Introduction
In orthodontics, adding restorative materials on occlusal or lingual surfaces is a common method to create a mini-biteplane to increase patients’ vertical dimension temporarily to facilitate several treatment procedures. However, this method transmits excessive occlusal forces through the periodontal ligament and causes trauma. In this prospective randomized clinical trial, we measured and compared quantitatively the volumes of root resorption after 4 weeks of occlusal trauma.
Methods
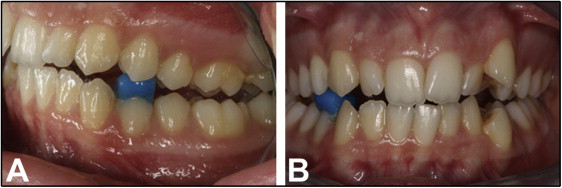
Forty-eight maxillary and mandibular first premolars of 12 patients (6 girls, 6 boys) comprised the sample for this study. One side of each patient was randomly selected as the control. On the contralateral side, a light-cured glass ionomer cement (Transbond Plus Light Cure Band Adhesive; 3M Unitek, Monrovia, Calif) was bonded onto the occlusal surface of the mandibular first premolar so that the cement was in contact with the maxillary first premolar. After 4 weeks, both first premolars were extracted. Each sample was imaged using a microcomputed tomography system (1172; SkyScan, Aartselaar, Belgium) and analyzed with specially designed software for volumetric measurements of resorption craters. Furthermore, pain was evaluated with a visual analog scale for 7 days.
Results
There were significant differences in the amounts of root resorption between the control and the experimentally traumatized teeth. No significant difference among the buccal, lingual, mesial, and distal surfaces was found in either jaw. Furthermore, no significant difference existed in the amount of root resorption among the cervical, middle, and apical thirds of both jaws. There was no correlation between age, sex, volume of the root resorption craters, and pain.
Conclusions
Restorative buildups, used to increase the vertical dimension by 2 mm for 4 weeks, caused root resorption along the sides of the teeth during the active bite-increase period.
It has been documented that external root resorption can result from excessive occlusal force when there is severe occlusal trauma. This occurs after the periodontium has lost its capacity to contain the force, resulting in alveolar bone loss and in some cases root resorption. Premature contact in centric occlusion and lateral excursive movements are common etiologies of occlusal trauma. Bruxing activity as a result of premature contact can exacerbate the root resorption process. It has also been suggested that excessive fremitus from occlusal trauma could be attributed to the resorption of the root apex after the adaptive capacity of the periodontium is exceeded.
The severity and type of trauma are also important factors related to root resorption. Intrusive trauma was defined as one of the most serious types of trauma related to root resorption and can lead to severe root resorption and ankylosis. It was demonstrated that after intrusive trauma, external resorption was encountered in 54.8% of the teeth, and all teeth with closed root apices lost their vitality.
In orthodontics, adding restorative materials on the occlusal or lingual surfaces is a common method to create a mini-biteplane to increase patients’ vertical dimensions temporarily to facilitate several treatment procedures. However, this method transmits excessive occlusal forces through the periodontal ligament and causes trauma. Unlike intrusion mechanics, force vectors cannot be easily controlled by orthodontists with these types of mini-biteplanes; therefore, their effect might be more deleterious than intrusive mechanics.
To date, the effect of trauma caused by orthodontic occlusal buildups on root resorption has not been investigated.
The aim this study was to evaluate the amount of root resorption after 4 weeks of occlusal trauma on the maxillary and mandibular premolars caused by restorative buildups. The null hypothesis was that there is no difference in the extent of root resorption between the control and experimental teeth.
Material and methods
Forty-eight maxillary and mandibular first premolars of 12 patients (6 girls, 6 boys; average chronologic age, 14.75 ± 2.09 years) who required bilateral extractions as part of their orthodontic treatment comprised the sample for this study. Ethics approval was obtained from the human ethics committee at the University of Bulent Ecevit in Zonguldak, Turkey (2009/06). The study protocol was explained to all patients and their parents. Written and verbal informed consent was obtained from the patients and their parents or guardians. The selection criteria for this study were (1) no previous reported or observed dental treatment to the teeth to be extracted, (2) no previous reported or observed trauma to the teeth to be extracted, (3) no previous reported or observed orthodontic treatment involving the teeth to be extracted, (4) no past or present signs or symptoms of periodontal disease, (5) no past or present signs or symptoms of bruxism, (6) no significant medical history that would affect the dentition, (7) no physical abnormality in the anatomy of the craniofacial or dentoalveolar complex, and (8) completed apexification.
