Oral and maxillofacial surgery (OMFS) has undergone a renaissance/metamorphosis as a specialty and in the technologic innovations that have enhanced the surgical care of patients. This article reviews traditional maximal transoral approaches in the management of common pathologic lesions seen by OMFS, and compares these techniques with a literature review that applies minimally invasive technology and innovative robotic surgery (transoral robotic surgery) to treat similar lesions. The traditional approaches described in this article have transcended generations and future trends are suggested that will improve the training of the OMFS legacy as clinicians move forward in the care of patients.
Key points
- •
Over the past three decades oral and maxillofacial surgery (OMFS) has undergone a metamorphosis in terms of technology and surgical therapy.
- •
The conventional use of maximal surgery for wide transoral exposure has been challenged by the risks of postoperative morbidity, such as neurosensory deficits, loss of tissue, and reoperation for reconstruction.
- •
The application of minimally invasive endoscopic surgery has allowed the surgeon an opportunity to approach anatomy of the head and neck that was not previously visible in their surgical field.
- •
Transoral robotic surgery (TORS) shows great promise as a technologic tool in the training of oral and maxillofacial surgeons and more large clinical trials are needed to support its use as a standard of care.
- •
Future trends in surgical intervention should take advantage of the technology that can enhance the training of future surgeons, and the care of their patients.
Introduction
Within the last three decades oral and maxillofacial surgery (OMFS) has undergone a renaissance/metamorphosis as a specialty, and more importantly in the technologic innovations that have enhanced the surgical care of patients. As baby boomer surgeons, the authors admit that had they been exposed earlier to many of the new techniques described in this article, their surgical experience would have provided an opportunity to collect a greater number of outcomes data for OMFS-based practice standards.
The OMFS has been the leader of surgical approaches of the head and neck extraorally and intraorally, with the latter having advantages of less visible scarring, less tissue trauma, and maintenance of function and esthetics. Disadvantages, however, have included tissue trauma, neurosensory deficits, vascular compromise, edema, and difficulty in approaching deeper structures not often seen with the naked eye. Over the last 25 years, technology has enhanced the ability to deliver surgical care that minimizes the surgical morbidities mentioned previously. , This article reviews traditional maximal transoral approaches in the management of pathologic lesions see by the oral and maxillofacial surgeon, and compares these techniques with a literature review that applies minimally invasive technology and innovative robotic surgery (transoral robotic surgery [TORS]) to treat similar lesions. Future strategies are hypothesized that will improve the training of our legacy moving forward. This article is limited to a discussion of cystic and cancerous lesions and the reader is referred to other surgical approaches for head and neck pathology in this issue.
Traditional maximal surgery versus minimally invasive surgery in the management of intraoral cystic lesions
Traditional Maximal Surgical Intervention
The traditional approaches applied in OMFS are often referred to as maximally invasive because the surgical plan requires wide exposure and careful dissection to allow for complete extirpation of pathology. The traditional approaches for the removal of intraoral cysts follow an algorithm that consists of a series of steps beginning with diagnostic imaging in the three dimensions to determine the boundaries of dissection followed by aspiration to ensure a safe surgical approach and subsequent differential diagnosis. The latter then provides a choice of treatment alternatives resulting in either complete excision of the cyst or marsupialization and irrigation to enhance a metaplasia of cytoarchitecture followed by enucleation.
Maximal surgical techniques have their advantages and disadvantages. Approaches for total excision of large cysts may be problematic with postoperative complications including submucosal hematomas, wound dehiscence, infection, injury to tooth roots, paresthesia, increased risk of bleeding within adjacent neurovascular bundles, facial edema, unnecessary bone removal, oroantral fistula formation, and ultimately longer healing time. , Alternatively, maximal approaches offer better evaluation visually to avoid a second procedure. With respect to health care economics, open procedures are associated with increased postoperative pain, which leads to increased pain management costs, increased estimated blood loss, leading to a higher transfusion rate, and longer length of stay, all of which contributed to a higher direct cost. Indirect costs include a patient’s extended time away from work and disability-related expenses.
