and resilient enough to prevent interfragmentary mobility during healing. Nonrigid fixation “stabilizes the fragments during function but may allow some interfragmentary motion.” Most forms of nonrigid fixation are functionally stable; that is, they do not prevent all interfragmentary motion, but rather create a plate-bone construct that is stable enough to allow some function during skeletal healing. For nonrigid fixation to succeed, the fracture itself must be carefully selected; it should be simple and have good interfragmentary fit and buttressing. The superior border miniplate technique of treating a mandibular angle fracture is a classic example of functionally stable fixation.
Materials
Although resorbable materials such as poly (L-lactide)/polylactic acid implants are available, titanium and its alloys remain the materials of choice in rigid fixation systems. (This chapter is limited to the discussion of nonresorbable fixation options.) Titanium is inert, nontoxic, corrosion resistant and has high tensile strength. Most commercial internal fixation systems contain commercially pure titanium or titanium alloy plates and screws of various dimensions and strengths. Two of the greatest benefits of titanium are its high strength-to-weight ratio and its corrosion resistance. Because it is nonferromagnetic (i.e., safe for future magnetic resonance imaging [MRI]) and resists all corrosion by bodily fluids, titanium has become and continues to be the implant material of choice for rigid fixation.
Osseointegration relies upon biocompatibility, and it plays a role in internal fixation. It allows bone to tolerate and stabilize metallic implants, such as screws. Titanium is one of the metals that promotes biocompatibility. Most plates are made from either commercially pure titanium or a titanium alloy consisting of mostly titanium and, to a lesser extent, a combination of aluminum, vanadium, nickel, chromium, iron, molybdenum, and niobium. Screws are usually made from commercially pure titanium, stainless steel, or a titanium alloy.
Principles of Fracture Healing
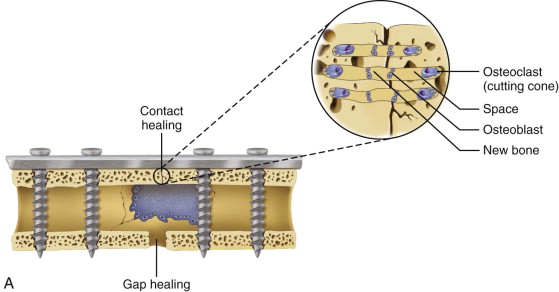
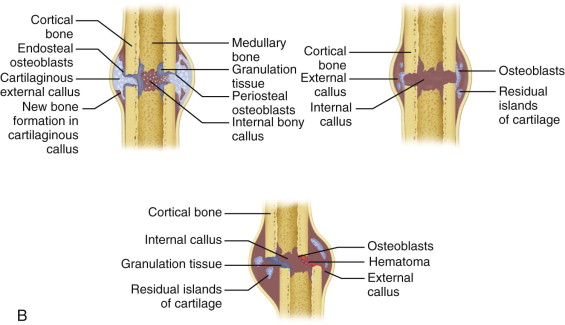
Mandibular bone is a composite of organic collagen and inorganic mineral. Mandibular collagen resists tensile forces, and the mineral component resists compressive forces. Throughout life, mandibular bone is constantly remodeling in response to the functional loads created by the muscles of mastication. In response to fracture, it heals by one of two processes: primary (contact or direct) healing or secondary (callus or gap) healing. An understanding of these processes will result in better treatment decisions ( Figure 62-2 ). Primary bone healing occurs when the fractured bone fragments are well reduced and then stabilized in a way that allows minimal fragment mobility, usually by using a rigid form of osteosynthesis. Primary healing occurs in areas of good bone contact by direct remodeling of the haversian system with direct crossing of osteoclasts and osteoblasts across the fracture plane, with no callus formation. In contrast, secondary bone healing with a callus occurs when some mobility remains between the fractured fragments; for instance, when a fractured mandible is treated by intermaxillary fixation alone or when there is a gap leaving mobility between fragments. No callus is formed in primary bone healing. Secondary healing typically occurs when a fracture hematoma between bone fragments remodels into a callus. The callus evolves from granulation tissue to connective tissue, followed by mineralized cartilage and eventually compact bone formation.
Zones of Osteosynthesis and Screw Depth
The concept of lines of mandibular osteosynthesis were introduced by Michelet et al and later popularized by Champy; this concept is used mostly in miniplate osteosynthesis. The lines represent regions of mandibular compressive or tensile forces, which can vary depending on muscle function and the location of the load. It can be helpful to conceptualize these lines of osteosynthesis as strong, thick areas of the mandible that resist functional stresses and that also make ideal locations to place screws and smaller plates (miniplates) in fracture repair. ( Figure 62-3 ).
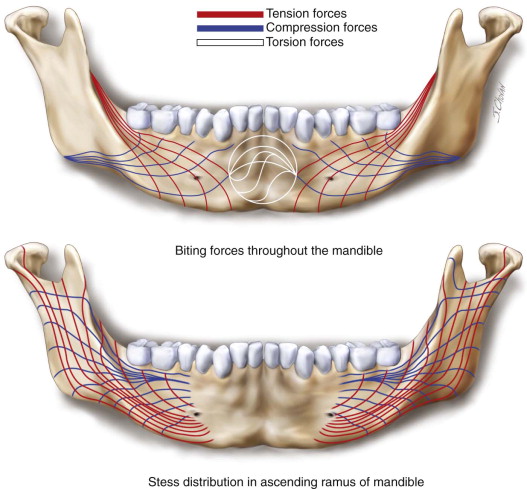
In fractures of the angle and posterior body, most loading is anterior to the fracture site; therefore, the superior border is usually under tensile forces, whereas the inferior border undergoes more compressive forces. In fractures of the symphyseal region, these forces alternate between the superior and inferior border. When the surgeon uses nonrigid fracture fixation, miniplates and screws are placed along the lines of mandibular osteosynthesis. When miniplates and monocortical screws are used, the weakest portion of the entire construct is usually the plate itself; therefore, bicortical screws are not advantageous in nonrigid fixation (i.e., in dense bone the miniplate will fail before the monocortical screws). When larger reconstruction plates and screws are used correctly, they can stabilize the jaw under any force, no matter where they are place along the mandible; however, because they gain additional durability when bicortical screws are used, they usually are placed along the inferior border to avoid tooth and nerve injury.
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