Before the study, routine orthodontic records (extraoral and intraoral photographs, orthopantomography, lateral cephalometric films, orthodontic plaster casts, and periapical radiographs of the maxillary and mandibular first premolars) were collected from all patients.
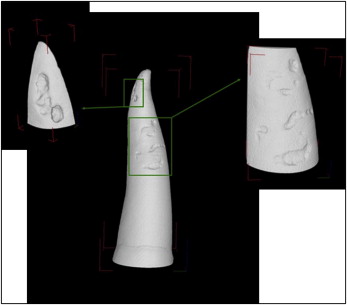
One side of each patient was randomly selected as the control. On the contralateral side, a light-cured glass ionomer cement (Transbond Plus Light Cure Band Adhesive; 3M Unitek, Monrovia, Calif) was bonded onto the occlusal surface of the mandibular first premolar so that the cement was in contact with the maxillary first premolar. The thickness of this cement was adjusted to 2 mm between the buccal cusp tips of both first premolars ( Fig 1 ). After 4 weeks, all first premolars were extracted. Extractions were performed to prevent any forceps contact to the cervical cementum. Immediately after extraction, the teeth were sterilized and stored in individual containers containing sterilized deionized water (Milli Q; Millipore, Bedford, Mass) that was sufficient to immerse the entire tooth at an ambient room temperature of 23°C ± 1°C until due for testing. All samples were scanned with a desktop x-ray microtomograph (1172; SkyScan, Aartselaar, Belgium) at the Australian Center for Microscopy and Microanalysis. All samples were scanned from the cementoenamel junction to the root apex with a resolution of 17.2 μm and a rotation step of 0.3°. The x-ray beams were generated at a voltage of 60 kV and 150 mA. After scanning, all radiographs were saved as 16-bit tagged image file format (TIFF) files. NRecon software (version 1.4.2; SkyScan) was used to transform these shadow images into a 3-dimensional cone-beam reconstruction algorithm. VG Studio Max software (version 1.2.1; Volume Graphics, Heidelberg, Germany) was used to visualize the samples and isolate the root resorption craters ( Fig 2 ). Each root resorption lesion was classified according to its vertical (cervical, medial, and apical) and axial (buccal, lingual, mesial, distal) locations. Isolated crater images were processed with 2-dimensional software (Chull 2D; University of Sydney, Sydney, NSW, Australia), and the total volume of each root resorption crater was calculated. All measurements were made by the same blinded researcher (F.C.). During the first 7 days of the experimental period, the patients were also given a form to record their pain on a visual analog scale.
Statistical analysis
The Wilcoxon signed rank test was used for the comparison of root resorption values between the trauma and control groups, and between the maxilla and the mandible ( P <0.05). The Friedman ( P <0.05) and Wilcoxon ( P <0.0083) tests were applied to determine the significant differences among the root surfaces and the vertical thirds. The Pearson correlation coefficient was used to evaluate possible correlations between age, sex, volume of the root resorption craters, and pain.
Results
The mean volumes of resorption per tooth in the control group were 11.881 × 10 −3 mm 3 and 7.3 × 10 −3 mm 3 on the maxillary and mandibular premolar roots, respectively. The experimental sides of the maxillary and mandibular premolars had 81.230 × 10 −3 mm 3 and 93.017 × 10 −3 mm 3 of root resorption on average, respectively ( Fig 3 , Table I ). The mean differences between the experimental and control groups were 6.83-fold in the maxillary premolars and 12.74-fold in the mandibular premolars. There were significant differences in the amount of root resorption between the control and experimentally traumatized teeth ( Table I ).