Minimally Invasive Surgical Intervention
Minimally invasive surgery, also referred to as endoscopic surgery, telescopic surgery, and/or less invasive surgery, had its origin from the work of Hunter and Sackler, the fathers of laparoscopic surgery. The work of McCain and colleagues , has blazed a trail for the use of this technology in order for the oral and maxillofacial surgeon to allow the naked eye an alternative technique to perform microscopic and macroscopic surgical intervention beyond boundaries that were previous exposed only with large incisions. Oral and maxillofacial surgeons can apply this technology in an effort to decrease patient postsurgical consequences, providing a bloodless surgery, and little trauma to surrounding anatomy. Access for intervention is smaller and distant to the area of interest and therefore less likely to cause injuries seen with larger access. As technology has grown, issues of instrument size and precision have made endoscopy more appealing and well accepted by practitioner and patient. Advantages include minimal morbidity, shorter hospital stay, a quicker return to premorbid function, and less postoperative discomfort. Miloro in his studies on treatment of subcondylar fractures with endoscopic methods showed shorter operating compared with traditional extraoral and intraoral approaches. The latter supports decreased length of hospital stay, minimal morbidity, and earlier return of the patient’s health-related quality of life.
Endoscopy has numerous other uses in the OMFS arena including trauma, obstructive salivary gland disease, maxillary sinus disease, temporomandibular disorders, and repair of neurosensory deficits caused by trauma of the trigeminal nerve. The learning curve for endoscopic surgery is steep and its success is predicated on the experience of the surgical team. It requires a well-seasoned primary endoscopic surgeon and an assistant to either help with the camera or manipulate the tissues for precise visualization. Fig. 1 depicts the armamentarium of a minimally invasive surgical instrument set up (Nexus CMF, Salt Lake City, UT).

Cases
The following cystic lesions are described using a maximal surgical approach by the authors and compared with a review of the literature that applies the use of a more minimally invasive surgical intervention. Each is discussed with respect to the surgical option, and the risks and benefits considered for successful patient outcomes.
