Abstract
Defining the ideal material for frontal sinus obliteration remains controversial. Autogenous cancellous bone is effective because of its biological properties: it undergoes fast revascularization acting as an active scaffold for bone healing, but is linked to additional donor site morbidity. Bone dust harvesting from the skull surface produces no sequelae but availability is limited. Many efforts have been made to overcome these drawbacks, and an ideal bone substitute sought. Demineralized Bone Matrix (DBX; Musculoskeletal Transplant Foundation, Edison, NJ, USA) is a commercially available product composed of demineralized bone particles reduced after proper processing of human bone in combination with sodium hyaluronate. It generates an osteoconductive surface and it is also a source of osteoinductive factors. Radiological follow-up using computed tomography is a very reliable method of following-up ossification and detecting the early signs of possible complications. The authors present their clinical series of postraumatic frontal sinus obliteration using a mixture of calvarial bone dust and DBX shell, with long-term radiological monitoring. The technique was demonstrated to be effective, reliable, stable in the long term and associated with minimal morbidity.
Frontal sinus fractures represent 2–12% of skull fractures and around 8% (5–15%) of all facial fractures according to different series. The high incidence of early and late complications means that complex frontal sinus fractures are prone to undergo surgical treatment in most cases. Posterior wall defects with nasofrontal duct involvement are the most common causes of intracranial complications.
Key points in frontal sinus fracture treatment include: the avoidance of residual dead space; prevention of possible continuous contamination of the intracranial space from the nasal cavity-ethmoidal cells; and the suppression of the natural tendency of the frontal sinus mucosa to proliferate in a pathological manner after sustaining trauma. Aggressive surgical techniques are proposed to prevent possible complications seeking a ‘one step’ resolution, including sinus obliteration.
Basic principles of frontal sinus obliteration have been developed over the last 50 years. This procedure has become one of the key points in the management of frontal sinus fracture treatment, chronic infection and benign tumours. Obliteration has been proved to reduce the risk of most common complications (mucocele, mucopyocele, osteomyelitis, meningitis and brain abscess).
The goal is to eliminate the sinus as a functional unit, avoiding epithelial regeneration. It is an alternative to more radical operations previously described as frontal sinus ‘exenteration’ (Reidel procedure, including removal of the anterior sinus wall and supraorbital ridges), or frontal sinus ablation (Killian procedure, similar to the previous one but preserving the supraorbital rim). Both procedures were associated with a high recurrence rate and significant cosmetic deformity.
The coronal approach allows excellent surgical access for the procedure and calvarial bone harvesting without additional morbidity. Best long-term results are obtained when obliteration is made with autogenous bone.
Alternative materials described for sinus obliteration are autogenous fat and muscle. Unlimited availability and no donor site morbidity make biomaterials a very attractive option for frontal sinus obliteration.
Inadequate frontal sinus fracture treatment may lead to serious complications even several years after the injury. Patients require long term clinical and radiological follow-up for early detection. Recurrent infection after sinus obliteration is usually associated with incomplete excision of the mucosa and inadequate nasofrontal duct sealing. The use of fat or muscle for obliteration may also facilitate infection as a result of a series of events starting with material resorption and creation of a dead space in the sinus cavity.
The objective of this article is to demonstrate that frontal sinus obliteration with autologous calvarial bone dust and demineralized bone matrix (DBX; Musculoskeletal Transplant Foundation, Edison, NJ, USA) is an effective and stable method, with minimal complications and morbidity. It prevents dead space formation and promotes effective nasofrontal duct sealing to prevent bacterial colonization. Long-term computed tomography (CT) monitoring facilitates early diagnosis of complications. In this paper the authors also discuss alternative materials used for obliteration.
Materials and methods
This is a prospective study including 18 patients with surgically treated frontal sinus fractures and a total of 30 sinus cavities obliterated with bone chips plus DBX at the authors’ department between 1 July 2005 and 1 July 2008.
Inclusion criteria for this study were: patients with acute traumatic pathology of the frontal sinus (anterior and/or posterior wall affected) with nasofrontal duct involvement, medically suitable for the proposed surgical procedure. Patients with isolated fractures of the anterior wall without involvement of the nasofrontal duct and severely comminuted/displaced fractures of the posterior wall requiring cranialization were excluded from this series.
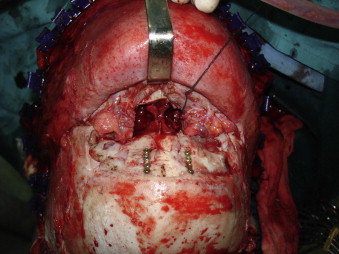
All patients were treated with the aim of preserving a safe non-functional frontal sinus through a bicoronal incision and subcranial approach. Surgical procedure included frontal sinus approach through the fractured anterior wall, excision of the sinus mucosa, sinus walls drilling, nasofrontal duct sealing, obliteration of the frontal sinus ( Fig. 1 ) and fixation of the fractured sinus walls.