| Control | Trauma | P | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Minimum | Maximum | Mean | SE | SD | Minimum | Maximum | Mean | SE | SD | ||
| Maxillary | |||||||||||
| Total | 0.0 | 111.478 | 11.881 | 9.142 | 31.667 | 0.0 | 341.262 | 81.230 | 30.962 | 107.255 | 0.0500 ∗ |
| Buccal | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 048.122 | 7.669 | 4.705 | 16.299 | 0.0431 ∗ |
| Lingual | 0.0 | 4.727 | 0.418 | 0.392 | 1.359 | 0.0 | 93.782 | 11.920 | 7.769 | 26.911 | 0.0277 ∗ |
| Mesial | 0.0 | 111.478 | 9.879 | 9.255 | 32.060 | 0.0 | 169.766 | 27.180 | 15.045 | 52.117 | 0.0593 |
| Distal | 0.0 | 12.822 | 1.584 | 1.063 | 3.683 | 0.0 | 294.422 | 34.461 | 24.032 | 83.251 | 0.0382 ∗ |
| Cervical | 0.0 | 12.822 | 1.740 | 1.083 | 3.752 | 0.0 | 161.793 | 23.337 | 14.573 | 50.482 | 0.2135 |
| Middle | 0.0 | 106.960 | 9.897 | 8.853 | 30.667 | 0.0 | 292.250 | 41.979 | 24.085 | 83.433 | 0.0409 ∗ |
| Apical | 0.0 | 1.628 | 0.245 | 0.166 | 0.576 | 0.0 | 56.553 | 15.914 | 6.051 | 20.963 | 0.0077 † |
| Mandibular | |||||||||||
| Total | 0.0 | 44.596 | 7.300 | 4.530 | 15.693 | 0.0 | 295.511 | 93.017 | 29.146 | 100.963 | 0.0033 † |
| Buccal | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 55.831 | 9.093 | 4.589 | 15.898 | 0.0180 ∗ |
| Lingual | 0.0 | 1.496 | 0.165 | 0.127 | 0.438 | 0.0 | 35.591 | 5.777 | 2.991 | 10.363 | 0.0425 ∗ |
| Mesial | 0.0 | 44.581 | 3.724 | 3.714 | 12.867 | 0.0 | 116.139 | 22.840 | 10.504 | 36.387 | 0.0469 ∗ |
| Distal | 0.0 | 36.481 | 3.411 | 3.023 | 10.471 | 0.0 | 220.651 | 55.306 | 22.799 | 78.978 | 0.0173 ∗ |
| Cervical | 0.0 | 3.877 | 0.323 | 0.323 | 1.119 | 0.0 | 137.788 | 34.368 | 13.287 | 46.026 | 0.0117 ∗ |
| Middle | 0.0 | 44.596 | 3.849 | 3.705 | 12.834 | 0.0 | 201.795 | 35.109 | 16.974 | 58.798 | 0.0164 ∗ |
| Apical | 0.0 | 36.481 | 3.128 | 3.033 | 10.508 | 0.0 | 187.483 | 23.540 | 15.166 | 52.537 | 0.0663 |
There was no statistically significant difference in the amount of root resorption between the jaws in the experimental and control groups ( Table II ). In all groups, there was no significant difference among the buccal, lingual, mesial, and distal surfaces of the roots ( Table III ). In the control group, the buccal surfaces of the roots in both the maxillary and mandibular premolars were observed as resorption-free areas. The distribution of the root resorption lesions on the root surfaces is shown in Figure 4 .