Case 1: nasopalatine duct cyst
The nasopalatine duct cyst (NDC) is a benign nonodontogenic cyst arising from the nasopalatine duct with epithelial remnants that become traumatized and proliferate by mucus retention, trauma, and/or infection. The NDC is the most common nonodontogenic cyst in the maxilla occurring in approximately 1% of the population. Most NDC are asymptomatic and when presented in clinic patients may describe a swollen painful area below the nose, an ill-fitting prostheses in the anterior maxilla, drainage, and/or complaints of nasal obstruction. Imaging varies in appearance from a well-circumscribed radiolucency to a large diffuse pattern that can violate the floor of the nasal cavity.
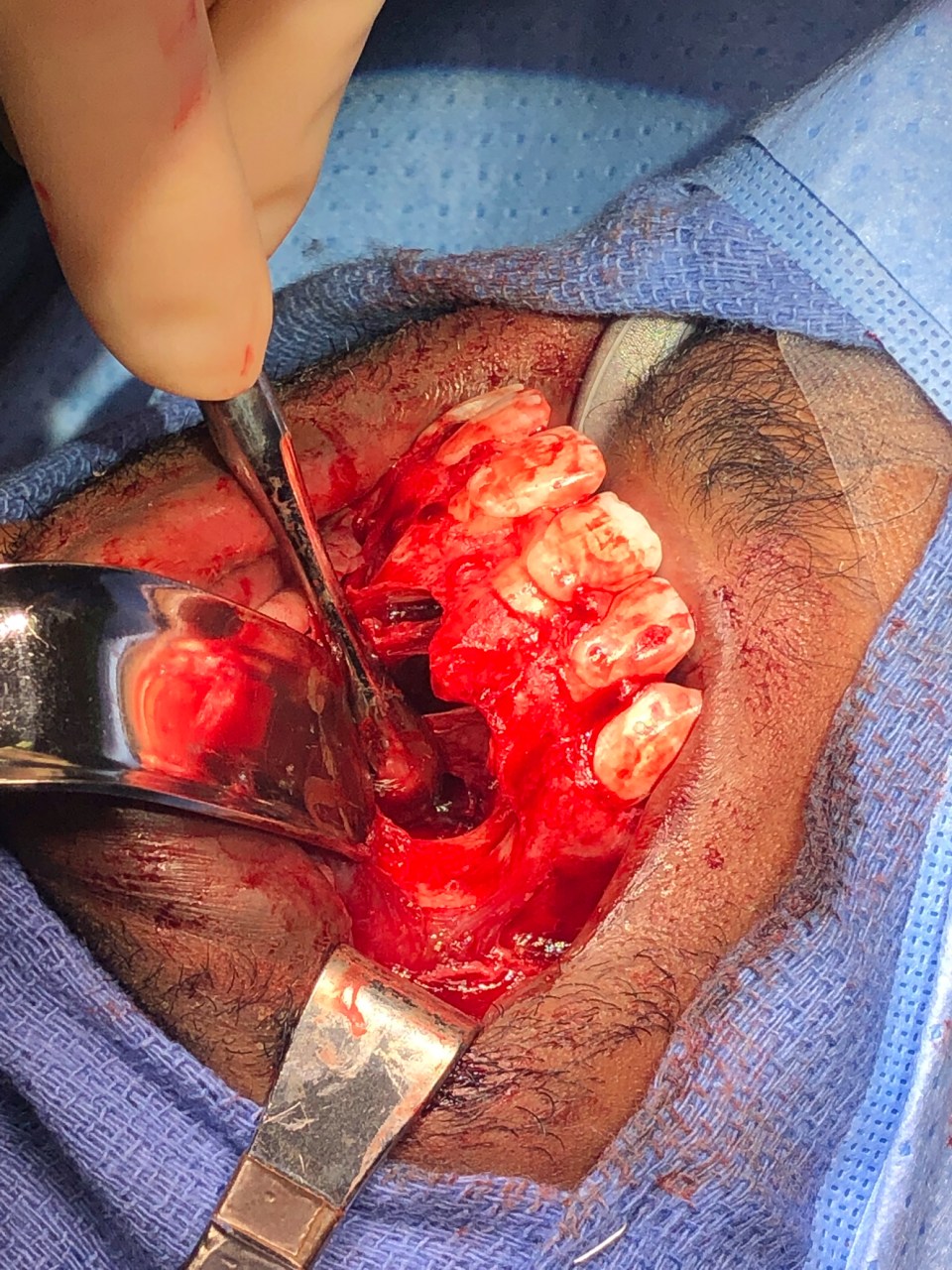
A 19-year-old man was referred to our oral surgery clinic at the University of Utah Medical Center with a complaint of a swelling in his anterior maxillary arch that was present for at least 6 months. He denied a history of trauma or bite by an insect or animal, and said it was just getting “bigger.” His medical and surgical histories were unremarkable. Laboratory values were within normal limits. Clinical evaluation depicted a facial deformity on frontal and lateral clinical positioning. Radiographic imaging with cone beam computed tomography revealed a large radiolucent lesion that extended bilaterally across his anterior maxilla ( Figs. 2 and 3 ) with a minimal degree of bony erosion of the enlarged cystic structure. Pulp testing of teeth #7, 8, 9, and 10 was performed and all exhibited vitality. The patient was taken to the operating room, nasotracheally intubated, and a traditional intraoral approach was performed with a sublabial excision that extended to a full-thickness flap because of the need for bilateral exposure to the floor of the nose for complete enucleation. The cyst was aspirated and a minimal amount of straw-colored fluid was removed. Figs. 4 and 5 depict the cyst on exposure followed by enucleation and measured 3.0 cm × 2.5 cm × 2.0 cm in total. We applied gauze packing to the resultant crater to help decrease the dead space that resulted from a presumptive effect of hydrostatic pressure. The patient healed unremarkably over a period of 3-week follow-up. No recurrence has been reported over a period of 24 months.



