Preauricular Approach
The temporomandibular joint (TMJ) is situated in an area that is relatively easy to expose surgically, although the extent of exposure obtained is not much. The structure that limits the extent of exposure is the branching facial nerve.
SURGICAL ANATOMY
Although the TMJ itself is relatively small, there are many important anatomic structures near it. This region contains the parotid gland, superficial temporal vessels, and facial and auriculotemporal nerves.
Parotid Gland
The parotid gland lies below the zygomatic arch, below and in front of the external acoustic meatus, on the masseter muscle, and behind the ramus of the mandible. The superficial pole of the parotid gland lies directly on the TMJ capsule. The parotid gland itself is enclosed within a capsule derived from the superficial layer of the deep cervical fascia, frequently called the parotideomasseteric fascia.
Superficial Temporal Vessels
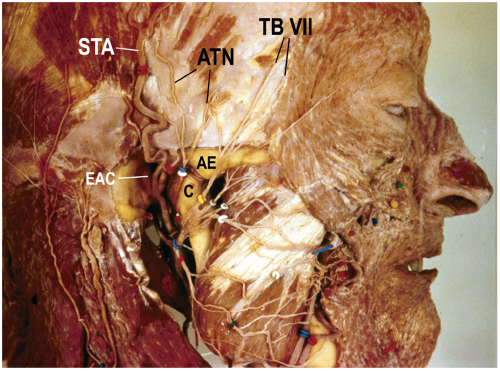
The superficial temporal vessels emerge from the superior aspect of the parotid gland and accompany the auriculotemporal nerve (see Fig. 12.1). The superficial temporal artery rises in the parotid gland by bifurcation of the external carotid artery (the other terminal artery is the internal maxillary). As it crosses superficial to the zygomatic arch, a temporal branch is given off just over the arch. This vessel is a common source of bleeding during surgery. The superficial temporal artery divides into the frontal and parietal branches a few centimeters above the arch. The superficial temporal vein lies superficial and usually posterior to the artery. The auriculotemporal nerve accompanies, and is posterior to, the superficial temporal artery.
Auriculotemporal Nerve
The auriculotemporal nerve innervates parts of the auricle, the external auditory meatus, the tympanic membrane, and the skin in the temporal area. It courses from the medial side of the posterior neck of the condyle and turns superiorly, running over the zygomatic root of the temporal bone (Fig. 12.1). Just anterior to the auricle, the nerve divides into its
terminal branches in the skin of the temporal area. Preauricular exposure of the TMJ area almost invariably injures this nerve. The damage is minimized by incising and dissecting in close apposition to the cartilaginous portion of the external auditory meatus, realizing that this structure runs somewhat anteriorly as it courses from lateral to medial. Temporal extension of the skin incision should be located posteriorly so that the main distribution of the nerve is dissected and retracted forward within the flap. Fortunately, patients rarely complain about sensory disturbances that result from damage to this nerve.
terminal branches in the skin of the temporal area. Preauricular exposure of the TMJ area almost invariably injures this nerve. The damage is minimized by incising and dissecting in close apposition to the cartilaginous portion of the external auditory meatus, realizing that this structure runs somewhat anteriorly as it courses from lateral to medial. Temporal extension of the skin incision should be located posteriorly so that the main distribution of the nerve is dissected and retracted forward within the flap. Fortunately, patients rarely complain about sensory disturbances that result from damage to this nerve.
Facial Nerve
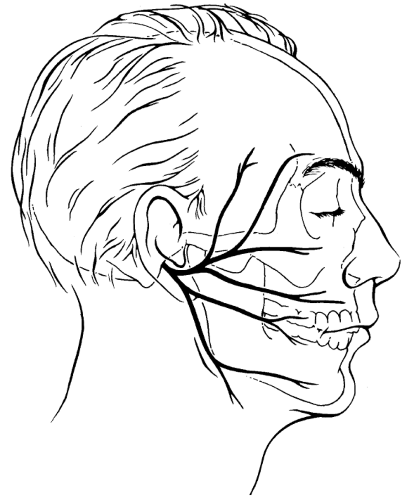
Shortly after the facial nerve exits the skull through the stylomastoid foramen, it enters the parotid gland. At this point, the nerve usually divides into two main trunks (temporofacial and cervicofacial), the branches of which variably anastomose to form a parotid plexus. The division of the facial nerve is located between 1.5 and 2.8 cm below the lowest concavity of the bony external auditory canal.