If the existing anterior wall fracture did not allow adequate management of the sinus cavity, the approach was completed with an osteotomy of the anterior sinus wall (subcranial approach). Posterior wall fracture osteosynthesis was done if possible ( Fig. 2 ) to maintain the sinus as a barrier between the roof of the nasal cavities and the anterior cranial fossa.
Nasofrontal duct sealing was carried out either with fractured bone fragments or calvarial bone grafts.
In every patient, sinus obliteration was performed with skull bone dust and DBX. Autogenous bone dust was harvested from the exposed calvarial surface using a scraper device (Autogenous, Mozo-Grau Co. Valladolid, Spain). The bone was mixed with DBX in a 1/1 proportion, thus obtaining the necessary amount of filler material for sinus obliteration ( Fig. 3 ). Demineralized Bone Matrix (Musculoskeletal Transplant Foundation, Edison, NJ, USA) is a commercially available preparation (Synthes Company, PA, USA) of demineralized bone matrix particles reduced after proper processing of cadaveric human bone in combination with sodium hyaluronate.

After sinus obliteration, proper repositioning and fixation of the fractured or osteotomized anterior sinus wall was done with titanium miniplates and screws (1.3 mm). Titanium mesh was also used for anterior wall reconstruction in case of comminution ( Fig. 4 ).

Mean patient follow up was 36 months (range 24–60 months). Radiological follow-up was carried out with high resolution multi-slice CT scans (1 mm axial cuts) 6 and 24 months after surgery. Adequate sinus cavity filling and density were checked and measured in Hounsfield Units (HU) ( Fig. 5 ). HU represent tissue density. Blood and soft tissue present less than 80 HU, cancellous bone 150–400 HU, and cortical bone 400–750 HU. All studies were processed in an image workstation. ‘Extended brilliance workspace’ (Philips Medical Systems, USA) is an independent workstation providing various image processing tools and advanced reconstruction, analysis, reformatting, playback and archiving tasks. It allows processing of the digital imaging and communications in medicine (DICOM) data generated by the multislice CT and the production of multiplanar and three-dimensional reconstructions.

Results
Bilateral sinus obliteration was carried out in 12 patients; 6 underwent a unilateral procedure. 15 patients were male (83.3%) and 3 female (16.7%). The age range was 15–69 years (average 36 years).
The most common mechanism of injury was a direct high energy impact in the frontal bone in a motor vehicle accident. The most usual fracture pattern was a bilateral, displaced anterior wall associated with non-displaced posterior wall fracture (44.4%), followed by bilateral fractures with displacement of both anterior and posterior walls (22.2%). Other patterns included unilateral fractures with displacement of the anterior wall and posterior linear fracture (16.7%) and unilateral fractures with displacement of both anterior and posterior walls (16.7%).
Mean hospitalization time was 13 days (including intensive care unit stay). There was no perioperative mortality.
6 patients (33%) developed complications. All occurred at an early stage (within 6 months of treatment) and none were related to the material used for sinus obliteration. Three patients presented persistent frontal pain controlled with basic analgesic treatment. Two patients with comminuted fractures showed mild cosmetic deformity: one underwent reoperation with frontal cranioplasty and the other refused additional surgical treatment. The last complication was frontoorbital cellulitis, treated initially with intravenous antibiotics and later by surgical removal of the osteosynthesis material.
Radiological CT scans from the 30 obliterated sinuses (obtained 6 and 24 months after surgery) were analyzed to assess bone density and complications. No radiological evidence of sinus inflammatory disease or mucocele/mucopyocele was found in any case.
Sinusal radiopacity was significantly higher in the studies carried out 24 months postoperatively ( Figs. 6 and 7 ). Trabecular bone was found in the short-term studies (mostly peripherally), the bone became more cortical in the long-term follow up (with a significant progression in the amount of new bone formation). There was a positive correlation between bone density and the radiopacity achieved in relation to postoperative time. Ossification after sinus obliteration with bone chips and DBX shell occurred centripetally, starting from the sinus walls into the deep part of the sinus cavity. Average sinus bone density was 158.6 ± 60.06 HU at 6 months and 514.99 ± 178.38 HU at 24 months ( Table 1 ).