Most cases that are presented in the literature support extirpation of the NDC through a sublabial or palatine approach. Surgical enucleation is the treatment of choice with an extremely low recurrence rate. The alternative treatment modality of marsupialization is an acceptable alternative in select patients with large cystic spread into the nasal cavity. , Francoli and colleagues looked at 22 cases of NDC and suggested that the use of electroscapels may help to control hemostasis in these cases because the nasopalatine neurovascular bundle can precipitate significant bleeding during the dissection. The authors do support a direct transoral approach for enucleation. Disadvantages are a wide mucosal flap design; more bone removal; and the possibility of damage to neurovascular structures, tooth roots, and sinus mucosa. The latter is of concern because of occasional violation of the nasopalatine neurovascular bundle with resultant irreversible paresthesia of an anterior palate and associated tooth roots. These procedures as traditional approaches have resulted in rare recurrences with long-term follow-up. The authors, however, do recommend that even with full visualization during cyst removal, the surgeon is wise to follow up with postoperative imaging and yearly re-evaluation. Taken together a risk–benefit ratio is always of importance when offering the patient surgical options (see summary and conclusions).
The transoral maximal surgical approach described previously is circumvented through minimally invasive endoscopic marsupialization of the NDC. , Studies have supported the application of transnasal endoscopy in the treatment of odontogenic pathologies in the maxillary sinus because of its ability to improve patency of cysts for adequate drainage, and minimal violation of adjacent structures. , The visual system allows for a more precise approach and several authors recommend this as a first approach for treatment of oral surgical pathology before the need for a secondary maximal exposure. , , Wu and colleagues used transnasal endoscopic marsupialization as a salvage treatment of a large NDC that was treated several times prior using transoral surgical dissection. They reported a successful resolution of symptomatology 6 months after surgery. Other surgical studies support using a combination of transoral and endoscopic surgical intervention in resolving odontogenic pathologies. , , This option provides a one-time surgical entry, better illumination, and magnification and avoidance of violation of adjacent structures. , ,
Case 2: maxillary odontogenic cysts
Maxillary odontogenic and nonodontogenic lesions often expand into the maxillary sinus and surrounding midface anatomy. Cystic lesions with epithelial lined tracts can impede successful removal and increase the risk of morbidity to maxillary structure, and nasal structure and function. The traditional paradigms for surgical extirpation of maxillary odontogenic and nonodontogenic cysts based on the degree of spread have ranged from enucleation, curettage, maxillectomy, marsupialization, osteotomy, and removal of teeth. Extension of pathology often requires a second surgery to reconstruct large defects.
A 55-year-old woman was seen at the oral surgery clinic of the University of Utah complaining of a dull pain in her right posterior quadrant that was present for about 7 to 8 months. She denied a history of prior infection, trauma, or other dental problems. She denied any neurosensory deficits and denied observing purulence or “bad taste.” Teeth #2 and 3 were pulp tested and gave equivocal findings. The patient was concerned because of her past medical history of a brainstem stroke after surgery for a meningioma in her right frontotemporal lobe. She required a decompressive hemicraniectomy, which precipitated a brainstem stroke with left hemiplegia, spasticity, contractures, and several seizures. She has been followed every 6 to 12 months for the past 10 years with no exacerbations other than occasional seizure activity that is well-controlled by medications. An intraoral examination revealed dentition in fair repair except for the maxillary first molar in the upper right quadrant, which exhibited class 2+ mobility with minimal purulence on palpation. Further palpation superiorly revealed an expansion of the bony wall of the lateral right maxillary sinus. No neurosensory deficit was evident and the patient stated she felt minimal pressure when palpated with no pain. Radiographic imaging with cone beam computed tomography depicted a large radiopacity surrounding tooth #3 and extending through to the maxillary sinus. There was expansion of the bone with evidence of erosion into the sinus on coronal and sagittal view. The axial view showed significant buccal-lingual expansion without erosion into the palate. Both right and left maxillary sinuses appeared to exhibit radiopacities characteristic of a bilateral maxillary sinusitis ( Figs. 6 and 7 ).