The terminal branches of the facial nerve emerge from the parotid gland and radiate anteriorly (Fig. 12.1). They are commonly classified as temporal, zygomatic, buccal, marginal mandibular, and cervical. The location of the temporal branches is of particular concern during TMJ surgery because these are the branches that are most likely to be damaged. As the temporal nerve branches (frequently two) cross the lateral surface of the zygomatic arch, they course along the undersurface of the temporoparietal fascia (see Fig. 6.5). The temporal branch crosses the zygomatic arch at varying locations in different individuals, and may be located anywhere from 8 to 35 mm (20 mm average) anterior to the external auditory canal
(see Fig. 12.2) (1). Therefore, the temporal branches of the facial nerve can be protected by incising through the superficial layer of temporalis fascia and periosteum of the zygomatic arch not more than 0.8 cm in front of the anterior border of the external auditory canal.
(see Fig. 12.2) (1). Therefore, the temporal branches of the facial nerve can be protected by incising through the superficial layer of temporalis fascia and periosteum of the zygomatic arch not more than 0.8 cm in front of the anterior border of the external auditory canal.
Temporomandibular Joint
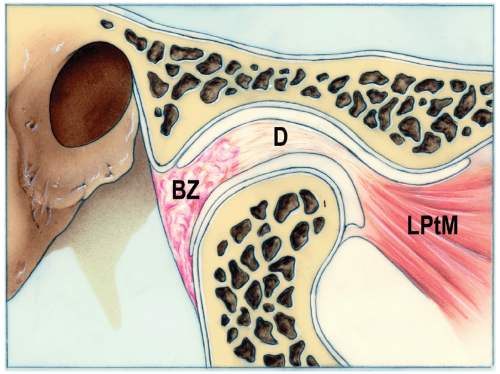
The TMJ capsule defines the anatomic and functional boundaries of the TMJ. The thin, loose fibrous capsule surrounds the articular surface of the condyle and blends with the periosteum of the mandibular neck. On the temporal bone, the articular capsule completely surrounds the articular surfaces of the eminence and fossa (see Fig. 12.3). The attachments of the capsule are firmly adhered to the bone. Anteriorly, the capsule attaches in front of the crest of the articular eminence; laterally, it adheres to the edge of the eminence and fossa; and posteriorly, it extends medially along the anterior lip of the squamotympanic and petrotympanic fissures. The medial attachment runs along the sphenosquamosal suture. The articular capsule is strongly reinforced laterally by the temporomandibular (lateral) ligament, composed of a superficial fan-shaped layer of obliquely oriented connective tissue fibers and a deeper, narrow band of fibers that run more horizontally. The ligament attaches broadly to the outer surface of the root of the zygomatic arch and converges downward and backward to attach to the back of the condyle below and behind its lateral pole.
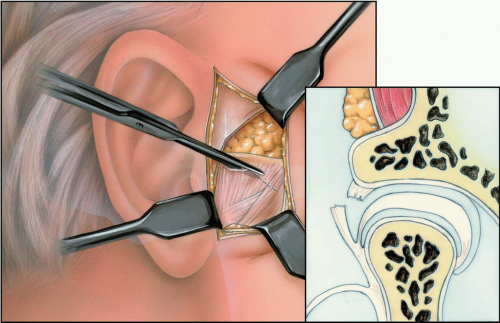
The articular disk is a firm but flexible structure with a biconcave shape (see Fig. 12.4). The disk is usually divided into three regions: the posterior band, the intermediate zone, and the anterior band. The central intermediate zone is considerably thinner (1 mm) than the posterior (3 mm) and anterior (2 mm) bands. The upper surface of the disk adapts to
the contours of the fossa and the eminence of the temporal bone, and the lower surface of the disk adapts to the contour of the mandibular condyle.
the contours of the fossa and the eminence of the temporal bone, and the lower surface of the disk adapts to the contour of the mandibular condyle.