| Mandible | Maxilla | P | |||||
|---|---|---|---|---|---|---|---|
| Mean | SE | SD | Mean | SE | SD | ||
| Control | |||||||
| Total | 11.881 | 9.142 | 31.667 | 7.300 | 4.530 | 15.693 | 0.6297 |
| Buccal | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 1.0000 |
| Lingual | 0.418 | 0.392 | 1.359 | 0.165 | 0.127 | 0.438 | 0.5899 |
| Mesial | 9.879 | 9.255 | 32.060 | 3.724 | 3.714 | 12.867 | 0.9774 |
| Distal | 1.584 | 1.063 | 3.683 | 3.411 | 3.023 | 10.471 | 0.9774 |
| Cervical | 1.740 | 1.083 | 3.752 | 0.323 | 0.323 | 1.119 | 0.3186 |
| Middle | 9.897 | 8.853 | 30.667 | 3.849 | 3.705 | 12.834 | 0.9323 |
| Apical | 0.245 | 0.166 | 0.576 | 3.128 | 3.033 | 10.508 | 0.7987 |
| Trauma | |||||||
| Total | 81.230 | 30.962 | 107.255 | 93.017 | 29.146 | 100.963 | 0.6707 |
| Buccal | 7.669 | 4.705 | 16.299 | 9.093 | 4.589 | 15.898 | 0.4095 |
| Lingual | 11.920 | 7.769 | 26.911 | 5.777 | 2.991 | 10.363 | 0.8874 |
| Mesial | 27.180 | 15.045 | 52.117 | 22.840 | 10.504 | 36.387 | 0,8874 |
| Distal | 34.461 | 24.032 | 83.251 | 55.306 | 22.799 | 78.978 | 0.7987 |
| Cervical | 23.337 | 14.573 | 50.482 | 34.368 | 13.287 | 46.026 | 0.2913 |
| Middle | 41.979 | 24.085 | 83.433 | 35.109 | 16.974 | 58.798 | 0.6297 |
| Apical | 15.914 | 6.051 | 20.963 | 23.540 | 15.166 | 52.537 | 0.9323 |
| Control | P | Trauma | P | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | SD | Mean | SE | SD | |||
| Maxillary | ||||||||
| Buccal | 0.0 | 0.0 | 0.0 | 0.2839 | 7.669 | 4.705 | 16.299 | 0.0398 ∗ |
| Lingual | 0.418 | 0.392 | 1.359 | 11.920 | 7.769 | 26.911 | ||
| Mesial | 9.879 | 9.255 | 32.060 | 27.180 | 15.045 | 52.117 | ||
| Distal | 1.584 | 1.063 | 3.683 | 34.461 | 24.032 | 83.251 | ||
| Mandibular | ||||||||
| Buccal | 0.0 | 0.0 | 0.0 | 0.1586 | 9.093 | 4.589 | 15.898 | 0.0579 |
| Lingual | 0.165 | 0.127 | 0.438 | 5.777 | 2.991 | 10.363 | ||
| Mesial | 3.724 | 3.714 | 12.867 | 22.840 | 10.504 | 36.387 | ||
| Distal | 3.411 | 3.023 | 10.471 | 55.306 | 22.799 | 78.978 | ||
∗ Wilcoxon test did not show significant difference among root surfaces ( P <0.0083).
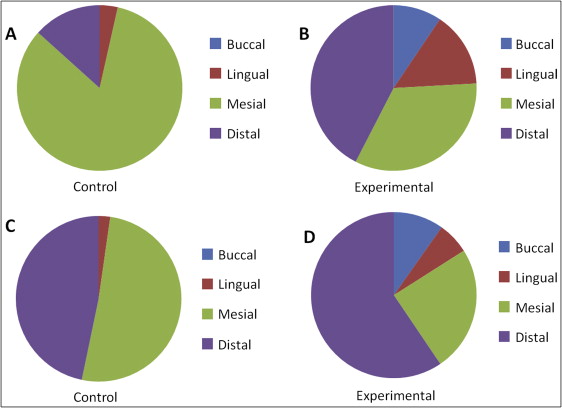
There was no significant difference in the amount of resorption among the cervical, middle, and apical thirds of the roots in either jaw, or between the control and experimental groups ( Table IV ). The distribution of resorption in the thirds of the root is shown in Figure 5 .
| Control | P | Trauma | P | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | SE | SD | Mean | SE | SD | |||
| Maxillary | ||||||||
| Cervical | 1.740 | 1.083 | 3.752 | 0.4169 | 23.337 | 14.573 | 50.482 | 0.1593 |
| Middle | 9.897 | 8.853 | 30.667 | 41.979 | 24.085 | 83.433 | ||
| Apical | 0.245 | 0.166 | 0.576 | 15.914 | 6.051 | 20.963 | ||
| Mandibular | ||||||||
| Cervical | 0.323 | 0.323 | 1.119 | 0.3499 | 34.368 | 13.287 | 46.026 | 0.7515 |
| Middle | 3.849 | 3.705 | 12.834 | 35.109 | 16.974 | 58.798 | ||
| Apical | 3.128 | 3.033 | 10.508 | 23.540 | 15.166 | 52.537 | ||
Stay updated, free dental videos. Join our Telegram channel

VIDEdental - Online dental courses