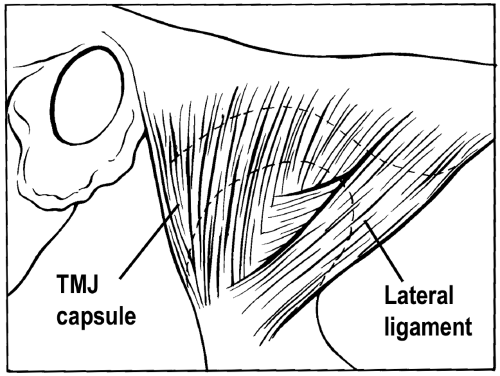
Figure 12.3 The temporomandibular joint (TMJ) capsule and lateral ligament. The lateral ligament has both oblique and horizontal components.
|
Posteriorly, the disk and the loosely organized posterior attachment tissues (i.e., bilaminar zone and retrodiscal pad) are contiguous. The retrodiscal tissue is a soft, areolar connective tissue with large vascular spaces. The posterior attachment tissues adhere to the tympanic plate of the temporal bone posterosuperiorly and to the neck of the condyle posteroinferiorly. Anteriorly, the disk, the capsule, and the fascia of the superior head of the lateral pterygoid muscle are contiguous. The superior head of the lateral pterygoid muscle may have some fibers inserting directly into the disk anteromedially.
The articular disk of the TMJ is a hypovascular intra-articular structure that separates the condylar head from the glenoid fossa. It is firmly attached to the condyle at its lateral pole; it
is not directly attached to the temporal bone. The articular disk and its posterior attachment tissues merge with the capsule around their periphery. The disk and its attachments divide the joint space into separate superior and inferior spaces. In the sagittal plane, the upper joint space is contiguous with the glenoid fossa and the articular eminence. The upper joint space always extends further anteriorly than the lower joint space. The lower joint space is contiguous with the condyle and extends only slightly anterior to the condyle along the superior aspect of the superior head of the lateral pterygoid muscle. In the frontal plane, the upper joint space overlaps the lower joint space. Therefore, dissection through the lateral capsule brings one into the superior compartment.
is not directly attached to the temporal bone. The articular disk and its posterior attachment tissues merge with the capsule around their periphery. The disk and its attachments divide the joint space into separate superior and inferior spaces. In the sagittal plane, the upper joint space is contiguous with the glenoid fossa and the articular eminence. The upper joint space always extends further anteriorly than the lower joint space. The lower joint space is contiguous with the condyle and extends only slightly anterior to the condyle along the superior aspect of the superior head of the lateral pterygoid muscle. In the frontal plane, the upper joint space overlaps the lower joint space. Therefore, dissection through the lateral capsule brings one into the superior compartment.
Layers of the Temporoparietal Region
The temporoparietal fascia is the most superficial fascial layer beneath the subcutaneous fat (see Fig. 12.5). This fascia is the lateral extension of the galea and is continuous with the superficial musculoaponeurotic system (SMAS) layer. It is frequently called the superficial temporal fascia or the suprazygomatic SMAS. It is easy to miss this layer completely when incising the skin because it is just beneath the surface. The blood vessels of the scalp, such as the superficial temporal vessels, run along its superficial aspect close to the subcutaneous fat. On the other hand, the motor nerves, such as the temporal branch of the facial nerve, run on the deep surface of the temporoparietal fascia.
The subgaleal fascia in the temporoparietal region is well developed and can be dissected as a discrete fascial layer if required, but it is generally used only as a cleavage plane in the standard preauricular approach.
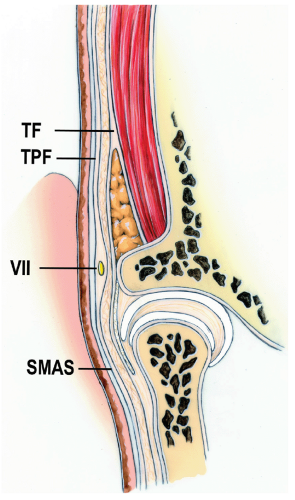
Figure 12.5 Coronal section of the temporomandibular joint (TMJ) region. TF, temporalis fascia (note that it splits inferior to this point into superficial and deep layers); TPF, temporoparietal fascia; VII, temporal branch of the facial nerve; SMAS, superficial musculoaponeurotic system.
Stay updated, free dental videos. Join our Telegram channel
VIDEdental - Online dental courses
 Get VIDEdental app for watching clinical videos
Get VIDEdental app for watching clinical videos

|